Back
Neonatal Nephrology/AKI
Category: Abstract Submission
Neonatal Nephrology/AKI I
114 - Acute Kidney Injury and Fluid Accumulation Following Neonatal Sepsis
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 114
Publication Number: 114.125
Publication Number: 114.125
Shruthi Mohan, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Faris N. Al Gharaibeh, Cincinnati Children's Hospital Medical Center, cincinnati, OH, United States; Michael Santoro, Cincinnati Children's Hospital Medical Center, Indianapolis, IN, United States; Stuart L. Goldstein, Cincinnati Children's Hospital, Cincinnati, OH, United States; Cara Slagle, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Shruthi Mohan, MBBS, MD (she/her/hers)
Pediatric nephrology fellow, PGY5
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Acute kidney injury (AKI) and/or fluid overload are associated with increased morbidity and mortality in critically ill neonates. Data regarding neonatal AKI and fluid accumulation (FA) following sepsis are sparse in the neonatal intensive care unit (NICU).
Objective: Describe the incidence of AKI and FA following neonatal sepsis and assess for associations with mortality.
Design/Methods: This retrospective study included neonates with a positive blood culture, admitted to Cincinnati Children’s or University of Cincinnati NICUs from 6/2020 to 6/2021. Exclusion criteria: < 5 days of antibiotics, no serum creatinine (SCr) data, or presence of a congenital kidney anomaly with dialysis dependence. AKI was the primary outcome, defined by the neonatal modified Kidney Diseases: Improving Global Outcomes definition. FA was calculated for 7 days after positive culture by cumulative net fluid balance (L)/dry weight (kg). FA was not adjusted for insensible losses.
Results: 49 neonates had 54 sepsis episodes with a 33% (n=18/54) incidence of AKI. AKI diagnosis was based on SCr criteria alone in 22% (n=12), urine output (UO) criteria alone in 2% (n=1) and combined SCr and UO criteria in 11% (n=6). AKI stage ≥ 2 accounted for 55% (n=10). No subjects received renal replacement therapy. There was a 22% mortality rate (n=11). Four subjects experienced death prior to 48 hours and were excluded from further FA analysis. Median peak FA to day 7 was 31% [IQR: 23%,47%] with median time to >10% FA of 2 days [IQR: 1, 3]. FA >10% occurring on day 1 was associated with AKI (50% vs. 15%, OR 5.8, 95% CI 1.5-22.7, p=0.008). Subject demographics, nephrotoxic antibiotic exposure, and caffeine exposure did not differ between AKI and no AKI subgroups (table 1). Subjects with AKI were more likely to require vasopressor support (55% vs 25%, OR:3.7, 95%CI 1.1-12.4, p=0.027) and had more SCr measurements (7 [IQR: 3,8] vs. 3 [IQR: 2,5], p=0.013). Mortality risk was increased in subjects with any AKI (47% vs 9%, OR 8.5, 95%CI 1.9-39.4, p=0.003) and FA >10% occurring on day 1 (38% vs 6%, OR: 9.4, 95%CI 1.5-57.6, p=0.007) (figure 1). Multivariable logistic regression model including AKI, gestational age at birth, birthweight, sex, and race showed that AKI retained association with mortality, aOR 15.9, 95% CI 1.8-137.3, p 0.01 (table 2).Conclusion(s): AKI and early FA in neonatal sepsis was associated with higher mortality. Focus on AKI and FA prevention could potentially mitigate some of the mortality.
Shruthi Mohan_CV 01/22CV-Shruthi Mohan 01:22.pdf
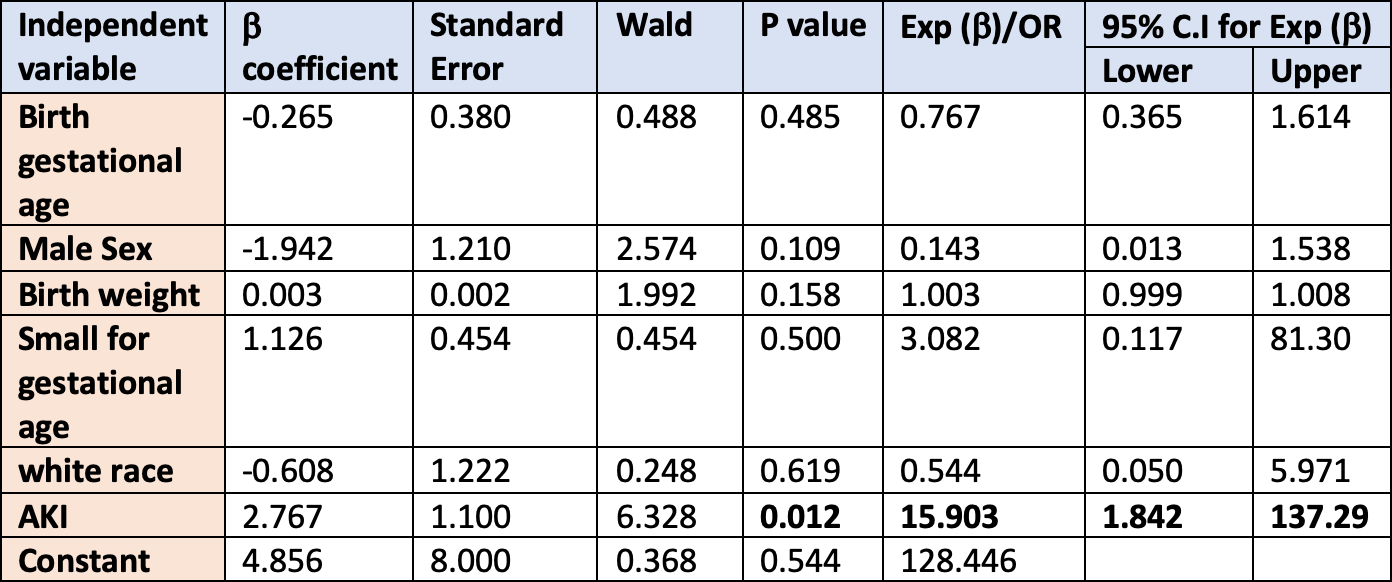
Table 2: Multivariable Logistic Regression Model for Mortality in Blood Culture Positive Neonatal Sepsis.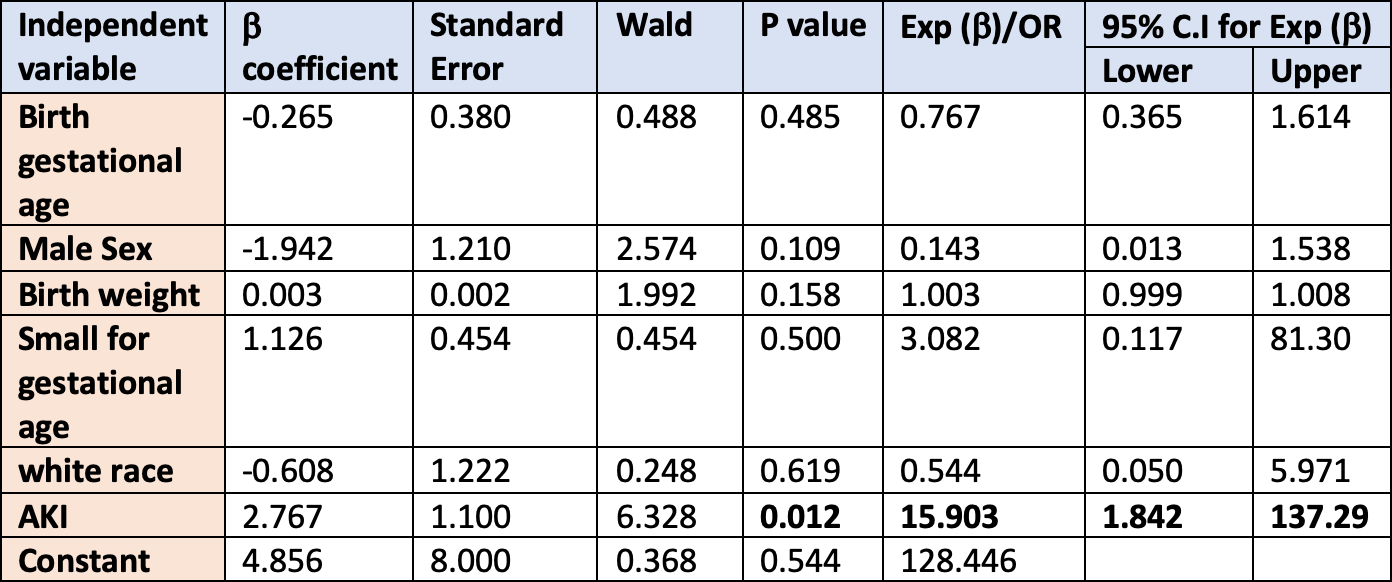
Objective: Describe the incidence of AKI and FA following neonatal sepsis and assess for associations with mortality.
Design/Methods: This retrospective study included neonates with a positive blood culture, admitted to Cincinnati Children’s or University of Cincinnati NICUs from 6/2020 to 6/2021. Exclusion criteria: < 5 days of antibiotics, no serum creatinine (SCr) data, or presence of a congenital kidney anomaly with dialysis dependence. AKI was the primary outcome, defined by the neonatal modified Kidney Diseases: Improving Global Outcomes definition. FA was calculated for 7 days after positive culture by cumulative net fluid balance (L)/dry weight (kg). FA was not adjusted for insensible losses.
Results: 49 neonates had 54 sepsis episodes with a 33% (n=18/54) incidence of AKI. AKI diagnosis was based on SCr criteria alone in 22% (n=12), urine output (UO) criteria alone in 2% (n=1) and combined SCr and UO criteria in 11% (n=6). AKI stage ≥ 2 accounted for 55% (n=10). No subjects received renal replacement therapy. There was a 22% mortality rate (n=11). Four subjects experienced death prior to 48 hours and were excluded from further FA analysis. Median peak FA to day 7 was 31% [IQR: 23%,47%] with median time to >10% FA of 2 days [IQR: 1, 3]. FA >10% occurring on day 1 was associated with AKI (50% vs. 15%, OR 5.8, 95% CI 1.5-22.7, p=0.008). Subject demographics, nephrotoxic antibiotic exposure, and caffeine exposure did not differ between AKI and no AKI subgroups (table 1). Subjects with AKI were more likely to require vasopressor support (55% vs 25%, OR:3.7, 95%CI 1.1-12.4, p=0.027) and had more SCr measurements (7 [IQR: 3,8] vs. 3 [IQR: 2,5], p=0.013). Mortality risk was increased in subjects with any AKI (47% vs 9%, OR 8.5, 95%CI 1.9-39.4, p=0.003) and FA >10% occurring on day 1 (38% vs 6%, OR: 9.4, 95%CI 1.5-57.6, p=0.007) (figure 1). Multivariable logistic regression model including AKI, gestational age at birth, birthweight, sex, and race showed that AKI retained association with mortality, aOR 15.9, 95% CI 1.8-137.3, p 0.01 (table 2).Conclusion(s): AKI and early FA in neonatal sepsis was associated with higher mortality. Focus on AKI and FA prevention could potentially mitigate some of the mortality.
Shruthi Mohan_CV 01/22CV-Shruthi Mohan 01:22.pdf
Table 2: Multivariable Logistic Regression Model for Mortality in Blood Culture Positive Neonatal Sepsis.