Neonatal General
Category: Abstract Submission
Neonatology General 2: Brain - Renal - Electrolytes
361 - Identifying the Critical Window in Growth Associated with Neurodevelopmental Outcome in Preterm Infants Born < 30 Weeks Gestation
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 361
Publication Number: 361.132
Publication Number: 361.132
Izabela Oluwole, Loma Linda University Children's Hospital, Redlands, CA, United States; John B. C. Tan, Loma Linda University Children's Hospital, Riverside, CA, United States; Rebekah M. Leigh, Loma Linda University School of Medicine, Redlands, CA, United States; Gina Hou, Loma Linda University Children's Hospital, Redlands, CA, United States; Fu-Sheng Chou, Loma Linda University School of Medicine, Loma Linda, CA, United States

Izabela Oluwole, MD
Fellow
Loma Linda University Children's Hospital
Loma Linda, California, United States
Presenting Author(s)
Background: Neurodevelopmental outcomes in preterm infants is known to be related to nutrition and growth. It is currently unknown if there is a critical window within a preterm infant’s growth trajectory during the early postnatal life that is most associated with neurodevelopmental outcome. Identification of this critical window in growth could lead to improving neurodevelopmental outcome.
Objective: We aimed to identify the critical window of growth which is most associated with neurodevelopmental outcome.
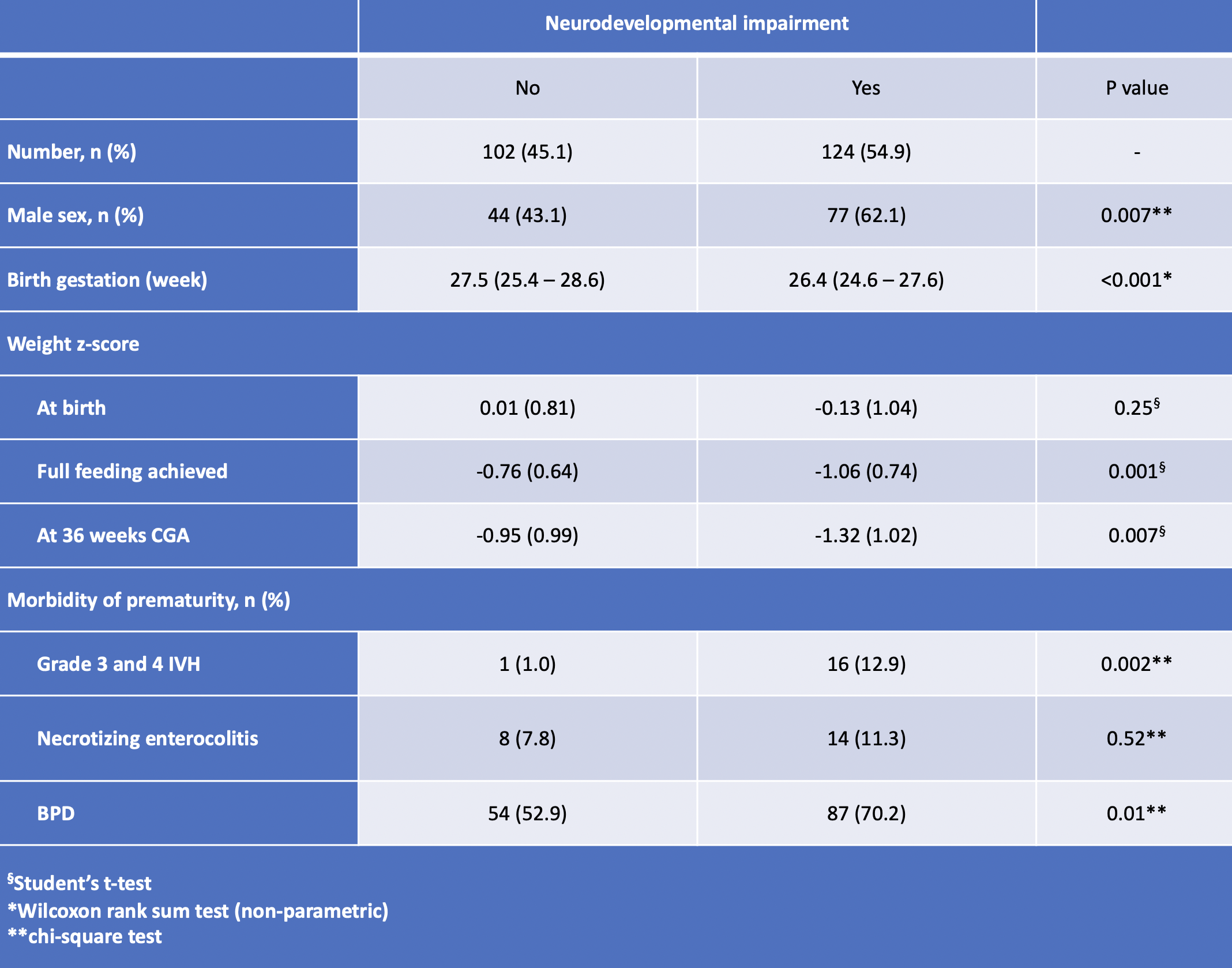
Design/Methods: We conducted a single-center retrospective study from 2015 to 2019 in infants born < 30 weeks gestation. Demographic, weight data, and Bayley Scales of Infant and Toddler Development (BSID) scaled scores were extracted from the electronic medical records database. Neurodevelopmental impairment (NDI) was assigned when any patient had a scaled score of < 7 for any BSID domain or had cerebral palsy. Weight z-scores were calculated based on 2013 Fenton growth charts. To narrow down the critical window, we designated three clinically important time points for premature infants: 1) birth, 2) time when full enteral feeds (TFEF) is achieved, and 3) corrected gestational age (CGA) at 36 weeks. Then, we calculated the difference in weight z-scores between time points and compared the differences in weight z-score between patients with and without neurodevelopmental impairment (NDI). Furthermore, we performed a multiple logistic regression to determine the association between TFEF and NDI while adjusting for birth gestation and birth weight z-score.
Results: We identified 226 patients born at < 30 weeks gestation available for analysis. Demographic characteristics are summarized in Table 1. The average differences in weight z-scores were calculated for the three timepoints between patients with and without NDI (Figure 1). Between birth and TFEF we found that there was a significant decrease in the differences in weight z-score in the NDI group compared to the no-NDI group. Between TFEF and 36 weeks CGA we did not find any significant difference between the two groups. In a logistic regression model, the association between time-to-full-enteral-feeds and NDI remained significant after adjusting for GA and birth weight z-score (Figure 2).Conclusion(s): We identified the critical window in growth which is associated with NDI to be between birth and achieving full enteral feeds. Ensuring adequate growth in the critical window may have the strongest influence on neurodevelopmental outcomes.
Table 1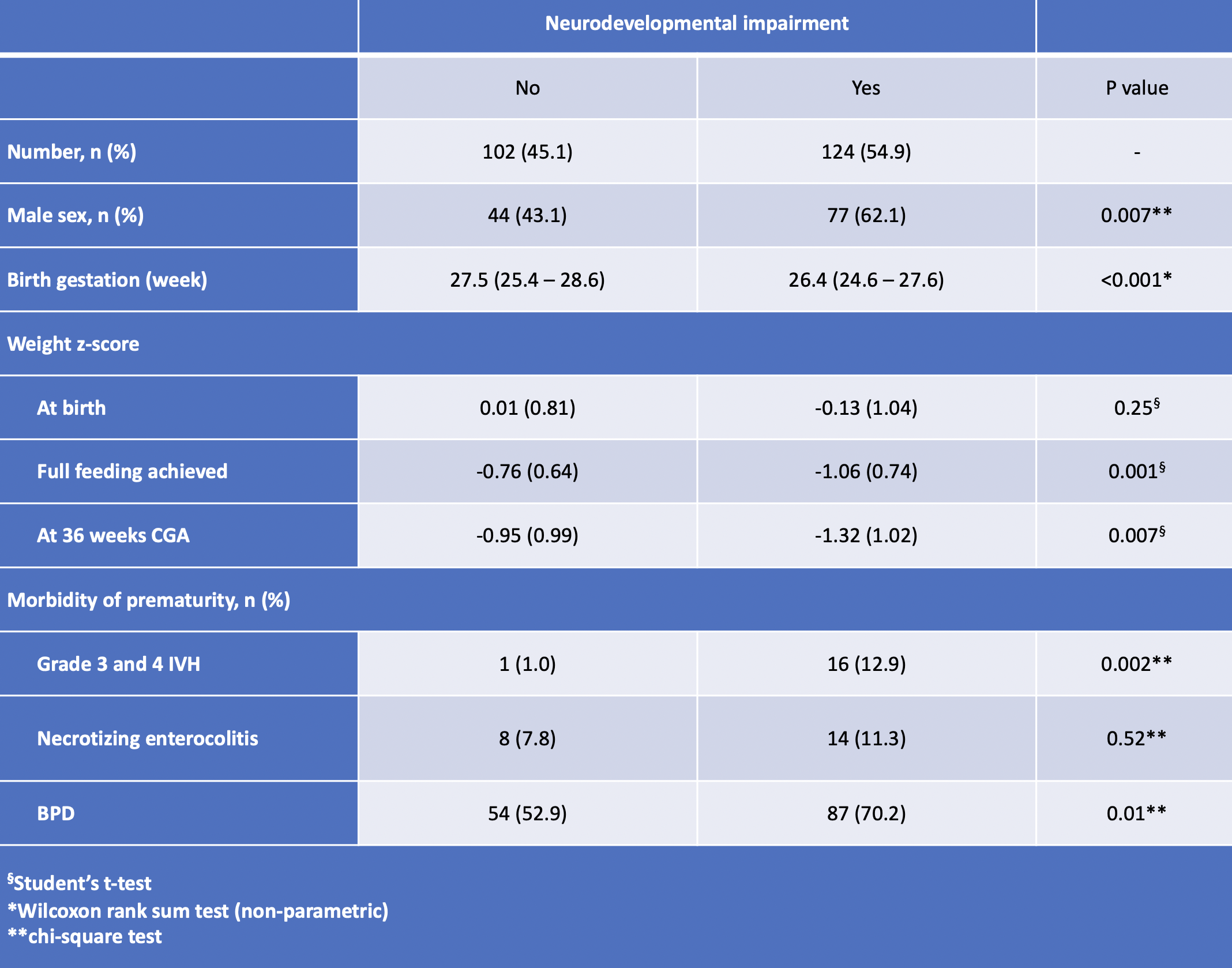 Demographic characteristics of the babies included in the study
Demographic characteristics of the babies included in the study
Figure 1.png) Plots showing the trends of weight z-scores at indicated timepoints in babies with and without NDI. Differences in weight z-scores between timepoints and the associated with descriptive statistics (Student’s t-test) are presented in the table.
Plots showing the trends of weight z-scores at indicated timepoints in babies with and without NDI. Differences in weight z-scores between timepoints and the associated with descriptive statistics (Student’s t-test) are presented in the table.
Objective: We aimed to identify the critical window of growth which is most associated with neurodevelopmental outcome.
Design/Methods: We conducted a single-center retrospective study from 2015 to 2019 in infants born < 30 weeks gestation. Demographic, weight data, and Bayley Scales of Infant and Toddler Development (BSID) scaled scores were extracted from the electronic medical records database. Neurodevelopmental impairment (NDI) was assigned when any patient had a scaled score of < 7 for any BSID domain or had cerebral palsy. Weight z-scores were calculated based on 2013 Fenton growth charts. To narrow down the critical window, we designated three clinically important time points for premature infants: 1) birth, 2) time when full enteral feeds (TFEF) is achieved, and 3) corrected gestational age (CGA) at 36 weeks. Then, we calculated the difference in weight z-scores between time points and compared the differences in weight z-score between patients with and without neurodevelopmental impairment (NDI). Furthermore, we performed a multiple logistic regression to determine the association between TFEF and NDI while adjusting for birth gestation and birth weight z-score.
Results: We identified 226 patients born at < 30 weeks gestation available for analysis. Demographic characteristics are summarized in Table 1. The average differences in weight z-scores were calculated for the three timepoints between patients with and without NDI (Figure 1). Between birth and TFEF we found that there was a significant decrease in the differences in weight z-score in the NDI group compared to the no-NDI group. Between TFEF and 36 weeks CGA we did not find any significant difference between the two groups. In a logistic regression model, the association between time-to-full-enteral-feeds and NDI remained significant after adjusting for GA and birth weight z-score (Figure 2).Conclusion(s): We identified the critical window in growth which is associated with NDI to be between birth and achieving full enteral feeds. Ensuring adequate growth in the critical window may have the strongest influence on neurodevelopmental outcomes.
Table 1
 Demographic characteristics of the babies included in the study
Demographic characteristics of the babies included in the studyFigure 1
.png) Plots showing the trends of weight z-scores at indicated timepoints in babies with and without NDI. Differences in weight z-scores between timepoints and the associated with descriptive statistics (Student’s t-test) are presented in the table.
Plots showing the trends of weight z-scores at indicated timepoints in babies with and without NDI. Differences in weight z-scores between timepoints and the associated with descriptive statistics (Student’s t-test) are presented in the table.