Global Neonatal & Children's Health
Category: Abstract Submission
Global Child and Adolescent Health II
156 - Impact of a Neonatal Transport Team in Western India
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 156
Publication Number: 156.112
Publication Number: 156.112
Emma Squire, Stanford University School of Medicine, East Palo Alto, CA, United States; Justin Lee, Stanford University, Palo Alto, CA, United States; Yogendra B. Waratkar, Shrimad Rajchandra Hospital Dharampur Valsad India, Valsad, Gujarat, India; Nilima Ragavan, Stanford University School of Medicine, Palo Alto, CA, United States

Emma Squire, MD
Pediatric Resident
Stanford University School of Medicine
East Palo Alto, California, United States
Presenting Author(s)
Background: Neonatal mortality remains a significant problem in low- and middle-income countries particularly for low birth weight and premature infants. Use of neonatal transport using a specialized team with access to infant-specific equipment helps reduce neonatal morbidity and mortality; however, access to such services is limited particularly in rural communities. Few studies to date have examined the impact of creating culturally-affirming specialized neonatal transport teams tailored specifically for rural communities in India. Prior to 2018, outborn neonates at Shrimad Rajchandra Hospital (SRH), a charitable tertiary care hospital serving rural communities in Gujarat, India, had 3 times higher mortality rates than inborns.
Objective: The goal of this study is to examine neonatal outcomes following implementation of a specialized neonatal transport team.
Design/Methods: In 2018 a multidisciplinary team of doctors, nurse practitioners, critical care transport nurses, and respiratory therapists from Stanford Healthcare helped develop a Neonatal Transport team at SRH with trained staff and a fully equipped neonatal ambulance. Training included didactics, simulations, and development of procedures and protocols. We then conducted an IRB approved retrospective cohort study comparing outcomes of 121 babies transported by the SRH team August 2018 – May 2021 to 128 babies transported by other means, adjusting for multiple covariates including birth weight, gestational age, gender.
Results: We found a lower mortality rate for babies transported by the SRH team (HR 0.44 (0.22, 0.89), p = 0.02). For a subset of babies with low birth weight and prematurity this mortality benefit was further enhanced. Low birth weight and premature newborns transported by the SRH team also had increased survival probability following admission to the NICU (p = 0.047). Furthermore, the SRH team had more equitable patient transports by gender [48% female (SRH) vs 35% female (other)]. There were no neonatal deaths during transport by this specialized team. Conclusion(s): The SRH Neonatal transport team has led to more effective and equitable patient transports in this region. Expanded care delivery to female infants is particularly important as females are often not given the same care due to structural sexism and sex preference. Through this work, we demonstrate the feasibility and potential impact of developing a trained neonatal transport team in a low resource setting. Further work is needed to understand the barriers in utilization of this team and to facilitate earlier transfers of sick neonates.
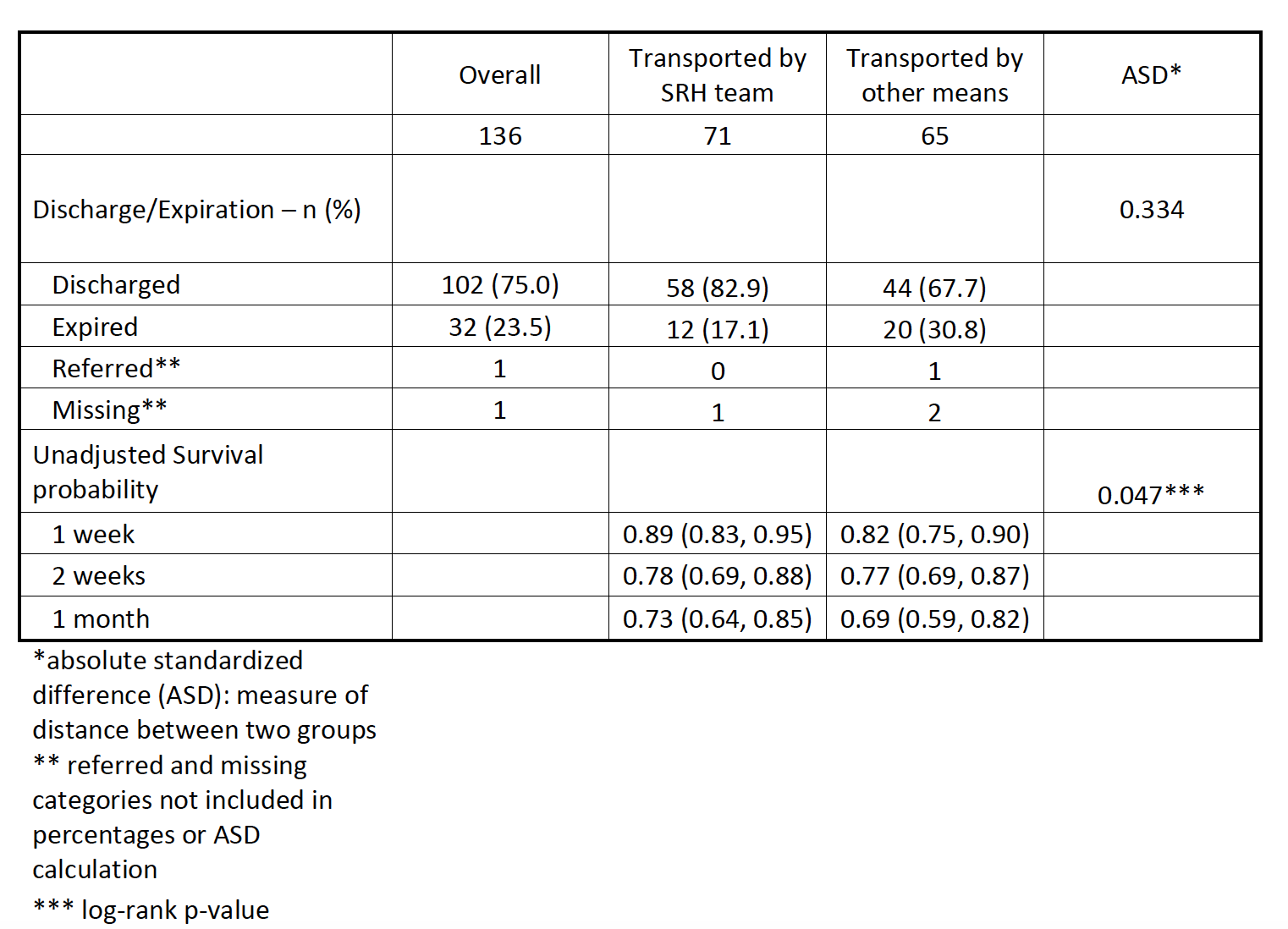
Table 1 Outcome characteristics by cohort for only low birthweight ( < 2.5 Kg) and premature newborns ( < 37w GA)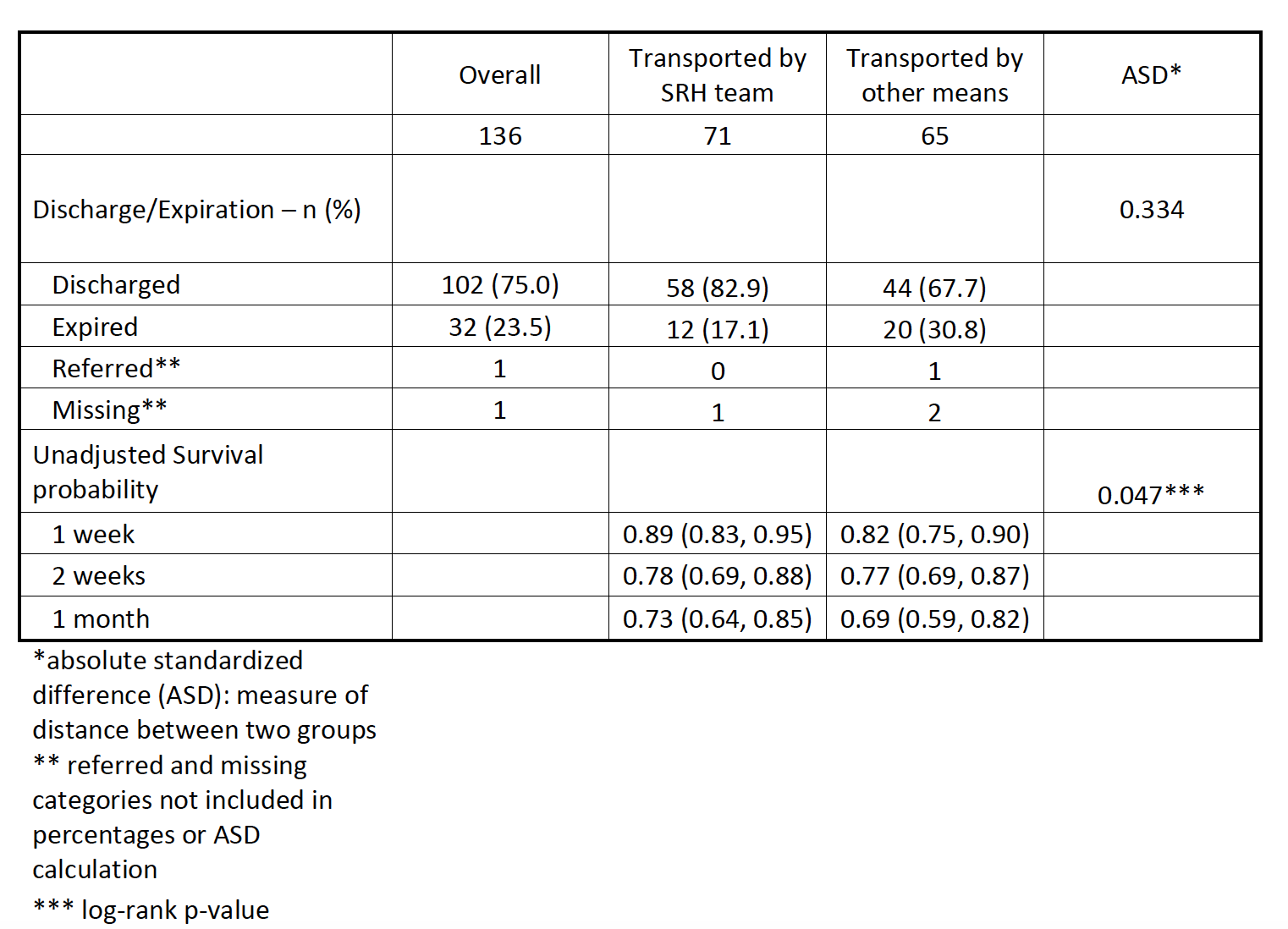
Objective: The goal of this study is to examine neonatal outcomes following implementation of a specialized neonatal transport team.
Design/Methods: In 2018 a multidisciplinary team of doctors, nurse practitioners, critical care transport nurses, and respiratory therapists from Stanford Healthcare helped develop a Neonatal Transport team at SRH with trained staff and a fully equipped neonatal ambulance. Training included didactics, simulations, and development of procedures and protocols. We then conducted an IRB approved retrospective cohort study comparing outcomes of 121 babies transported by the SRH team August 2018 – May 2021 to 128 babies transported by other means, adjusting for multiple covariates including birth weight, gestational age, gender.
Results: We found a lower mortality rate for babies transported by the SRH team (HR 0.44 (0.22, 0.89), p = 0.02). For a subset of babies with low birth weight and prematurity this mortality benefit was further enhanced. Low birth weight and premature newborns transported by the SRH team also had increased survival probability following admission to the NICU (p = 0.047). Furthermore, the SRH team had more equitable patient transports by gender [48% female (SRH) vs 35% female (other)]. There were no neonatal deaths during transport by this specialized team. Conclusion(s): The SRH Neonatal transport team has led to more effective and equitable patient transports in this region. Expanded care delivery to female infants is particularly important as females are often not given the same care due to structural sexism and sex preference. Through this work, we demonstrate the feasibility and potential impact of developing a trained neonatal transport team in a low resource setting. Further work is needed to understand the barriers in utilization of this team and to facilitate earlier transfers of sick neonates.
Table 1 Outcome characteristics by cohort for only low birthweight ( < 2.5 Kg) and premature newborns ( < 37w GA)