Back
Neonatal Nephrology/AKI
Category: Abstract Submission
Neonatal Nephrology/AKI I
105 - Acute kidney injury in preterm neonates decreases cerebral tissue oxygenation
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 105
Publication Number: 105.125
Publication Number: 105.125
Kari Borowski, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Matthew W. Harer, University of Wisconsin, Middleton, WI, United States; Claudette O. Adegboro, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States

Kari Borowski, BS
Medical Student
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: The kidney and central nervous system are strongly interconnected. In preterm neonates, acute kidney injury (AKI) has been independently associated with increased rates and severity of intraventricular hemorrhage (IVH). Similarly, research in children has demonstrated a link between chronic kidney disease (CKD) and abnormal brain architecture and function. Prior near-infrared spectroscopy (NIRS) tissue oxygenation studies in critically ill neonates have not evaluated differences in cerebral tissue oxygenation (CrSO2) based on AKI status. The purpose of this study was to evaluate CrSO2 trends in neonates with and without AKI.
Objective: Our objective was to determine the effect of AKI on CrSO2 in preterm neonates.
Design/Methods: We retrospectively evaluated the CrSO2 values of 35 neonates born less than 32 weeks’ gestation who were prospectively enrolled in a continuous NIRS monitoring study in the first week. AKI was determined by the modified neonatal Kidney Disease: Improving Global Outcomes (KDIGO) definition including urine output (UOP). Incidence of IVH and periventricular leukomalacia (PVL) were collected from head ultrasound or MRI imaging performed at any time during the NICU hospitalization.
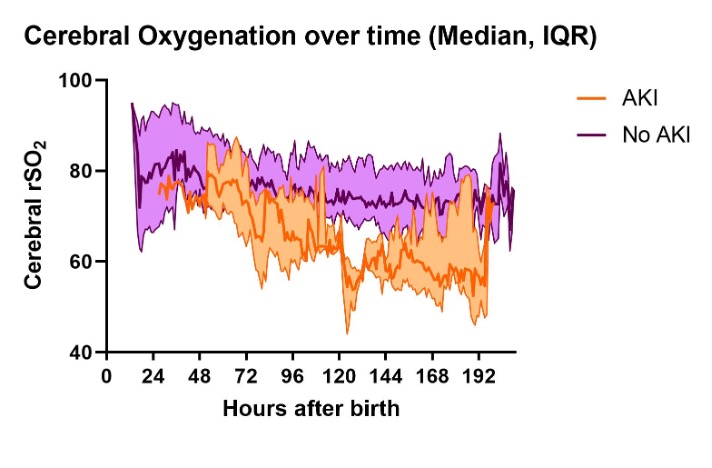
Results: Three patients developed AKI, one with stage 1 and two with stage 2, at an average age of 5 days. There was no difference in rates of IVH or PVL between the AKI and no AKI groups (AKI, n=1 (33.33%); No AKI, n=6 (18.75%), p=0.124). The median CrSO2 values for AKI patients were significantly lower for the first week compared to the no AKI patients (65.12% vs. 75.67%, p< 0.0001, figure 1). The fluctuations in median CrSO2 values for AKI vs. no AKI groups over time are shown in figure 2 with the peak difference seen at 5 days of age.Conclusion(s): In this small pilot analysis, neonates with AKI had lower cerebral oxygenation compared to those without AKI. While this data does not prove that AKI decreases cerebral oxygenation, it highlights the possibility that cerebral tissue perfusion or oxygen utilization may be affected by AKI independent of IVH or PVL. Additionally, these results indicate that declines in cerebral oxygenation may predict AKI onset sooner than current diagnostic criteria allow. Further investigation with a larger sample size is needed to determine the extent to which AKI affects cerebral oxygenation as well as the timing of these changes. Future preterm neonatal NIRS and AKI studies should include short- and long-term neurodevelopmental outcomes to evaluate if prevention of AKI may also protect against brain injury in preterm neonates.
Figure 1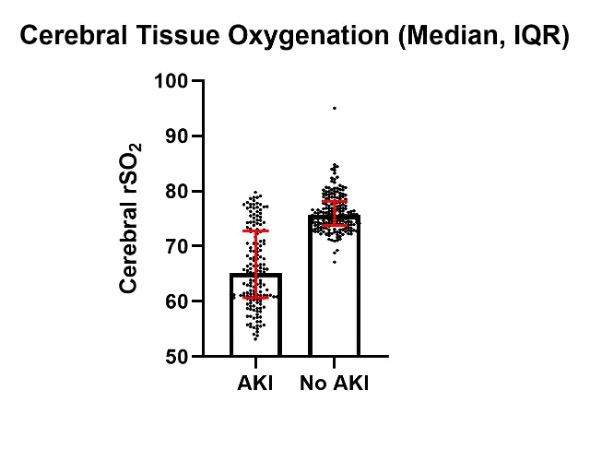
Figure 2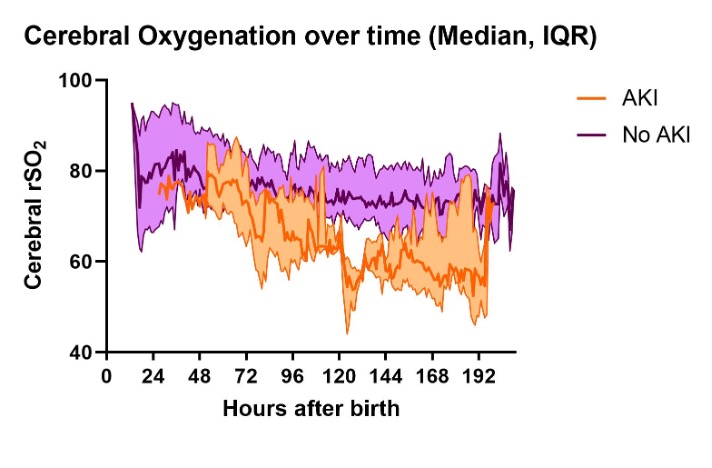
Objective: Our objective was to determine the effect of AKI on CrSO2 in preterm neonates.
Design/Methods: We retrospectively evaluated the CrSO2 values of 35 neonates born less than 32 weeks’ gestation who were prospectively enrolled in a continuous NIRS monitoring study in the first week. AKI was determined by the modified neonatal Kidney Disease: Improving Global Outcomes (KDIGO) definition including urine output (UOP). Incidence of IVH and periventricular leukomalacia (PVL) were collected from head ultrasound or MRI imaging performed at any time during the NICU hospitalization.
Results: Three patients developed AKI, one with stage 1 and two with stage 2, at an average age of 5 days. There was no difference in rates of IVH or PVL between the AKI and no AKI groups (AKI, n=1 (33.33%); No AKI, n=6 (18.75%), p=0.124). The median CrSO2 values for AKI patients were significantly lower for the first week compared to the no AKI patients (65.12% vs. 75.67%, p< 0.0001, figure 1). The fluctuations in median CrSO2 values for AKI vs. no AKI groups over time are shown in figure 2 with the peak difference seen at 5 days of age.Conclusion(s): In this small pilot analysis, neonates with AKI had lower cerebral oxygenation compared to those without AKI. While this data does not prove that AKI decreases cerebral oxygenation, it highlights the possibility that cerebral tissue perfusion or oxygen utilization may be affected by AKI independent of IVH or PVL. Additionally, these results indicate that declines in cerebral oxygenation may predict AKI onset sooner than current diagnostic criteria allow. Further investigation with a larger sample size is needed to determine the extent to which AKI affects cerebral oxygenation as well as the timing of these changes. Future preterm neonatal NIRS and AKI studies should include short- and long-term neurodevelopmental outcomes to evaluate if prevention of AKI may also protect against brain injury in preterm neonates.
Figure 1
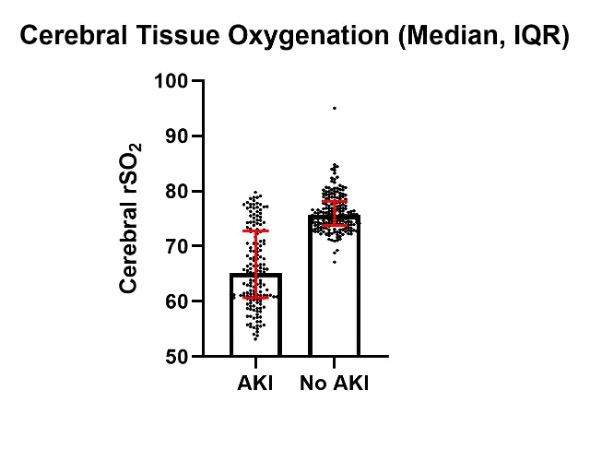
Figure 2