Back
Neonatal General
Category: Abstract Submission
Neonatology General 9: Congenital Anomalies - CV
300 - Clinical Correlates, Diagnosis, and Management of Sleep-disordered Breathing in Young Children with Down Syndrome
Monday, April 25, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 300
Publication Number: 300.441
Publication Number: 300.441
Katelyn M. Seither, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Kristen Suhrie, Indiana University School of Medicine, Indianapolis, IN, United States; Benjamin M. Helm, Indiana University School of Medicine, Indianapolis, IN, United States; Daniel T. Swarr, Cincinnati Children's Hospital Medical Center, Liberty Township, OH, United States; Christine H. Heubi, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States
- KS
Kristen Suhrie, MD (she/her/hers)
Faculty
Riley Hospital for Children
Indianapolis, Indiana, United States
Presenting Author(s)
Background: Individuals with Down syndrome (DS) have high rates of sleep-disordered breathing and demonstrate more severe manifestations of obstructive sleep apnea (OSA) compared with non-syndromic patients. The consequences of untreated OSA in childhood include pulmonary hypertension, cognitive dysfunction, and abnormal growth. The American Academy of Pediatrics recommends that children with DS have a sleep study by age four years. It is unclear if these guidelines are sufficient to address the burden of disease in very young patients. There is also a paucity of data regarding clinical characteristics associated with OSA and outcomes following medical or surgical intervention in this population.
Objective: To describe the use of polysomnography (PSG) and associated findings in patients with Down syndrome in infancy and early childhood, to identify comorbidities and outcomes associated with OSA, and to evaluate the effectiveness of medical and surgical interventions.
Design/Methods: A retrospective cohort study was performed at Cincinnati Children’s Hospital Medical Center for all children with DS born between 2013-2019. Electronic medical record data were extracted including demographics, use of PSG, incidence of OSA, age at diagnosis, OSA severity, and interventions utilized. Statistical analysis used Fishers exact tests, ANOVA, and multinomial logistic regression analysis with a significance threshold of p < 0.05.
Results: A total of 397 patients met inclusion criteria and 235 (59%) had a sleep study. Most patients (94%) had an abnormal PSG and 60% had moderate or severe disease. There was an inverse relationship between age at first sleep study and OSA severity (p < 0.001). All sleep studies obtained in the first month of life (n=26) were abnormal with 70% classified as severe. Most patients (82%) had a sleep study due to the presence of symptoms; among asymptomatic patients, 91% met polysomnographic criteria for OSA. OSA severity was associated with increased rates of failure to thrive (p < 0.01), aspiration (p < 0.01), G-tube feeding (p < 0.05), and pulmonary hypertension (p < 0.01). Most patients (79%) required multiple interventions to manage their OSA.Conclusion(s): In this cohort of infants and young children with DS who underwent PSG, a majority had moderate to severe OSA. The pervasiveness of severe disease in young infants suggests that current surveillance guidelines are inadequate. Infants should be evaluated with PSG in the first 6 months of life regardless of clinical symptoms. Further study is needed to prospectively evaluate the impact of early diagnosis and intervention on long term outcomes.
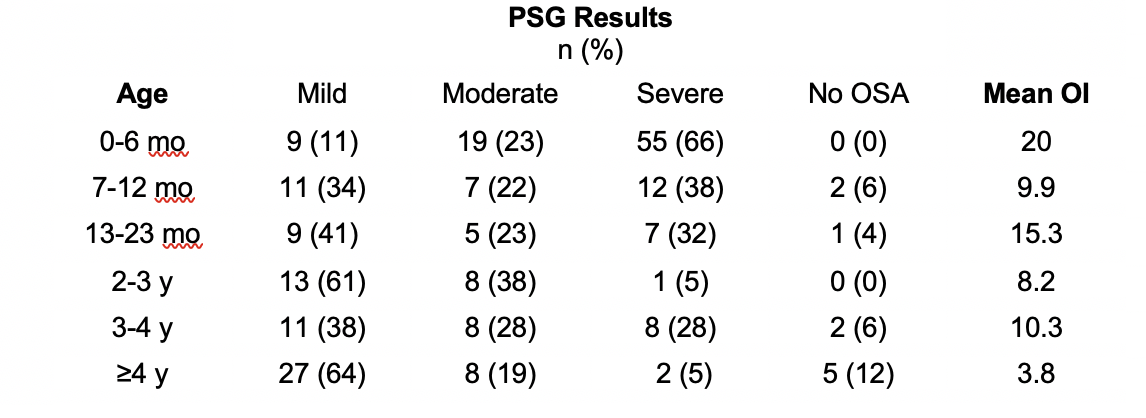
OSA Severity by Age at First Sleep Study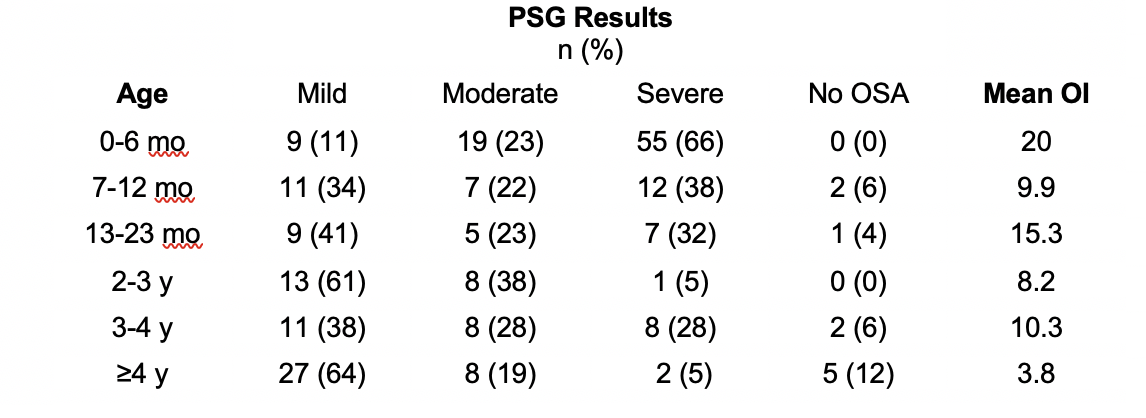
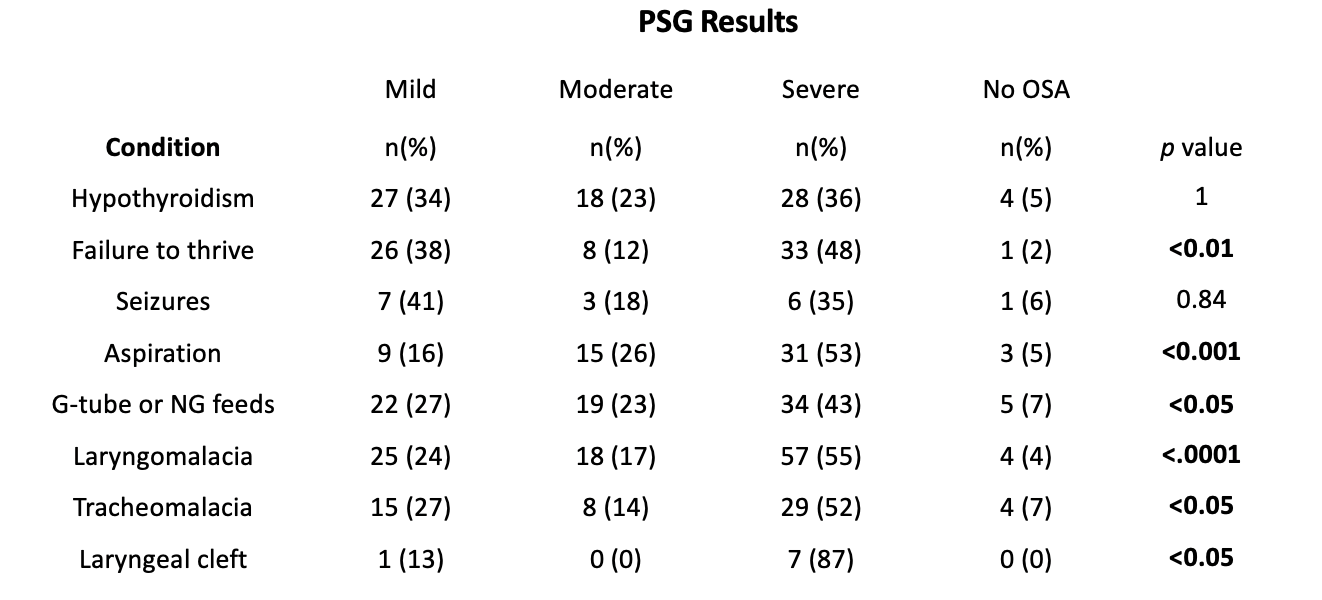
Comorbidities Associated with OSA Severity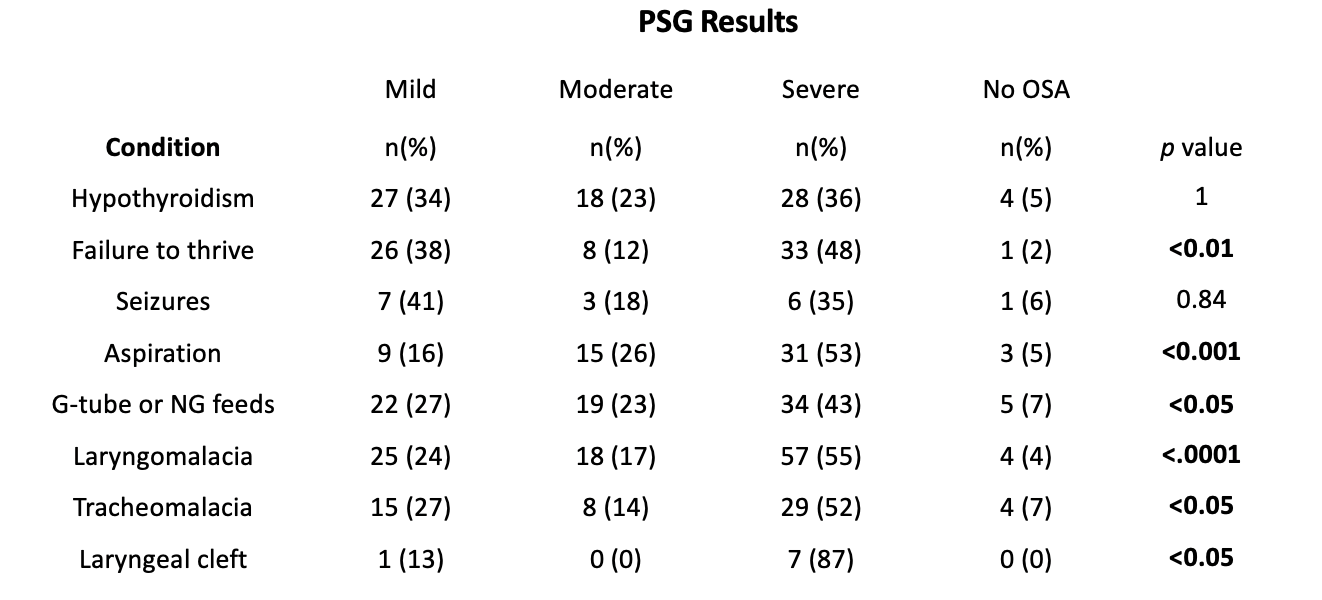
Objective: To describe the use of polysomnography (PSG) and associated findings in patients with Down syndrome in infancy and early childhood, to identify comorbidities and outcomes associated with OSA, and to evaluate the effectiveness of medical and surgical interventions.
Design/Methods: A retrospective cohort study was performed at Cincinnati Children’s Hospital Medical Center for all children with DS born between 2013-2019. Electronic medical record data were extracted including demographics, use of PSG, incidence of OSA, age at diagnosis, OSA severity, and interventions utilized. Statistical analysis used Fishers exact tests, ANOVA, and multinomial logistic regression analysis with a significance threshold of p < 0.05.
Results: A total of 397 patients met inclusion criteria and 235 (59%) had a sleep study. Most patients (94%) had an abnormal PSG and 60% had moderate or severe disease. There was an inverse relationship between age at first sleep study and OSA severity (p < 0.001). All sleep studies obtained in the first month of life (n=26) were abnormal with 70% classified as severe. Most patients (82%) had a sleep study due to the presence of symptoms; among asymptomatic patients, 91% met polysomnographic criteria for OSA. OSA severity was associated with increased rates of failure to thrive (p < 0.01), aspiration (p < 0.01), G-tube feeding (p < 0.05), and pulmonary hypertension (p < 0.01). Most patients (79%) required multiple interventions to manage their OSA.Conclusion(s): In this cohort of infants and young children with DS who underwent PSG, a majority had moderate to severe OSA. The pervasiveness of severe disease in young infants suggests that current surveillance guidelines are inadequate. Infants should be evaluated with PSG in the first 6 months of life regardless of clinical symptoms. Further study is needed to prospectively evaluate the impact of early diagnosis and intervention on long term outcomes.
OSA Severity by Age at First Sleep Study
Comorbidities Associated with OSA Severity