Neonatal General
Category: Abstract Submission
Neonatology General 5
406 - Maternal Perceptions of Optimism and Gratitude Associate with Vagal Tone and Stress Resilience
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 406
Publication Number: 406.135
Publication Number: 406.135
Fumiyuki C. Gardner, Pennsylvania State University College of Medicine, New Cumberland, PA, United States; Liz M. Sanchez Pena, Penn State College of Medicine, Lebanon, PA, United States; Brittany J. Fronheiser, Pennsylvania State University College of Medicine, Camp Hill, PA, United States; Gina Brelsford, Penn State Harrisburg, Middletown, PA, United States; Kim K. Doheny, Penn State College of Medicine and Penn State Children's Hospital, Hershey, PA, United States
Fumiyuki C. Gardner, Ph.D. (she/her/hers)
Research Specialist
Penn State College of Medicine
The Pennsylvania State University
Hershey, Pennsylvania, United States
Presenting Author(s)
Background: Mothers commonly express concern related to the unique challenges of parenting their preterm born infant. It is well known that mothers’ stress processing and associated psychological well-being influence maternal-infant interactions; thus, it is important to determine factors that may identify mothers at risk. Mothers’ perceptions and stress reactivity suggest how well they are coping at home. Vagal tone measured as high frequency heart rate variability (HF-HRV) has been studied as a stress resilience factor; however, its associations with perceptions regarding the NICU experience have not been well-studied in mothers post-discharge.
Objective: Explore differences in perceptions and stress responses in former NICU mothers.
Design/Methods: A cross-sectional cohort of 29 mothers of preterm born infants was enrolled, excluding those with conditions of autonomic dysfunction. For stress induction, mothers performed a Trier Social Stress Test including 5-min each of mental recall of the NICU experience, oral narration, and mental arithmetic. Vagal tone (HF-HRV) measured continuously by MindWare Mobile Impedance Cardiograph was analyzed by frequency domain. Mothers’ narratives were analyzed qualitatively. Distress Thermometer-Parent was administered to quantify distress within the past week.
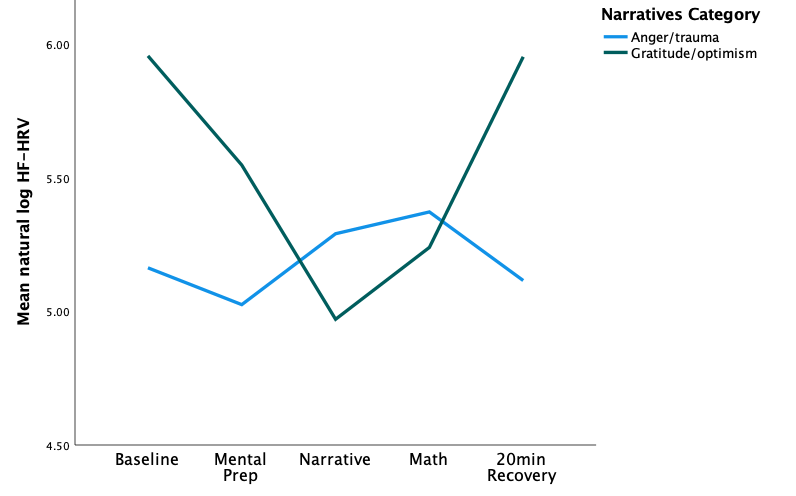
Results: Six mothers expressed gratitude and optimism (GO), 7 mothers expressed anger and trauma (AT), and 16 mothers were vague in emotional expression. GO mothers showed higher HF-HRV at baseline and post-stress vs. AT (Figure 1). For both GO and AT, HF-HRV decreased with stress. Change scores from baseline to narrative, and narrative to post-stress were higher in GO vs. AT (p=.04 and p=.02 respectively). Moreover, HF-HRV increased from narrative to post-stress [t(11)=2.29, p=.04] for GO only. AT reported higher distress compared to GO. Conclusion(s): Mothers with expressions of gratitude and optimism about their NICU experience showed higher vagal tone (HF-HRV), than mothers expressing anger and trauma as the predominant theme of their narrative. These findings suggest that helping mothers to articulate and reframe trauma to optimism and hopefulness supports higher vagal tone and stress resilience. Care providers should embrace opportunities for building stress resilience in parents through facilitative discussion and stress-processing of the NICU experience during hospitalization and post-discharge.
Funding: Children’s Miracle Network (GMB, KKD)
Figure 1: Mean HF-HRV in mothers who expressed anger/trauma and those who expressed gratitude/optimism when recounting their NICU experience.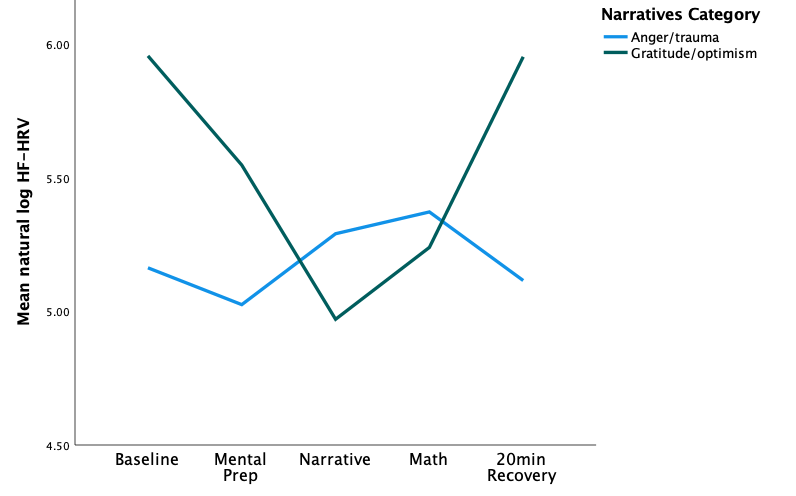
Objective: Explore differences in perceptions and stress responses in former NICU mothers.
Design/Methods: A cross-sectional cohort of 29 mothers of preterm born infants was enrolled, excluding those with conditions of autonomic dysfunction. For stress induction, mothers performed a Trier Social Stress Test including 5-min each of mental recall of the NICU experience, oral narration, and mental arithmetic. Vagal tone (HF-HRV) measured continuously by MindWare Mobile Impedance Cardiograph was analyzed by frequency domain. Mothers’ narratives were analyzed qualitatively. Distress Thermometer-Parent was administered to quantify distress within the past week.
Results: Six mothers expressed gratitude and optimism (GO), 7 mothers expressed anger and trauma (AT), and 16 mothers were vague in emotional expression. GO mothers showed higher HF-HRV at baseline and post-stress vs. AT (Figure 1). For both GO and AT, HF-HRV decreased with stress. Change scores from baseline to narrative, and narrative to post-stress were higher in GO vs. AT (p=.04 and p=.02 respectively). Moreover, HF-HRV increased from narrative to post-stress [t(11)=2.29, p=.04] for GO only. AT reported higher distress compared to GO. Conclusion(s): Mothers with expressions of gratitude and optimism about their NICU experience showed higher vagal tone (HF-HRV), than mothers expressing anger and trauma as the predominant theme of their narrative. These findings suggest that helping mothers to articulate and reframe trauma to optimism and hopefulness supports higher vagal tone and stress resilience. Care providers should embrace opportunities for building stress resilience in parents through facilitative discussion and stress-processing of the NICU experience during hospitalization and post-discharge.
Funding: Children’s Miracle Network (GMB, KKD)
Figure 1: Mean HF-HRV in mothers who expressed anger/trauma and those who expressed gratitude/optimism when recounting their NICU experience.