Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement II: Neurology and Infection
221 - Implementing Screening for Neonatal Delirium at Rady Children's Hospital NICU
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 221
Publication Number: 221.127
Publication Number: 221.127
Meghana Karmarkar, UCSD, San Diego, CA, United States; Laurel Moyer, Rady Children's Hospital San Diego/ UC San Diego, San Diego, CA, United States; Mark Speziale, Rady Children's Hospital San Diego, San Diego, CA, United States; Dannielle Heath, Rady Children's Hospital San Diego, San Diego, CA, United States

Meghana Karmarkar, MD
Fellow
UCSD
University of California San Diego
San Diego, California, United States
Presenting Author(s)
Background: Delirium is defined as fluctuating changes in awareness and cognition occurring in the setting of a medical illness. Although delirium is recognized in pediatric ICUs, it is not commonly diagnosed in the neonatal population. The NICU at Rady Children's Hospital is comprised of medically complex patients with prolonged hospital courses who are often on multiple medications for pain and sedation. Early recognition and treatment of delirium in the NICU may be helpful in improving clinical outcomes.
Objective: We conducted a QI project to implement screening for neonatal delirium in high-risk patients. Our objective is to increase delirium screening (RASS/CAPD scores) from 0% to 85% in eligible NICU patients by 03/2022.
Design/Methods: Multiple interdisciplinary meetings were initiated with key stakeholders to develop an algorithm for the evaluation of neonatal delirium. Completion of the RASS (Richmond Agitation and Sedation Scale) and age-adjusted CAPD (Cornell Assessment of Pediatric Delirium) scores were used as the objective tool for delirium screening. Weekly nursing compliance with RASS & CAPD score documentation is the primary process measure. Outcome measures include child psychiatry consultations. Initial inclusion criteria at the start of the project was defined as NICU patients > or = 38 weeks corrected gestational age who were mechanically ventilated > 7 days and who were receiving any benzodiazepines or opiates. Inclusion criteria was then expanded to include all infants > or = 38 weeks corrected gestational age. Multiple PDSA’s were conducted to optimize screening through increasing the reliability of the process. This included creation of an order set, and a required documentation checklist in the EMR of patients meeting eligibility criteria.
Results: Implementation of screening and data collection began in October 2020. After implementation, data from 10/2020 through 2/2021 showed an average weekly screening compliance of 76%. (Figure 1). Expansion of the inclusion criteria on 8/2021 resulted in a sharp decrease in compliance. Subsequently, addition of the documentation checklist in the EMR resulted in a center line shift in the data, with a current average weekly screening compliance of 59%. An average of 60% of all eligible NICU patients received a delirium screen prior to discharge (Figure 2).Conclusion(s): Through this QI project, we have increased awareness of neonatal delirium as a diagnosis in our NICU. Our expectation is that early recognition of delirium in our chronic patients will lead to more timely management of symptoms and decreased use of narcotic and sedative medications.
Figure 1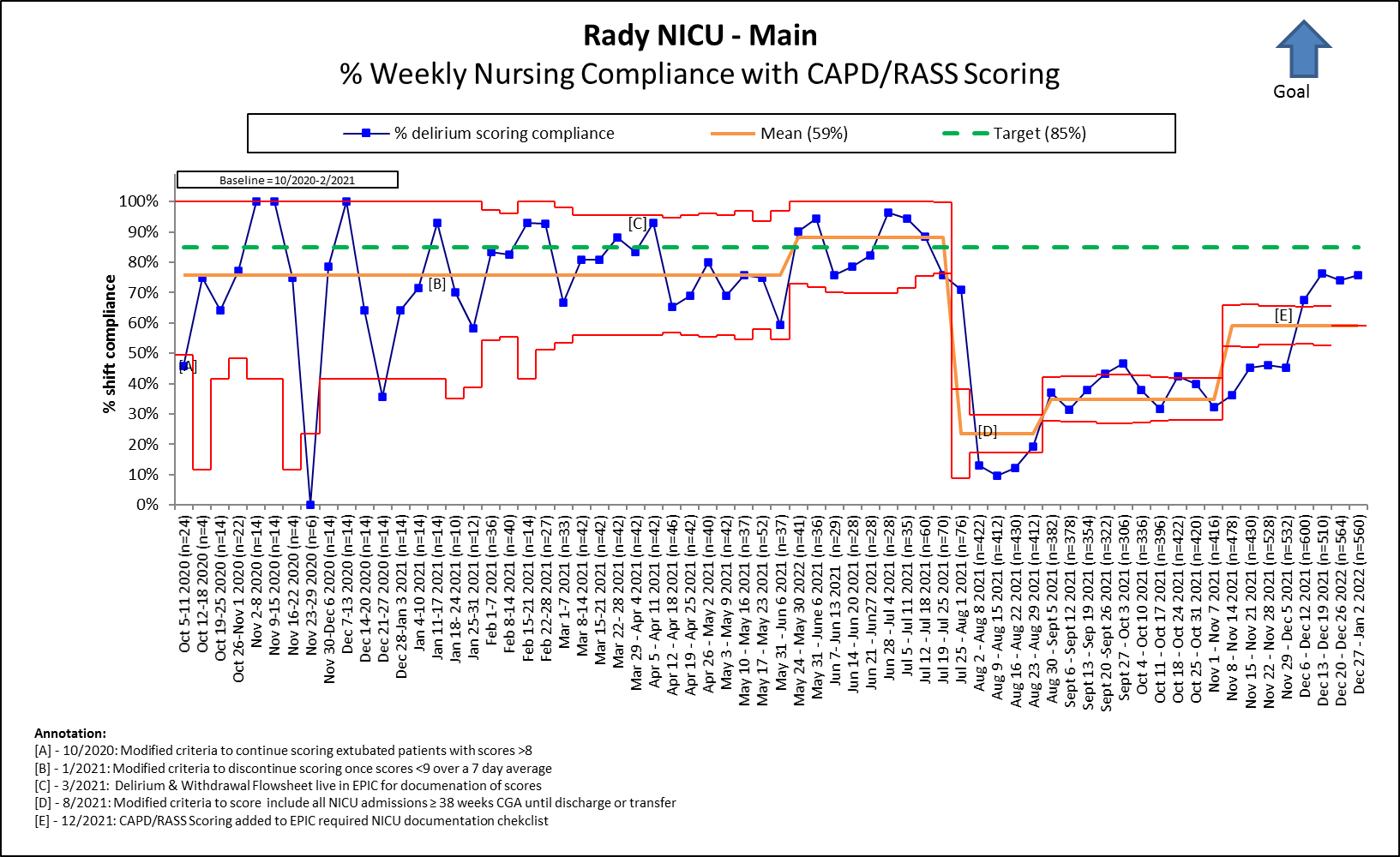 Weekly nursing compliance of Delirium screening.
Weekly nursing compliance of Delirium screening.
Figure 2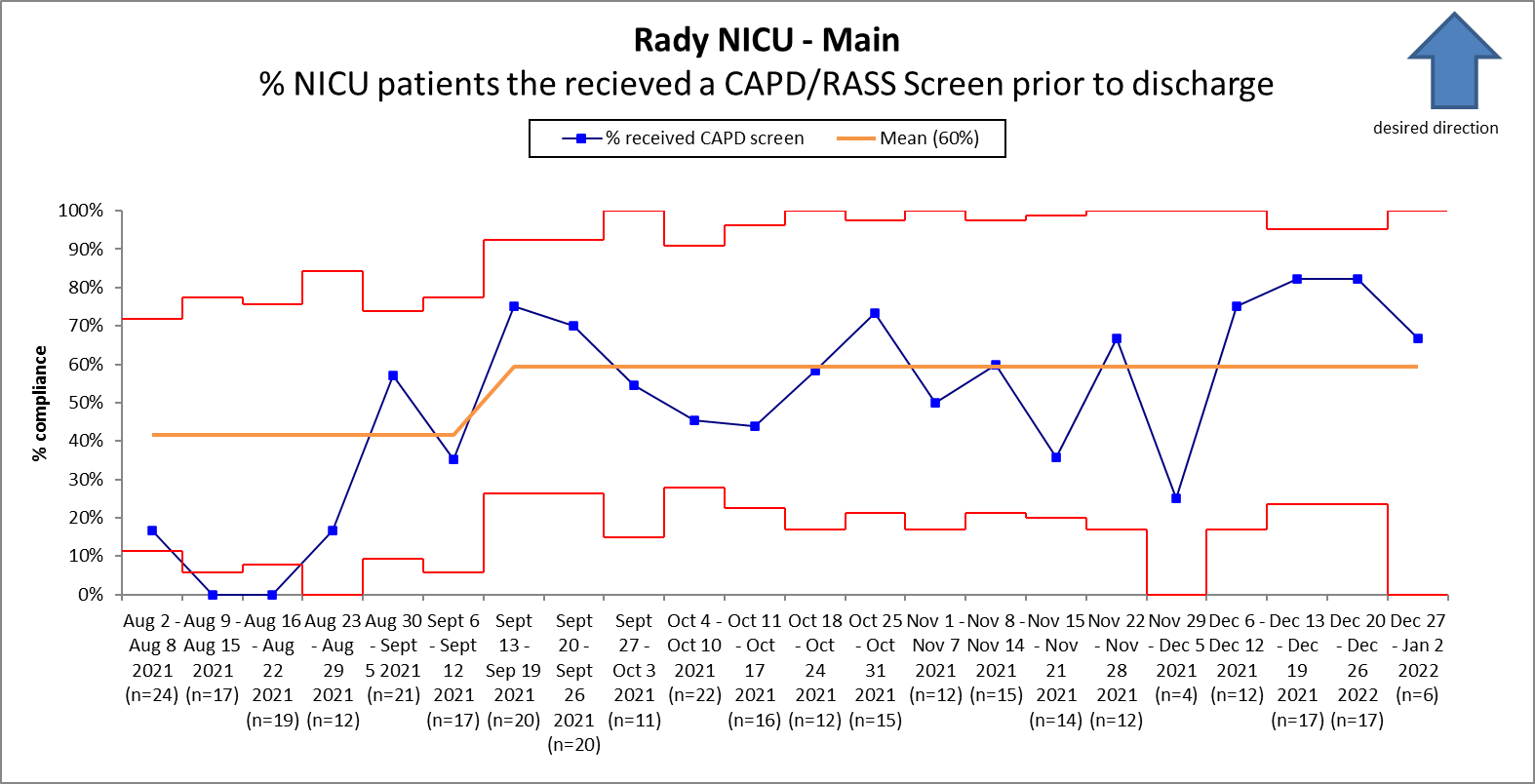 Percentage of NICU Patients receiving a Delirium screen prior to discharge.
Percentage of NICU Patients receiving a Delirium screen prior to discharge.
Objective: We conducted a QI project to implement screening for neonatal delirium in high-risk patients. Our objective is to increase delirium screening (RASS/CAPD scores) from 0% to 85% in eligible NICU patients by 03/2022.
Design/Methods: Multiple interdisciplinary meetings were initiated with key stakeholders to develop an algorithm for the evaluation of neonatal delirium. Completion of the RASS (Richmond Agitation and Sedation Scale) and age-adjusted CAPD (Cornell Assessment of Pediatric Delirium) scores were used as the objective tool for delirium screening. Weekly nursing compliance with RASS & CAPD score documentation is the primary process measure. Outcome measures include child psychiatry consultations. Initial inclusion criteria at the start of the project was defined as NICU patients > or = 38 weeks corrected gestational age who were mechanically ventilated > 7 days and who were receiving any benzodiazepines or opiates. Inclusion criteria was then expanded to include all infants > or = 38 weeks corrected gestational age. Multiple PDSA’s were conducted to optimize screening through increasing the reliability of the process. This included creation of an order set, and a required documentation checklist in the EMR of patients meeting eligibility criteria.
Results: Implementation of screening and data collection began in October 2020. After implementation, data from 10/2020 through 2/2021 showed an average weekly screening compliance of 76%. (Figure 1). Expansion of the inclusion criteria on 8/2021 resulted in a sharp decrease in compliance. Subsequently, addition of the documentation checklist in the EMR resulted in a center line shift in the data, with a current average weekly screening compliance of 59%. An average of 60% of all eligible NICU patients received a delirium screen prior to discharge (Figure 2).Conclusion(s): Through this QI project, we have increased awareness of neonatal delirium as a diagnosis in our NICU. Our expectation is that early recognition of delirium in our chronic patients will lead to more timely management of symptoms and decreased use of narcotic and sedative medications.
Figure 1
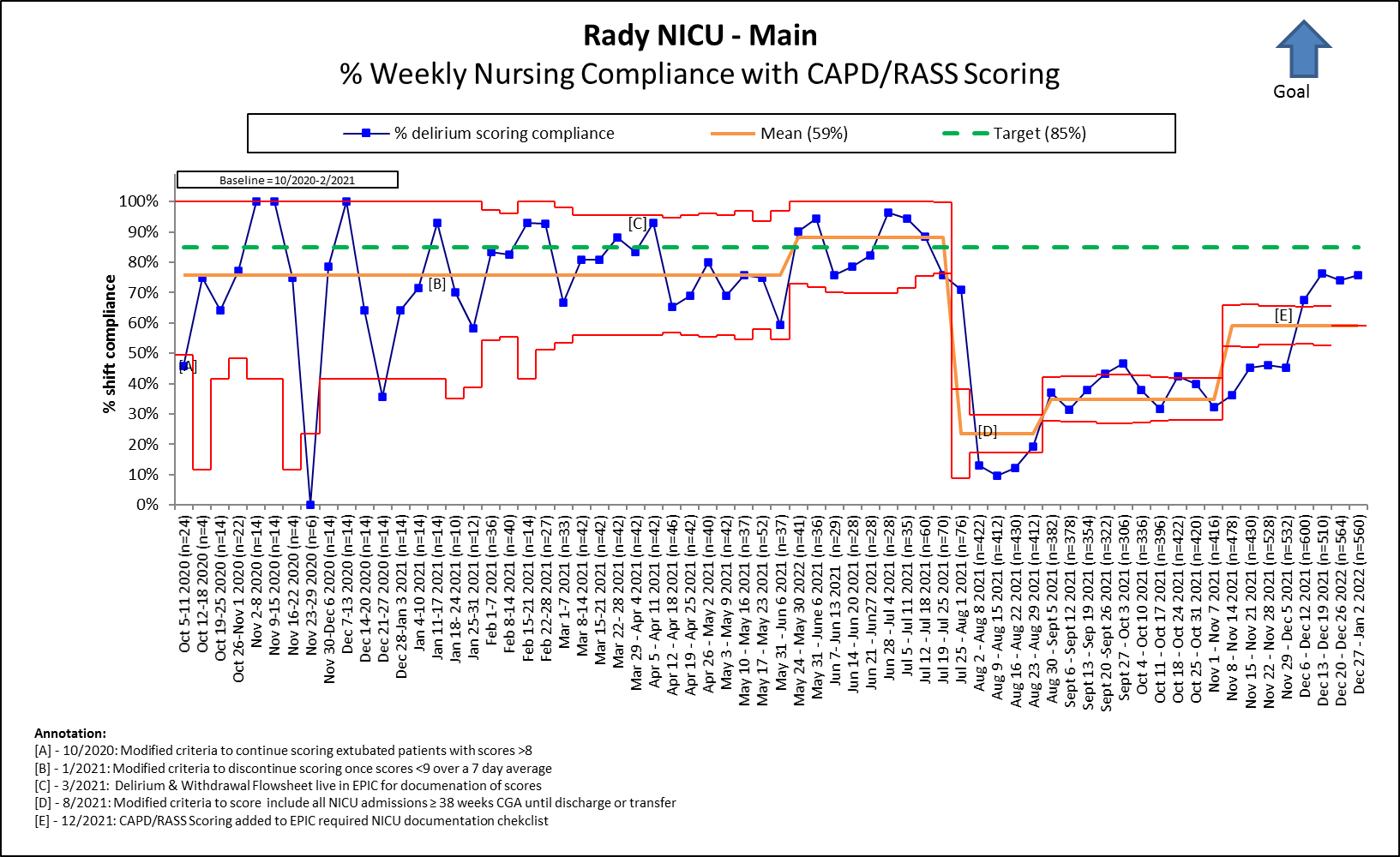 Weekly nursing compliance of Delirium screening.
Weekly nursing compliance of Delirium screening.Figure 2
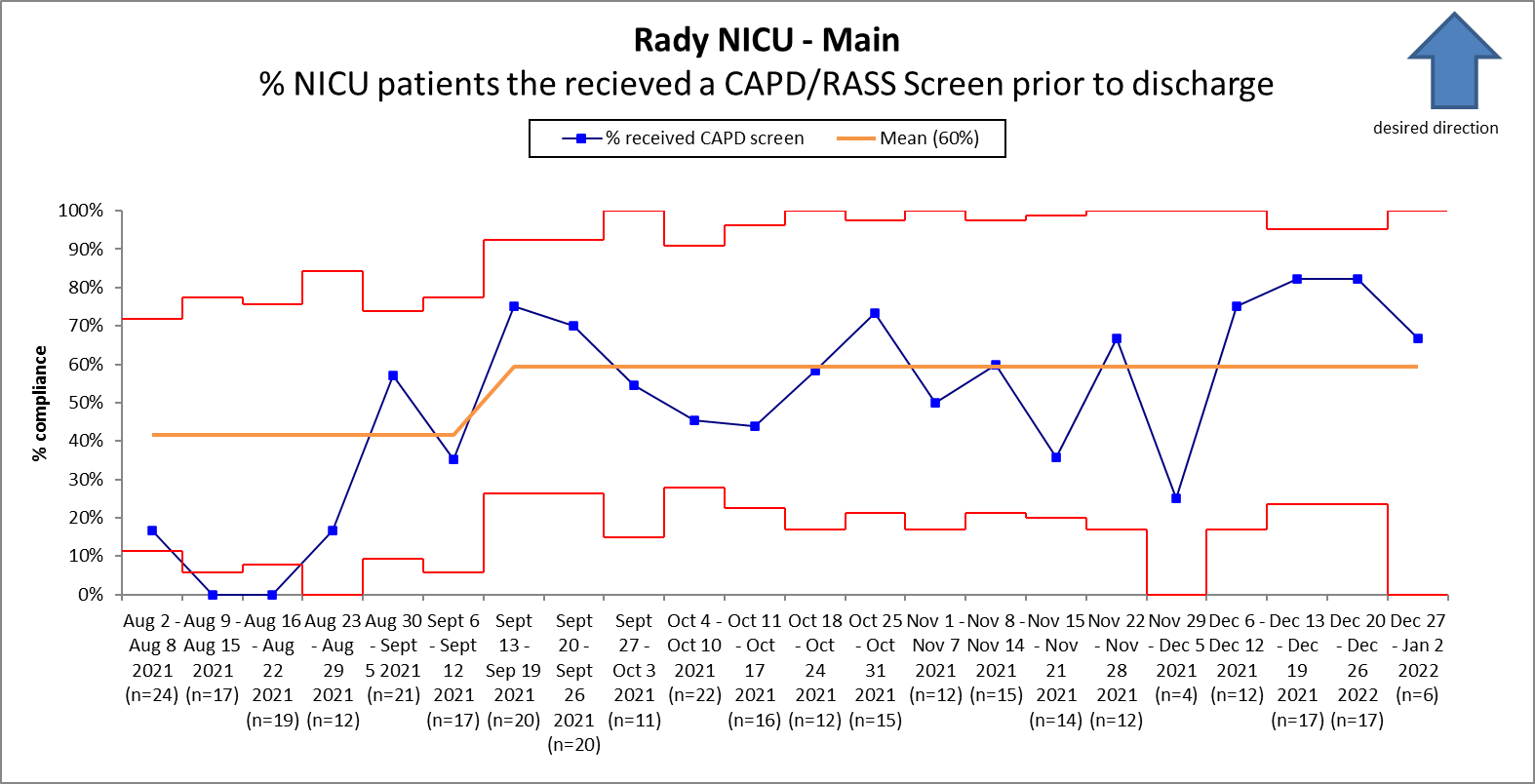 Percentage of NICU Patients receiving a Delirium screen prior to discharge.
Percentage of NICU Patients receiving a Delirium screen prior to discharge.