Back
Global Neonatal & Children's Health
Category: Abstract Submission
Global Child and Adolescent Health I
142 - In-Hospital Mortality and its Predictors in Very Low Birthweight Infants Managed in Tertiary Hospitals in Nigeria
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 142
Publication Number: 142.111
Publication Number: 142.111
Osayame A. Ekhaguere, Indiana University School of Medicine, Carmel, IN, United States; Iretiola B. Fajolu, University of Lagos, Lagos, Lagos, Nigeria; Ikechukwu R. Okonkwo, UBTH, Benin Ciyy, Edo, Nigeria; Amsa B. Mairami, National Hospital Abuja, Abuja, Federal Capital Territory, Nigeria

Osayame A. Ekhaguere, M.D., MPH
Neonatologist
Riley Hospital for Children at Indiana Univeristy Health
Carmel, IN, United States
Presenting Author(s)
Background: In-hospital mortality of very low birth weight (VLBW) infants (birth weight less than 1500 grams) is a benchmark for tertiary care type and quality. Data from low-resourced centers on in-hospital mortality of VLBWs are sparse
Objective: Describe rate, causes, and predictors of in-hospital VLBW mortality in tertiary institutions in Nigeria.
Design/Methods: A retrospective cohort study on clinical predictors of in-hospital mortality of VLBW admitted within 72 hours of life into three tertiary centers neonatal intensive care units (NICUs) in Nigeria from July 2017 to March 2021. Descriptive statistics were used to present mortality rates, causes, and timing of death and multivariate logistic analysis to identify some independent predictors of in-hospital mortality
Results: Of the 6187 NICU admission, 1161 met inclusion criteria. There were 545 (47%) in-hospital VLBW deaths recorded. Respiratory distress syndrome accounted for 57% (309) of the mortalities, and 55% of all mortalities occurred within 72 hours of life. The adjusted odds (aOR) of mortality was higher in males compared to females (aOR 3.013, 95% confidence interval (CI) 1.846 to 4.917), with cesarean compared to vaginal deliveries (aOR 1.562 95% CI 1.086 to 2.248), in patients with intraventricular hemorrhage (aOR 3.638 95% CI 1.566 to 8.453) and each point increase in Downs respiratory distress score (aOR 1.256 95% CI 1.128 to 1.398). The risk of mortality varied significantly amongst sites, as did the use of evidence-based neonatal interventions like surfactant, mechanical ventilation, and blended oxygenConclusion(s): In-hospital VLBW neonatal mortality in low-resource settings is high and varies significantly. Research on implementing evidence-based interventions to address modifiable risk factors is needed
Neonatal and maternal demographic and clinical characteristics by study outcome; survived to or died before hospital discharge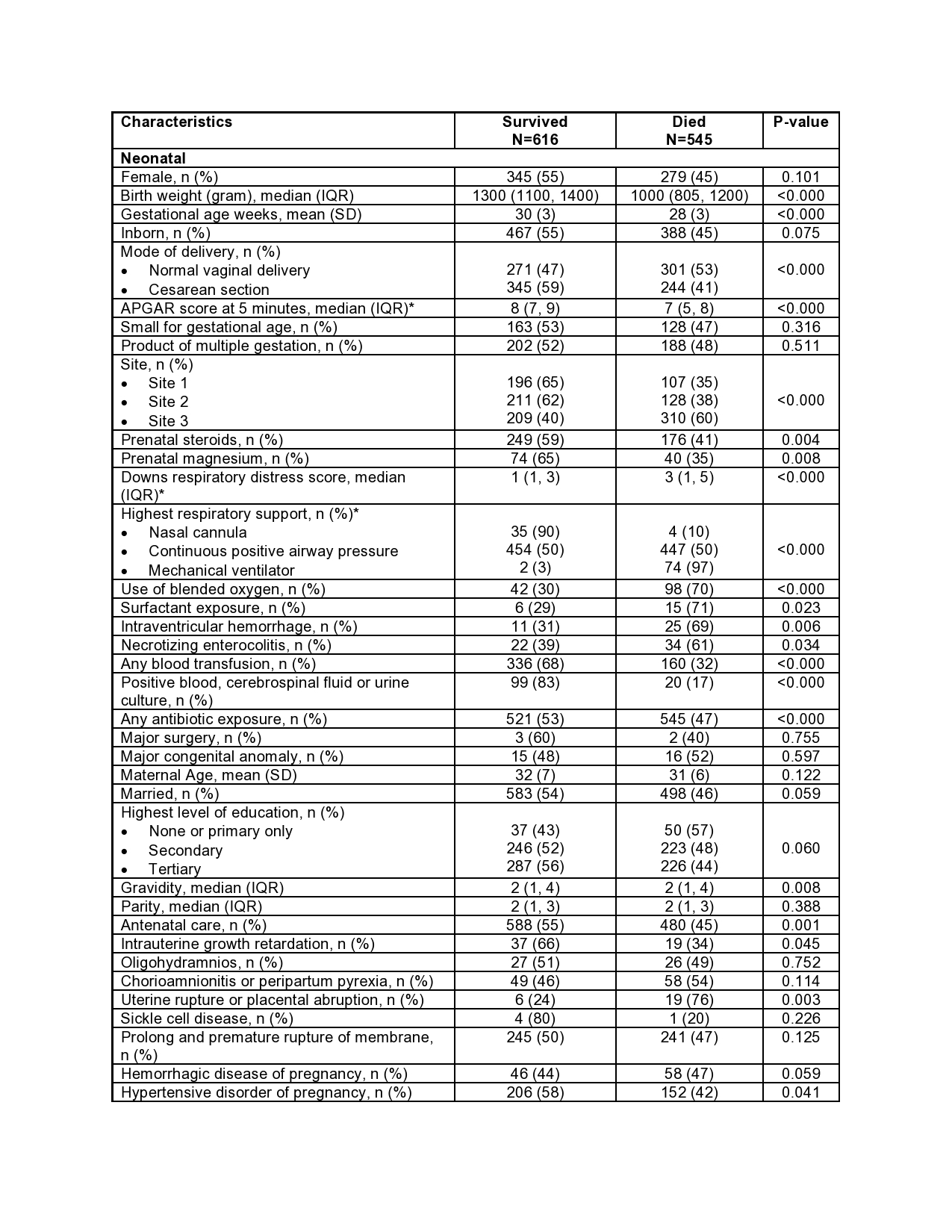 *Variables with ≥10% missing values
*Variables with ≥10% missing values
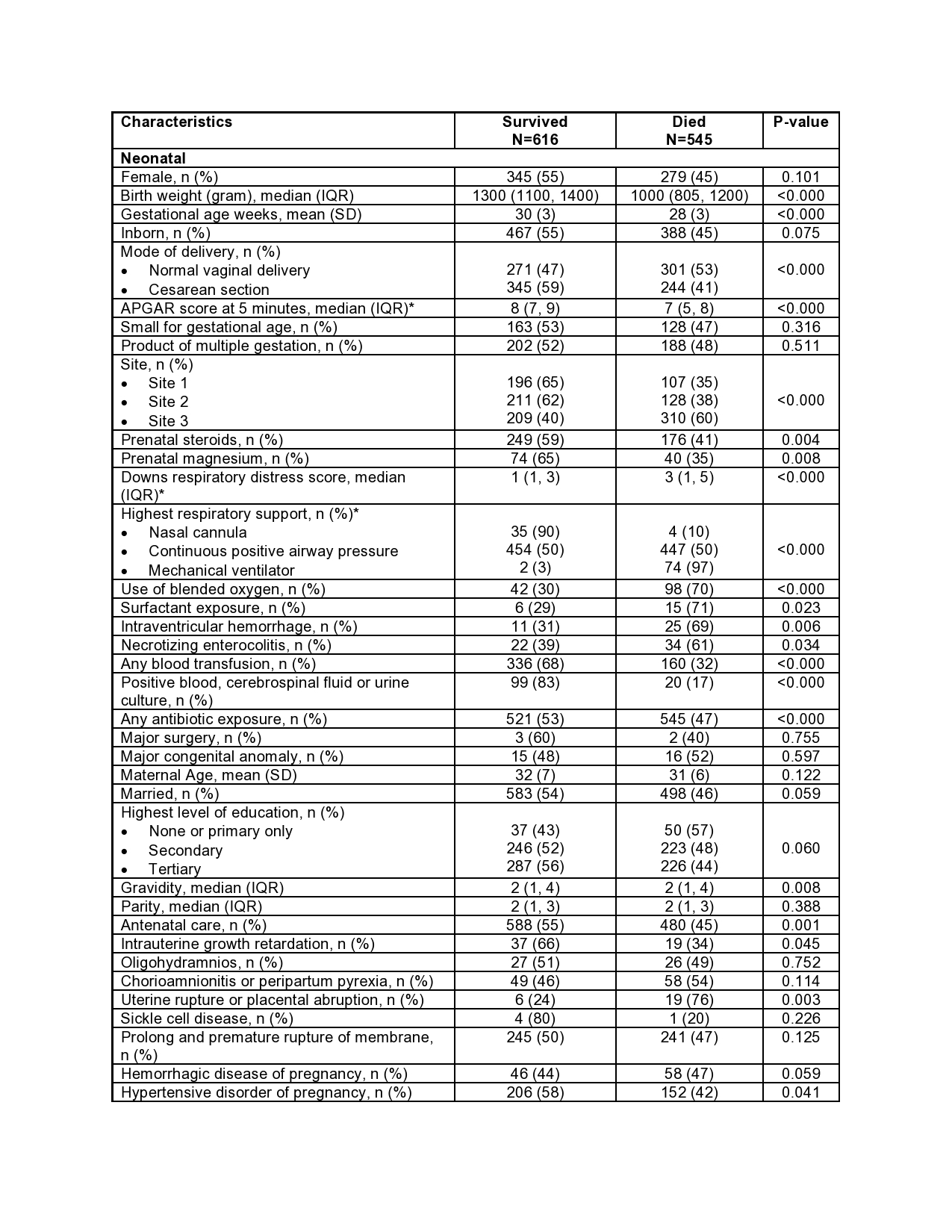
Multivariate logistic regression analysis for the predictor of in-hospital mortality in very low birth weight infants.jpg) *Mechanical ventilator exposure was not included in the model due to a lack of convergence. Almost all subjects placed on the ventilator died
*Mechanical ventilator exposure was not included in the model due to a lack of convergence. Almost all subjects placed on the ventilator died
Objective: Describe rate, causes, and predictors of in-hospital VLBW mortality in tertiary institutions in Nigeria.
Design/Methods: A retrospective cohort study on clinical predictors of in-hospital mortality of VLBW admitted within 72 hours of life into three tertiary centers neonatal intensive care units (NICUs) in Nigeria from July 2017 to March 2021. Descriptive statistics were used to present mortality rates, causes, and timing of death and multivariate logistic analysis to identify some independent predictors of in-hospital mortality
Results: Of the 6187 NICU admission, 1161 met inclusion criteria. There were 545 (47%) in-hospital VLBW deaths recorded. Respiratory distress syndrome accounted for 57% (309) of the mortalities, and 55% of all mortalities occurred within 72 hours of life. The adjusted odds (aOR) of mortality was higher in males compared to females (aOR 3.013, 95% confidence interval (CI) 1.846 to 4.917), with cesarean compared to vaginal deliveries (aOR 1.562 95% CI 1.086 to 2.248), in patients with intraventricular hemorrhage (aOR 3.638 95% CI 1.566 to 8.453) and each point increase in Downs respiratory distress score (aOR 1.256 95% CI 1.128 to 1.398). The risk of mortality varied significantly amongst sites, as did the use of evidence-based neonatal interventions like surfactant, mechanical ventilation, and blended oxygenConclusion(s): In-hospital VLBW neonatal mortality in low-resource settings is high and varies significantly. Research on implementing evidence-based interventions to address modifiable risk factors is needed
Neonatal and maternal demographic and clinical characteristics by study outcome; survived to or died before hospital discharge
 *Variables with ≥10% missing values
*Variables with ≥10% missing valuesMultivariate logistic regression analysis for the predictor of in-hospital mortality in very low birth weight infants
.jpg) *Mechanical ventilator exposure was not included in the model due to a lack of convergence. Almost all subjects placed on the ventilator died
*Mechanical ventilator exposure was not included in the model due to a lack of convergence. Almost all subjects placed on the ventilator died