Endocrinology: Type 2 Diabetes (T2 DM)
Category: Abstract Submission
Endocrinology I
518 - A non-obese diabetes mouse model born with small-for-gestational age
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 518
Publication Number: 518.107
Publication Number: 518.107
Nobuhiko Nagano, Department of Pediatrics and Child Health, Nihon University School of Medicine, Tokyo, Tokyo, Japan; Daichi Katayama, Department of Pediatrics and Child Health, Nihon University School of Medicine, Toky, tokyo, Tokyo, Japan; Kimitaka Nakazaki, Department of Pediatrics and Child Health, Nihon University School of Medicine, Tokyo, itabashiku, Tokyo, Japan; Shoichi Shimizu, Department of Pediatrics and Child Health, Nihon University School of Medicine, Itabashi, Tokyo, Japan; Tomoo Okada, Kanagawa institute of technology, ATSUGI, Kanagawa, Japan; Tatsuhiko Urakami, Nihon University School of Medicine, Itabashi, Tokyo, Japan; Ichiro Morioka, Nihon University School of Medicine, Itabashi, Tokyo, Japan
.jpg)
Daichi Katayama, no
graduate student
Nihon University Itabashi Hospital
meguro, Tokyo, Japan
Presenting Author(s)
Background: When experiencing undernutrition in utero, a neonate can be born with low birthweight and be at high risk of developing lifestyle-related diseases such as diabetes. Traditional diabetic animal models employ a high-fat diet to induce obesity have been established. However, in clinical practice, patients can develop diabetes without significant postnatal obesity, but were born small-for-gestational age (SGA), but such animal models have not been developed as yet.
Objective: To develop an adult non-obese diabetic mouse model using intrauterine ischemia to induce SGA in order to study the pathogenesis of hyperglycemia.
Design/Methods: This study was conducted with the approval of our animal ethics committee. At E16.5, intrauterine ischemia, where blood flow in both uterine arteries is blocked for 15 min, was performed in a subgroup of pregnant mice (I). Non-occluded dams were used as sham controls (C). After birth, female pups from each group were weaned at 4 wks of age and bred at 8 wks of age (n=7 for each group). Fasting blood glucose levels, serum insulin (IRI) concentrations, and homeostasis model assessment of insulin resistance (HOMA-R) were compared at 8 wks of age. Metabolite analyses were then performed on the liver tissues at 8 wks of age.
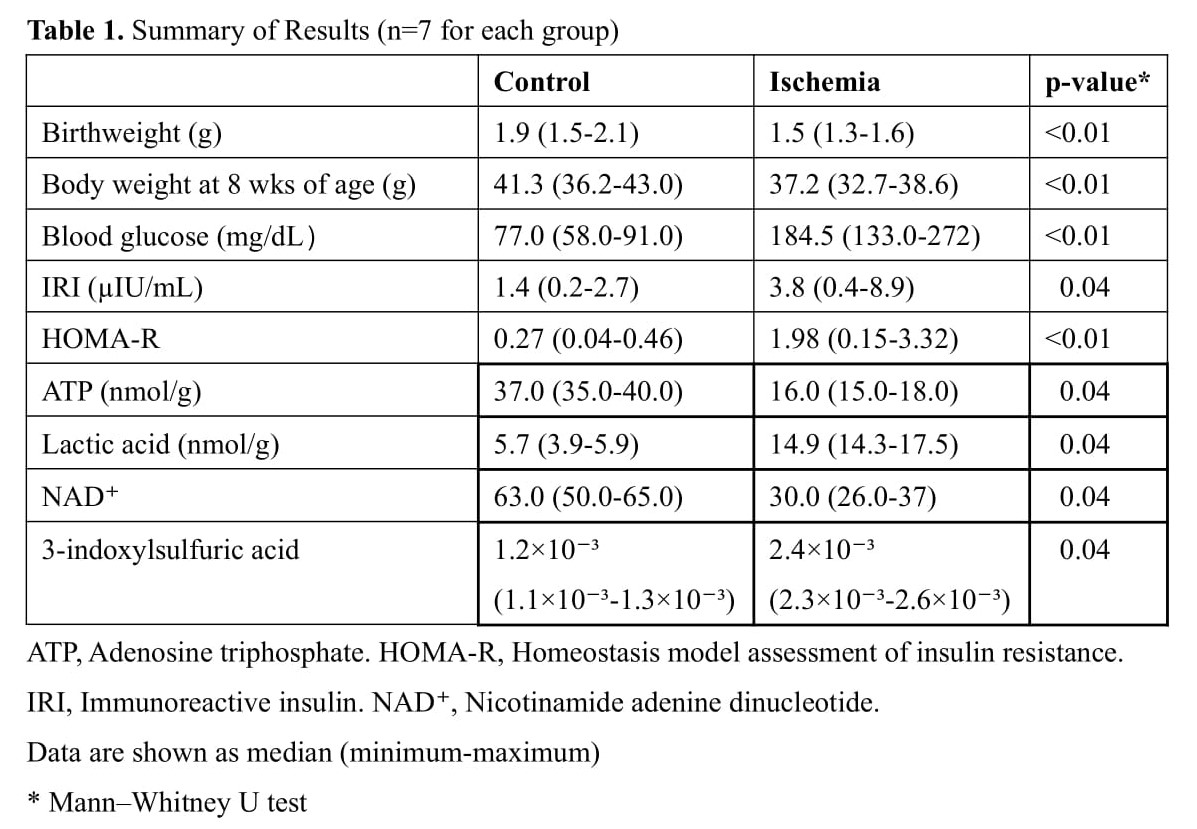
Results: Birthweight was significantly lower in Group I at birth, confirming SGA, and then remained underweight and showed hyperglycemia at 8 wks of age. In addition, IRI and HOMA-R were significantly higher in Group I. Metabolite analyses of Group I livers showed a significantly reduction of adenosine triphosphate and nicotinamide adenine dinucleotide production, and an increase in lactic acid compared with Group C, suggesting mitochondrial dysfunction. Furthermore, 3-indoxylsulfuric acid, an oxidative stress marker, levels in Group I were also significantly higher (Table 1).Conclusion(s): We confirmed our non-obese diabetic mouse model using intrauterine ischemia can yield in SGA pups and resultant hyperglycemia. It appears that the mechanism of hyperglycemia is due to insulin resistance as a result of mitochondrial dysfunction.
Summary of Results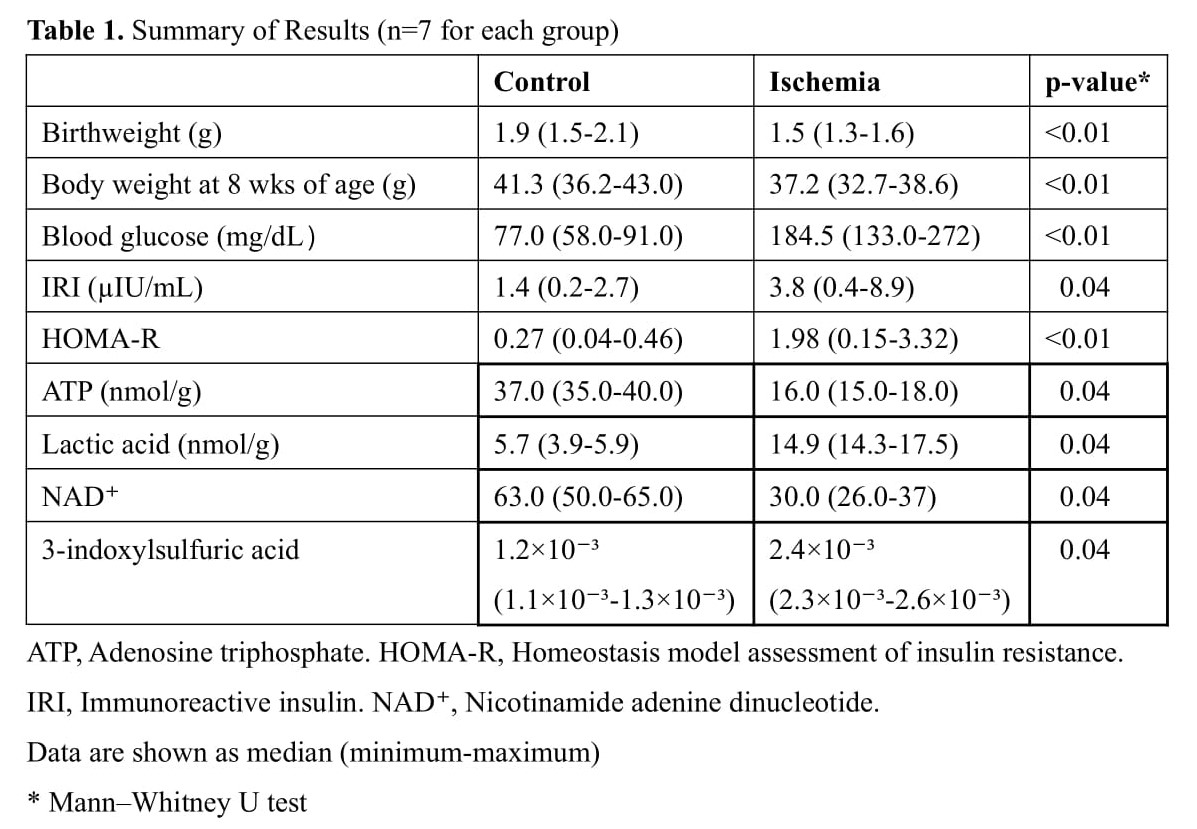
Objective: To develop an adult non-obese diabetic mouse model using intrauterine ischemia to induce SGA in order to study the pathogenesis of hyperglycemia.
Design/Methods: This study was conducted with the approval of our animal ethics committee. At E16.5, intrauterine ischemia, where blood flow in both uterine arteries is blocked for 15 min, was performed in a subgroup of pregnant mice (I). Non-occluded dams were used as sham controls (C). After birth, female pups from each group were weaned at 4 wks of age and bred at 8 wks of age (n=7 for each group). Fasting blood glucose levels, serum insulin (IRI) concentrations, and homeostasis model assessment of insulin resistance (HOMA-R) were compared at 8 wks of age. Metabolite analyses were then performed on the liver tissues at 8 wks of age.
Results: Birthweight was significantly lower in Group I at birth, confirming SGA, and then remained underweight and showed hyperglycemia at 8 wks of age. In addition, IRI and HOMA-R were significantly higher in Group I. Metabolite analyses of Group I livers showed a significantly reduction of adenosine triphosphate and nicotinamide adenine dinucleotide production, and an increase in lactic acid compared with Group C, suggesting mitochondrial dysfunction. Furthermore, 3-indoxylsulfuric acid, an oxidative stress marker, levels in Group I were also significantly higher (Table 1).Conclusion(s): We confirmed our non-obese diabetic mouse model using intrauterine ischemia can yield in SGA pups and resultant hyperglycemia. It appears that the mechanism of hyperglycemia is due to insulin resistance as a result of mitochondrial dysfunction.
Summary of Results