Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement II: Neurology and Infection
222 - Improved outcomes with Eat-Sleep-Console QI project in infants with NAS and the impact of the pandemic
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 222
Rachel Pham, Creighton University School of Medicine, Phoenix, AZ, United States; Sarah M. Small, Creighton University School of Medicine, Phoenix, AZ, United States; Meghan Turbenson, St. Joseph's Hospital and Medical Center, Phoenix, AZ, United States; Zoe R. Coleman, Dignity Health - St. Joseph's Hospital and Medical Center, Phoenix, AZ, United States; Vinit Manuel, ALLEGHENY CLINIC/AHN, Pittsburgh, PA, United States; Hemananda K. Muniraman, Phoenix Children's Hospital, PHOENIX, AZ, United States

Rachel Pham, BS
Medical Student
Creighton University School of Medicine
Phoenix, Arizona, United States
Presenting Author(s)
Background: Eat Sleep and Console (ESC), a functional-based assessment tool has been recently validated for the evaluation of infants with neonatal abstinence syndrome (NAS) and has been shown to improve outcomes with a decrease in the use of opioids and hospital length of stay (LOS) . We implemented a comprehensive quality improvement program with ESC protocol in March 2019 with emphasis on the promotion of functional-based assessment, parental presence at the bedside, and use of non-pharmacological intervention in infants with NAS.
Objective: Our specific aim was to decrease pharmacological treatment and LOS by 50% in 12 months. Following implementation, we compared outcome measures between pre-ESC and post-ESC cohorts and evaluated the impact of the current COVID-19 pandemic on the ESC program and outcomes.
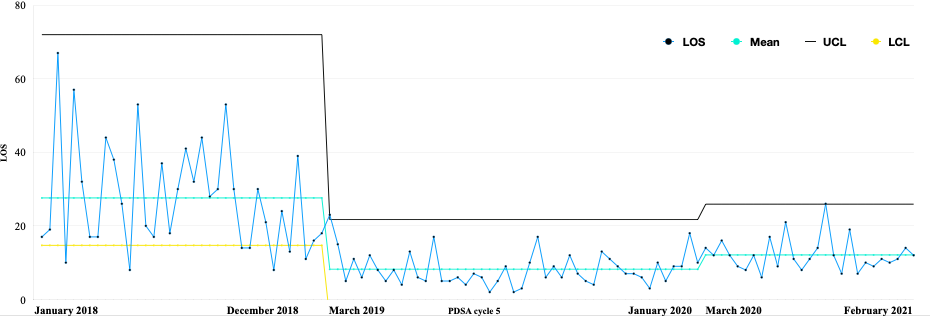
Design/Methods: Quality improvement process with prospective collection of data on outcomes, measures, and process. We compared LOS, pharmacologic treatment, hospital costs, and discharge home with parents. The outcomes were compared across three periods: pre-ESC (January 1st, 2018-December 31st, 2018), post-ESC (March 1st, 2019-January 31st, 2020), and the COVID-19 pandemic period (March 21st 2020-February 28th 2021).
Results: A total of 712 infants with intrauterine drug exposure were born during the study period, of which 109 term infants met the inclusion criteria of primary diagnosis of NAS (Pre-ESC cohort: 36, Post-ESC cohort: 47, and Pandemic period cohort: 26). There were no differences in maternal and infant characteristics, however, there was an increase in maternal fentanyl use seen in the pandemic period cohort. (Table) Use of pharmacological treatment decreased in the first year after implementation of the ESC program (44.7% vs 97.2%, p < 0.01). However, there was an increase to 76.7% in the second year during the pandemic. Similarly, mean LOS (8 vs 27), days of opioid treatment (2 vs 20), cumulative doses of opioids, and hospital costs decreased in the first year after implementation but increased during the pandemic period. (Table and figure).Conclusion(s): A functional, rather than symptom-based, assessment tool and prioritization of non-pharmacological interventions via ESC program led to a significant decrease in length of stay and opioid use in infants with NAS with reduced hospital costs. However, the current pandemic affected the resources and impacted some of the gains made in the first year of implementation of the ESC program.
Control chart: Length of stay over three year time period.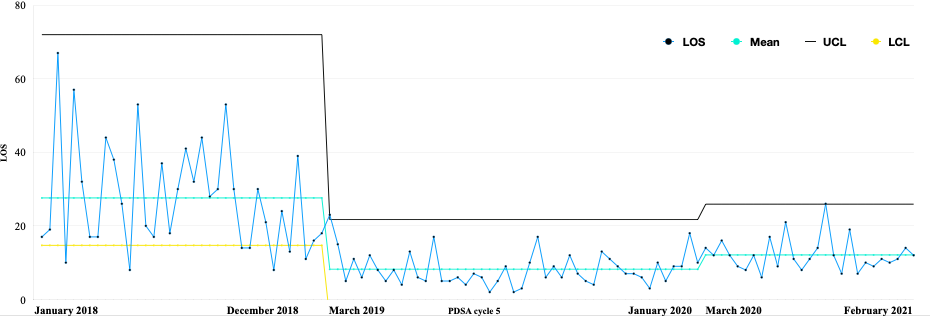
Objective: Our specific aim was to decrease pharmacological treatment and LOS by 50% in 12 months. Following implementation, we compared outcome measures between pre-ESC and post-ESC cohorts and evaluated the impact of the current COVID-19 pandemic on the ESC program and outcomes.
Design/Methods: Quality improvement process with prospective collection of data on outcomes, measures, and process. We compared LOS, pharmacologic treatment, hospital costs, and discharge home with parents. The outcomes were compared across three periods: pre-ESC (January 1st, 2018-December 31st, 2018), post-ESC (March 1st, 2019-January 31st, 2020), and the COVID-19 pandemic period (March 21st 2020-February 28th 2021).
Results: A total of 712 infants with intrauterine drug exposure were born during the study period, of which 109 term infants met the inclusion criteria of primary diagnosis of NAS (Pre-ESC cohort: 36, Post-ESC cohort: 47, and Pandemic period cohort: 26). There were no differences in maternal and infant characteristics, however, there was an increase in maternal fentanyl use seen in the pandemic period cohort. (Table) Use of pharmacological treatment decreased in the first year after implementation of the ESC program (44.7% vs 97.2%, p < 0.01). However, there was an increase to 76.7% in the second year during the pandemic. Similarly, mean LOS (8 vs 27), days of opioid treatment (2 vs 20), cumulative doses of opioids, and hospital costs decreased in the first year after implementation but increased during the pandemic period. (Table and figure).Conclusion(s): A functional, rather than symptom-based, assessment tool and prioritization of non-pharmacological interventions via ESC program led to a significant decrease in length of stay and opioid use in infants with NAS with reduced hospital costs. However, the current pandemic affected the resources and impacted some of the gains made in the first year of implementation of the ESC program.
Control chart: Length of stay over three year time period.