Back
Nephrology: Clinical
Category: Abstract Submission
Nephrology I: Potpourri
98 - Nephrotic syndrome in Children During the COVID-19 Pandemic
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 98
Publication Number: 98.138
Publication Number: 98.138
Aesha Maniar, Cohen Children's Medical Center, New Hyde Park, NY, United States; Jenelle Cocorpus, Cohen Children's Medical Center, New Hyde Park, NY, United States; Laura Castellanos Reyes, Cohen Children's Medical Center, New Hyde Park, NY, United States; Pamela Singer, Long Island Jewish Medical Center, New Hyde Park, NY, United States; Abby Basalely, Cohen Children's Medical Center, New Hyde Park, NY, United States; Christine Sethna, Cohen Children's Medical Center, New Hyde Park, NY, United States

Aesha Maniar, MD
Pediatric Resident
Cohen Children's Medical Center
Cohen Children's Medical Center
New Hyde Park, New York, United States
Presenting Author(s)
Background: SARS-CoV-2 is a respiratory virus that led to the global COVID-19 pandemic in 2020. Public health measures of mask wearing and social distancing decreased the incidence of common viruses among children. Given that nephrotic syndrome is often triggered by viral illnesses, the pandemic may have had an impact on the clinical features of nephrotic syndrome in children.
Objective: To characterize the effect of the COVID-19 pandemic on the epidemiology, clinical characteristics and health care utilization of children with nephrotic syndrome.
Design/Methods: This single center retrospective chart review compared the time period one year before (March 1 2019- Feb 28, 2020) and one year during the COVID-19 pandemic (March 1 2020- February 28, 2021). Children < 21 years followed with a diagnosis of nephrotic syndrome were included in the analysis. Epidemiologic events (new diagnoses, relapses), clinical characteristics (body mass index [BMI], blood pressure index, vitamin D level, urine protein:creatine [UPC]) and health care utilization (in-person office, telemedicine, hospital, emergency room [ED] visits) were compared pre-pandemic (PP) and during pandemic (DP) using paired t-test and Wilcoxon Rank Sum test.
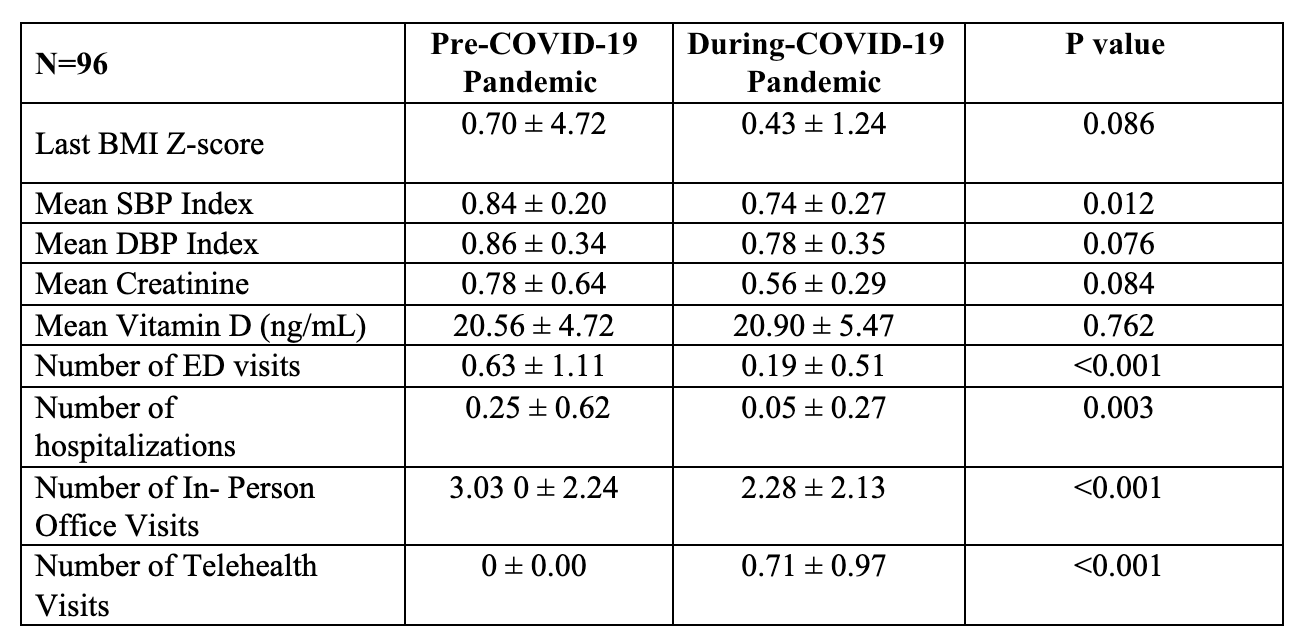
Results: There were 14 new diagnoses of nephrotic syndrome PP and 18 new diagnoses DP. Among 96 children followed PP and DP, the mean age was 10.7 ± 5.28 years, 64.6% were male and 14.6% were Black. Diagnoses included: 16.7% minimal change disease, 12.5 % focal segmental glomerulocsclerosis, 1% membranous nephropathy and 69.8% were not biopsied. 25% of patients were steroid sensitive, 54% were frequent relapsers and 20.8% were steroid resistant. Compared to the PP period, mean SBP index was significantly lower and there were fewer ED, hospital and in-person office visits in the DP period (Table 1). Telehealth visits were significantly greater DP compared to PP. Children with steroid sensitive/frequent relapsing nephrotic syndrome had significantly lower number of relapses DP (0.59 ± 095) compared to PP (1.27 ± 1.53), p < 0.001. For children with steroid resistant nephrotic syndrome, there was no significant difference in mean UPC DP (3.92 ± 9.94) compared to PP (3.70 ±6.54), p=0.14.Conclusion(s): There was less in-person healthcare utilization and more telehealth utilization DP compared to PP in children with nephrotic syndrome. There were also fewer relapses DP compared to PP likely due to fewer viral illnesses from public health measures during the pandemic.
Overall Epidemiology, Clinical Characteristics and Health Care Utilization in Children with Nephrotic Syndrome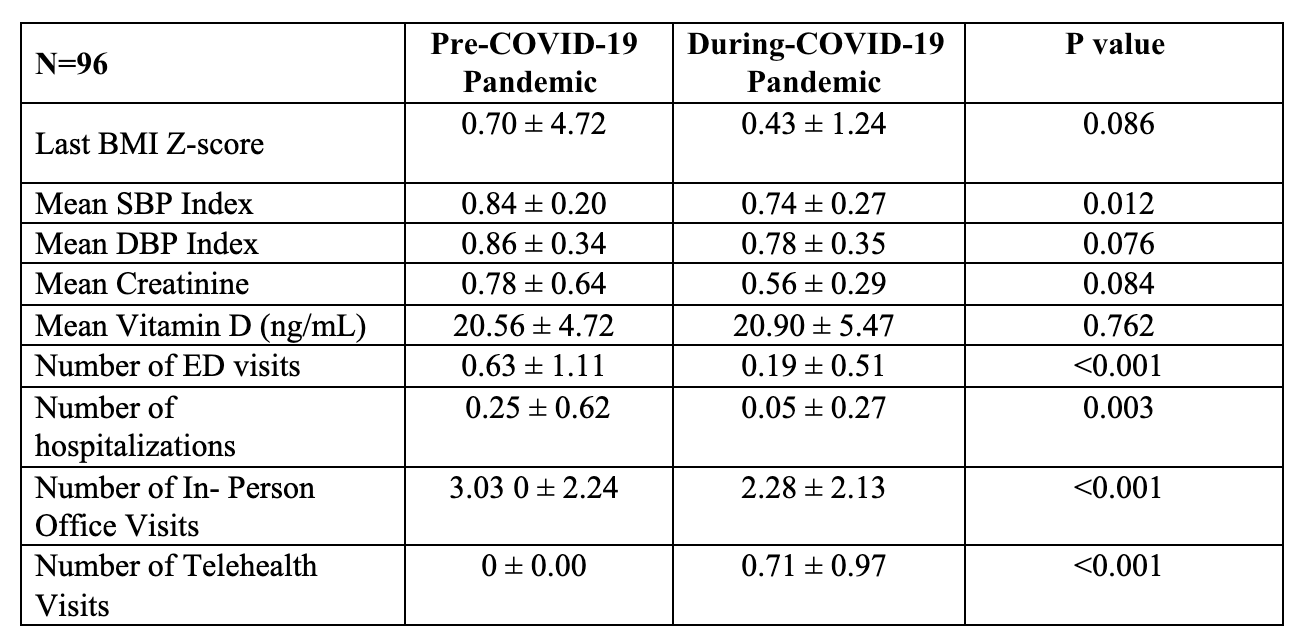
Objective: To characterize the effect of the COVID-19 pandemic on the epidemiology, clinical characteristics and health care utilization of children with nephrotic syndrome.
Design/Methods: This single center retrospective chart review compared the time period one year before (March 1 2019- Feb 28, 2020) and one year during the COVID-19 pandemic (March 1 2020- February 28, 2021). Children < 21 years followed with a diagnosis of nephrotic syndrome were included in the analysis. Epidemiologic events (new diagnoses, relapses), clinical characteristics (body mass index [BMI], blood pressure index, vitamin D level, urine protein:creatine [UPC]) and health care utilization (in-person office, telemedicine, hospital, emergency room [ED] visits) were compared pre-pandemic (PP) and during pandemic (DP) using paired t-test and Wilcoxon Rank Sum test.
Results: There were 14 new diagnoses of nephrotic syndrome PP and 18 new diagnoses DP. Among 96 children followed PP and DP, the mean age was 10.7 ± 5.28 years, 64.6% were male and 14.6% were Black. Diagnoses included: 16.7% minimal change disease, 12.5 % focal segmental glomerulocsclerosis, 1% membranous nephropathy and 69.8% were not biopsied. 25% of patients were steroid sensitive, 54% were frequent relapsers and 20.8% were steroid resistant. Compared to the PP period, mean SBP index was significantly lower and there were fewer ED, hospital and in-person office visits in the DP period (Table 1). Telehealth visits were significantly greater DP compared to PP. Children with steroid sensitive/frequent relapsing nephrotic syndrome had significantly lower number of relapses DP (0.59 ± 095) compared to PP (1.27 ± 1.53), p < 0.001. For children with steroid resistant nephrotic syndrome, there was no significant difference in mean UPC DP (3.92 ± 9.94) compared to PP (3.70 ±6.54), p=0.14.Conclusion(s): There was less in-person healthcare utilization and more telehealth utilization DP compared to PP in children with nephrotic syndrome. There were also fewer relapses DP compared to PP likely due to fewer viral illnesses from public health measures during the pandemic.
Overall Epidemiology, Clinical Characteristics and Health Care Utilization in Children with Nephrotic Syndrome