Emergency Medicine: All Areas
Category: Abstract Submission
4: Emergency Medicine I
38 - Children with mental health emergencies transported by EMS/police require more ED interventions and resources
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 38
Publication Number: 38.103
Publication Number: 38.103
Alexandra Cheetham, Children's Cincinnati, Cincinnati, OH, United States; Rachel Bensman, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Victoria Hartwell, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Lauren C. Riney, Pediatric Emergency Medicine, Cincinnati, OH, United States; Sang Hoon Lee, University of Cincinnati College of Medicine, Cincinnati, OH, United States; Lynn Babcock, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Wendy Pomerantz, Cincinnati Children's Hospital, Cincinnati, OH, United States

Alexandra Cheetham, MD
Fellow
Cincinnati Children's Hospital
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Mental health (MH) visits to pediatric emergency departments (EDs) have been increasing in recent years. Many of these patients are transported by Emergency Medical Services (EMS) or police. Patients with MH emergencies transported by EMS/police tend to have more severe symptoms and display more violent behavior.
Objective: To describe patient characteristics, ED interventions and outcomes for pediatric patients with acute MH needs transported by EMS or police compared to patients who self-transport.
Design/Methods: A retrospective electronic medical record review was conducted on a cohort of patients 5-18 years old who presented to a free-standing children’s hospital ED and its satellite ED from January 1, 2012 to December 31, 2020 with a MH chief complaint. Patients who self-transported were compared to those who arrived via EMS or police. Variables included demographics, Brief Rating of Aggression by Children and Adolescents (BRACHA) - a 14 point scale of risk of aggressive behavior, mechanical or physical restraint use, and psychiatric medication administration. Chi–square analysis was used to compare groups.
Results: During the study period, 471,509 patients 5-18 years old presented to the ED of which 70,557 (15%) had a MH complaint. Of MH patients, 79.5% self-transported, 14.6% arrived by EMS, and 5.9% were transported by police; mean age was 13.1 years (SD=3.1) and 47% were male. BRACHA was performed for 32,906 (47%) patients. Mean scores were significantly higher for EMS (5.6, SD 3.0) and police transports (6.1, SD 2.9) compared to self-transported patients (4.7, SD 3.1), p=0.004 and p < 0.001, respectively. Patients transported by EMS or police were more likely to require psychiatric medications and mechanical or physical restraint in the ED and more likely to be admitted to the hospital (Table). The most common medications used for chemical restraint were benzodiazepines and olanzapine.Conclusion(s): Patients with acute MH needs transported by EMS and police require more interventions in the ED than patients who self-transport. Higher ED restraint use, more frequent psychiatric medication administration, and higher admission rates for patients transported by EMS/police suggest these patients exhibit more aggressive behaviors and require more care and resources than patients who self-transport. EMS and police education should focus on stabilization and safe transport of patients with MH needs, including management of agitation and aggression.
Table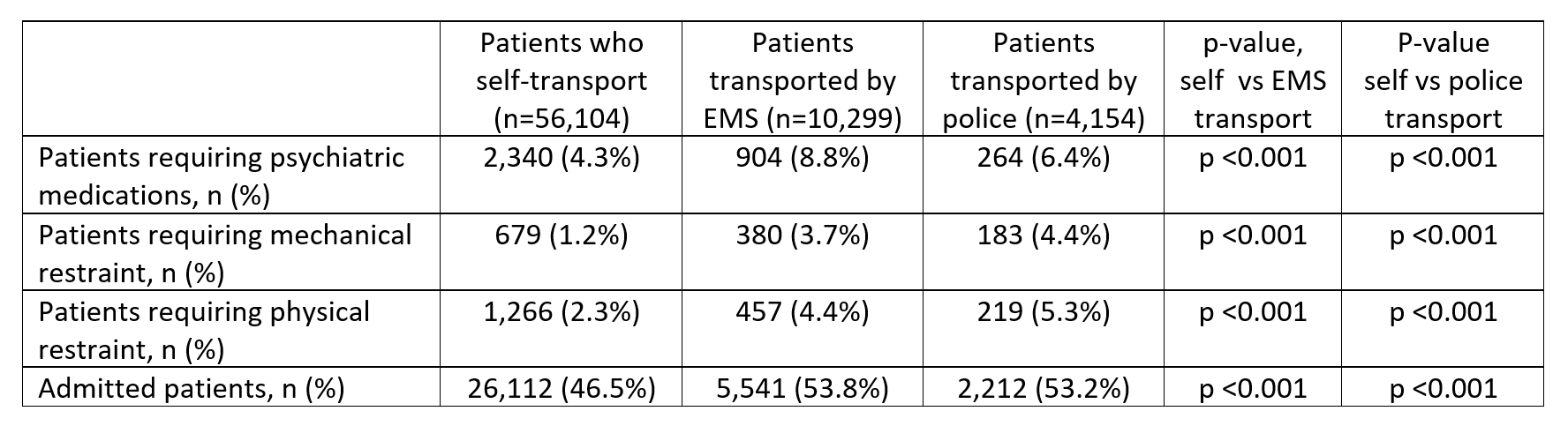 ED interventions and admissions for self-transported patients compared to patients transported by EMS and police
ED interventions and admissions for self-transported patients compared to patients transported by EMS and police
Objective: To describe patient characteristics, ED interventions and outcomes for pediatric patients with acute MH needs transported by EMS or police compared to patients who self-transport.
Design/Methods: A retrospective electronic medical record review was conducted on a cohort of patients 5-18 years old who presented to a free-standing children’s hospital ED and its satellite ED from January 1, 2012 to December 31, 2020 with a MH chief complaint. Patients who self-transported were compared to those who arrived via EMS or police. Variables included demographics, Brief Rating of Aggression by Children and Adolescents (BRACHA) - a 14 point scale of risk of aggressive behavior, mechanical or physical restraint use, and psychiatric medication administration. Chi–square analysis was used to compare groups.
Results: During the study period, 471,509 patients 5-18 years old presented to the ED of which 70,557 (15%) had a MH complaint. Of MH patients, 79.5% self-transported, 14.6% arrived by EMS, and 5.9% were transported by police; mean age was 13.1 years (SD=3.1) and 47% were male. BRACHA was performed for 32,906 (47%) patients. Mean scores were significantly higher for EMS (5.6, SD 3.0) and police transports (6.1, SD 2.9) compared to self-transported patients (4.7, SD 3.1), p=0.004 and p < 0.001, respectively. Patients transported by EMS or police were more likely to require psychiatric medications and mechanical or physical restraint in the ED and more likely to be admitted to the hospital (Table). The most common medications used for chemical restraint were benzodiazepines and olanzapine.Conclusion(s): Patients with acute MH needs transported by EMS and police require more interventions in the ED than patients who self-transport. Higher ED restraint use, more frequent psychiatric medication administration, and higher admission rates for patients transported by EMS/police suggest these patients exhibit more aggressive behaviors and require more care and resources than patients who self-transport. EMS and police education should focus on stabilization and safe transport of patients with MH needs, including management of agitation and aggression.
Table
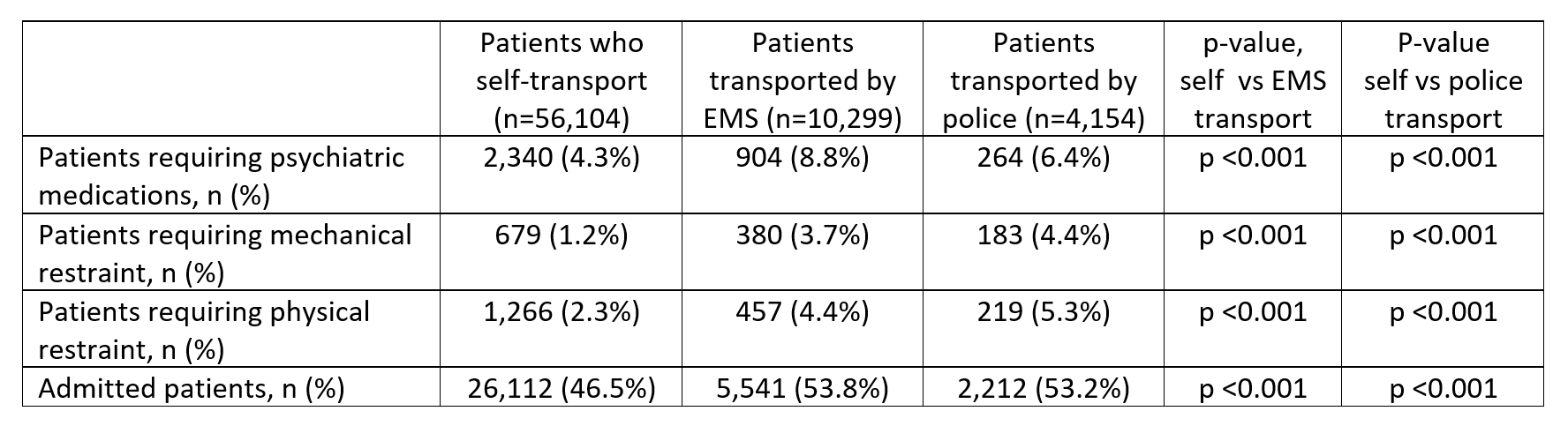 ED interventions and admissions for self-transported patients compared to patients transported by EMS and police
ED interventions and admissions for self-transported patients compared to patients transported by EMS and police