Back
Adolescent Medicine: General
Category: Abstract Submission
Adolescent Medicine II
502 - Pediatrician, Adolescent, and Caregiver Perspectives on STI Screening in Primary Care
Friday, April 22, 2022
6:15 PM – 8:45 PM US MT
Poster Number: 502
Publication Number: 502.100
Publication Number: 502.100
Fahd A. Ahmad, Washington University in St. Louis, St. Louis, MO, United States; Viani Dickey, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Emmanuel K. Tetteh, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Virginia R. McKay, Washington University in St Louis, St. Louis, MO, United States
- FA
Fahd A. Ahmad, MD, MSCI
Associate Professor of Pediatrics
Washington University in St. Louis
St. Louis, Missouri, United States
Presenting Author(s)
Background: Adolescents bear a disproportionate burden of sexually transmitted infections (STIs), yet STI screening is infrequently performed in pediatric primary care, with many at-risk patients not receiving STI testing. We have previously implemented a risk-based STI screening program in our pediatric emergency department, and aim to adapt and implement this program in pediatric primary care clinics.
Objective: The purpose of this study is to understand contextual factors influencing STI screening and testing among adolescents in these practices, informing our future implementation of this program.
Design/Methods: We conducted semi-structured interviews with 23 physicians and clinic staff, and 12 patient-caregiver dyads from four pediatric primary care practices in our area about practices and concerns related to STI screening. Qualitative analysis was conducted using a categorical coding technique guided by the Consolidated Framework for Implementation Research (CFIR).
Results: We recruited 23 physicians and clinic staff, and 12 patient-parent dyads. While participants did not endorse resistance to STI screening, we did identify multiple barriers to doing so. In alignment the CFIR domains, we present them at the individual level and the level of the inner setting and implementation process. Tables 1-3 provide representative quotes from each CFIR domain.
Individual level barriers to STI screening and testing included variability in clinicians’ practice patterns and their perception of STI risk in their patients. Physicians’ estimates of proportion of adolescents in their practice that are sexually active ranged from 10-95%, with estimates of sexually active patients at risk for STIs ranging from 25-100%.
Intervention level barriers centered on screening for STI risk factors not being a routine part of their process. Inner setting and implementation process barriers included time constraints during visits and a lack of capacity to perform testing. Nurses were rarely involved when screening did occur, with their role usually limited to urine sample collection. Confidentiality concerns created significant barriers to screening and testing on both individual and inner setting levels. Adopting confidential methods for testing and educating providers on patients’ recommendations for STI testing were discussed as ways to potentially improve STI care in pediatric patients.Conclusion(s): Our findings highlight a need to improve STI care in adolescents. An integrated approach that enhances patient confidentiality and improves clinicians’ knowledge could address gaps in STI care in pediatric primary care settings.
Table 1. Examples Quotes from CFIR Individual Patient Domain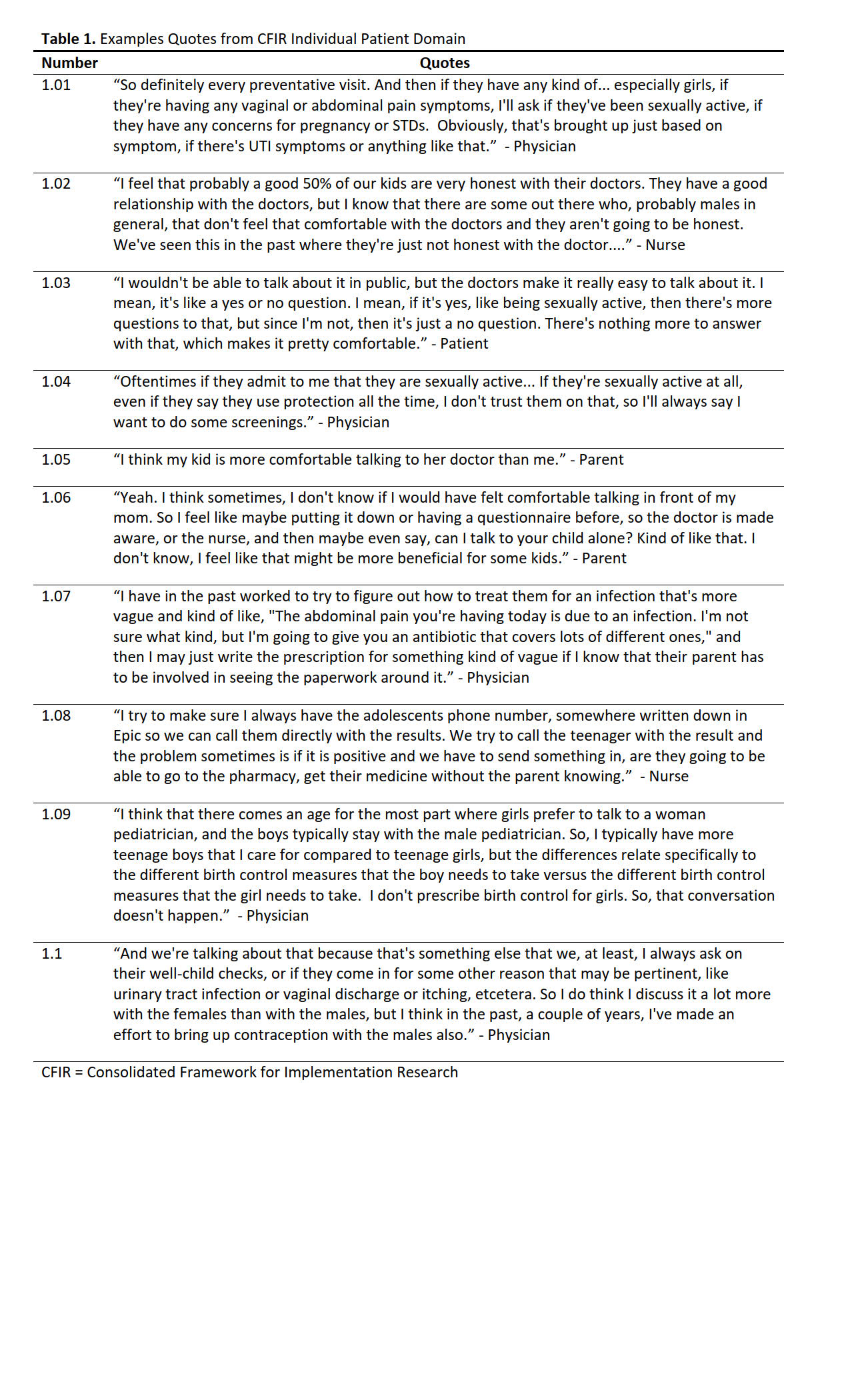 CFIR = Consolidated Framework for Implementation Research
CFIR = Consolidated Framework for Implementation Research
Table 2. Example Quotes from CFIR Intervention Domain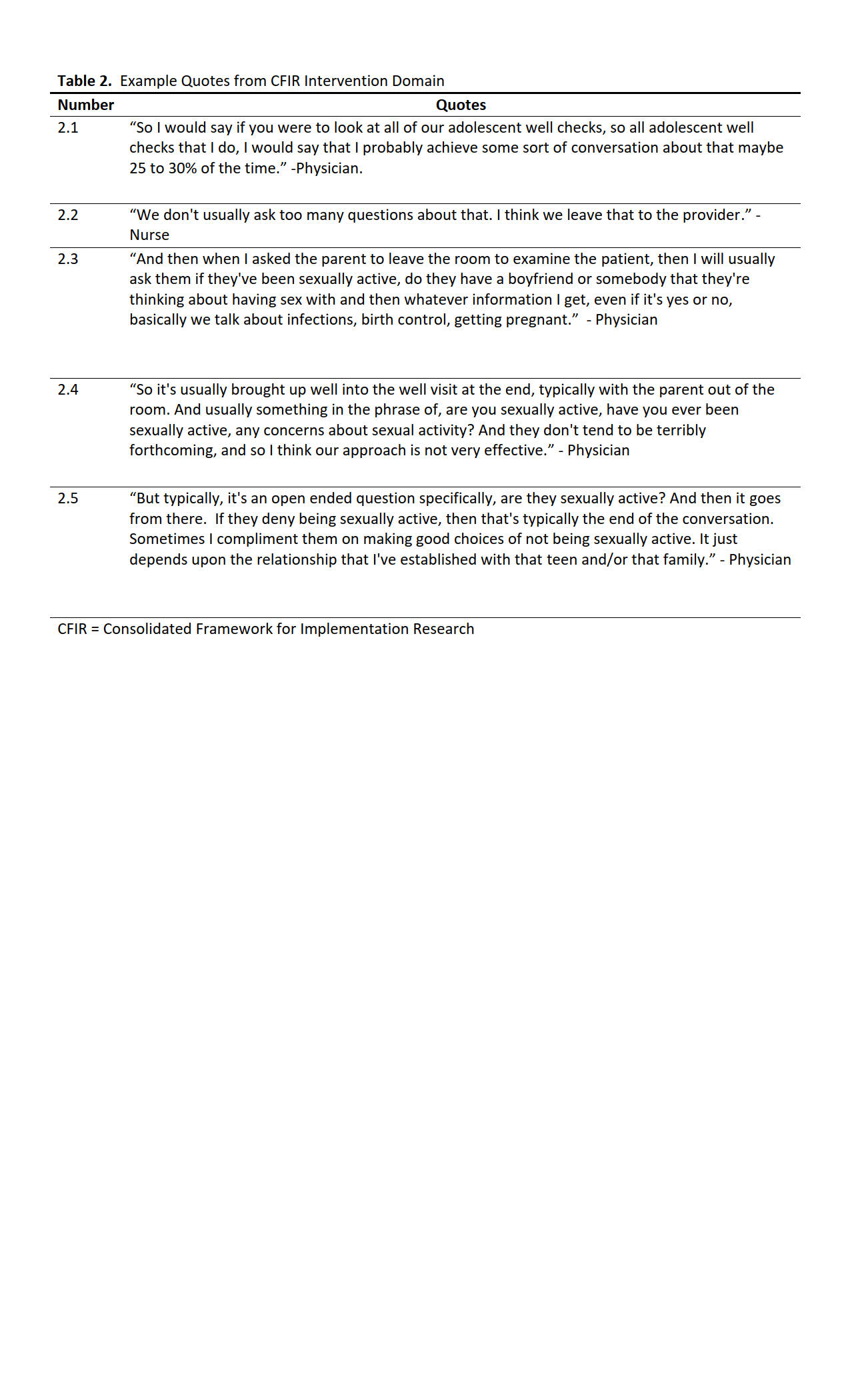 CFIR = Consolidated Framework for Implementation Research
CFIR = Consolidated Framework for Implementation Research
Objective: The purpose of this study is to understand contextual factors influencing STI screening and testing among adolescents in these practices, informing our future implementation of this program.
Design/Methods: We conducted semi-structured interviews with 23 physicians and clinic staff, and 12 patient-caregiver dyads from four pediatric primary care practices in our area about practices and concerns related to STI screening. Qualitative analysis was conducted using a categorical coding technique guided by the Consolidated Framework for Implementation Research (CFIR).
Results: We recruited 23 physicians and clinic staff, and 12 patient-parent dyads. While participants did not endorse resistance to STI screening, we did identify multiple barriers to doing so. In alignment the CFIR domains, we present them at the individual level and the level of the inner setting and implementation process. Tables 1-3 provide representative quotes from each CFIR domain.
Individual level barriers to STI screening and testing included variability in clinicians’ practice patterns and their perception of STI risk in their patients. Physicians’ estimates of proportion of adolescents in their practice that are sexually active ranged from 10-95%, with estimates of sexually active patients at risk for STIs ranging from 25-100%.
Intervention level barriers centered on screening for STI risk factors not being a routine part of their process. Inner setting and implementation process barriers included time constraints during visits and a lack of capacity to perform testing. Nurses were rarely involved when screening did occur, with their role usually limited to urine sample collection. Confidentiality concerns created significant barriers to screening and testing on both individual and inner setting levels. Adopting confidential methods for testing and educating providers on patients’ recommendations for STI testing were discussed as ways to potentially improve STI care in pediatric patients.Conclusion(s): Our findings highlight a need to improve STI care in adolescents. An integrated approach that enhances patient confidentiality and improves clinicians’ knowledge could address gaps in STI care in pediatric primary care settings.
Table 1. Examples Quotes from CFIR Individual Patient Domain
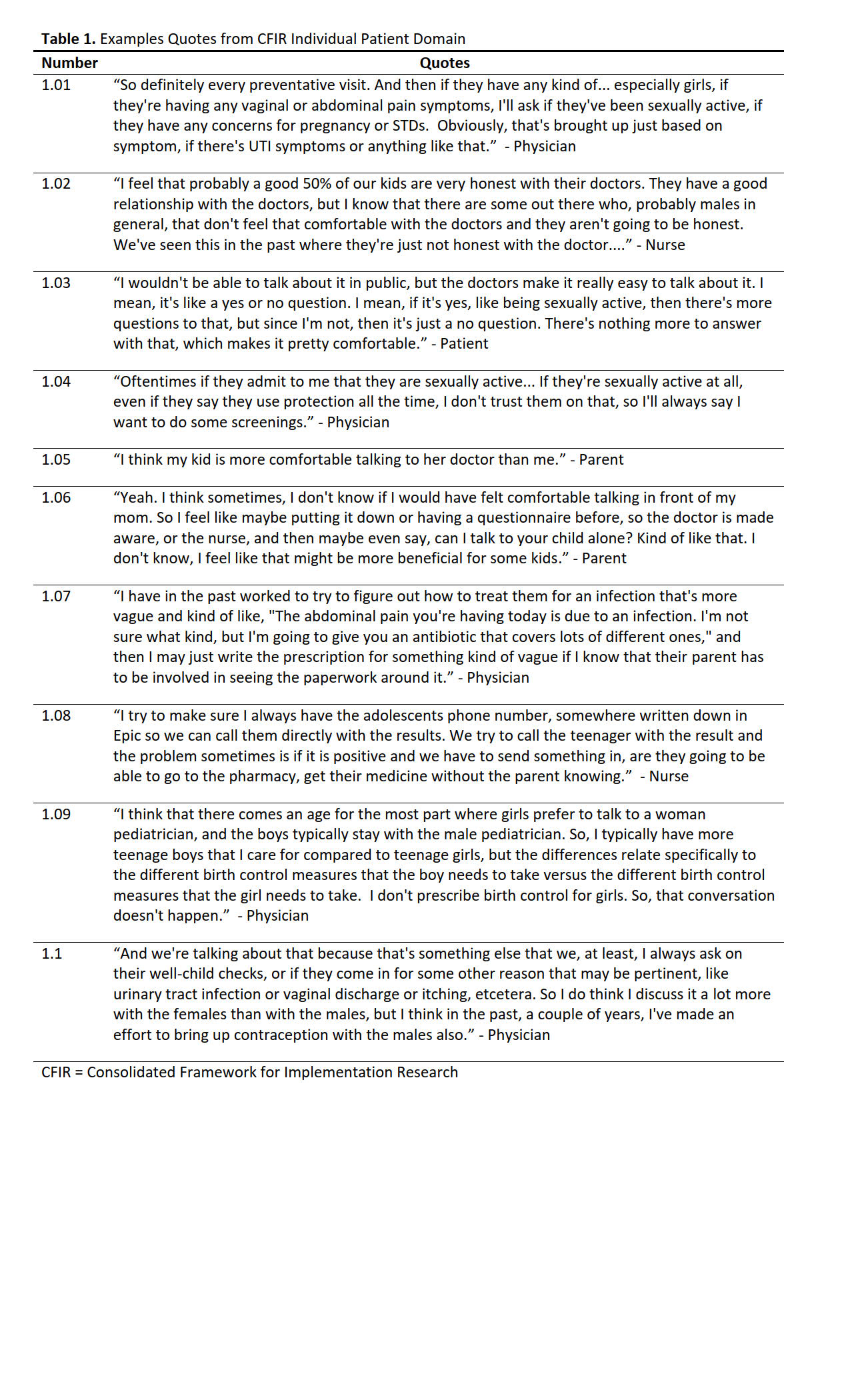 CFIR = Consolidated Framework for Implementation Research
CFIR = Consolidated Framework for Implementation ResearchTable 2. Example Quotes from CFIR Intervention Domain
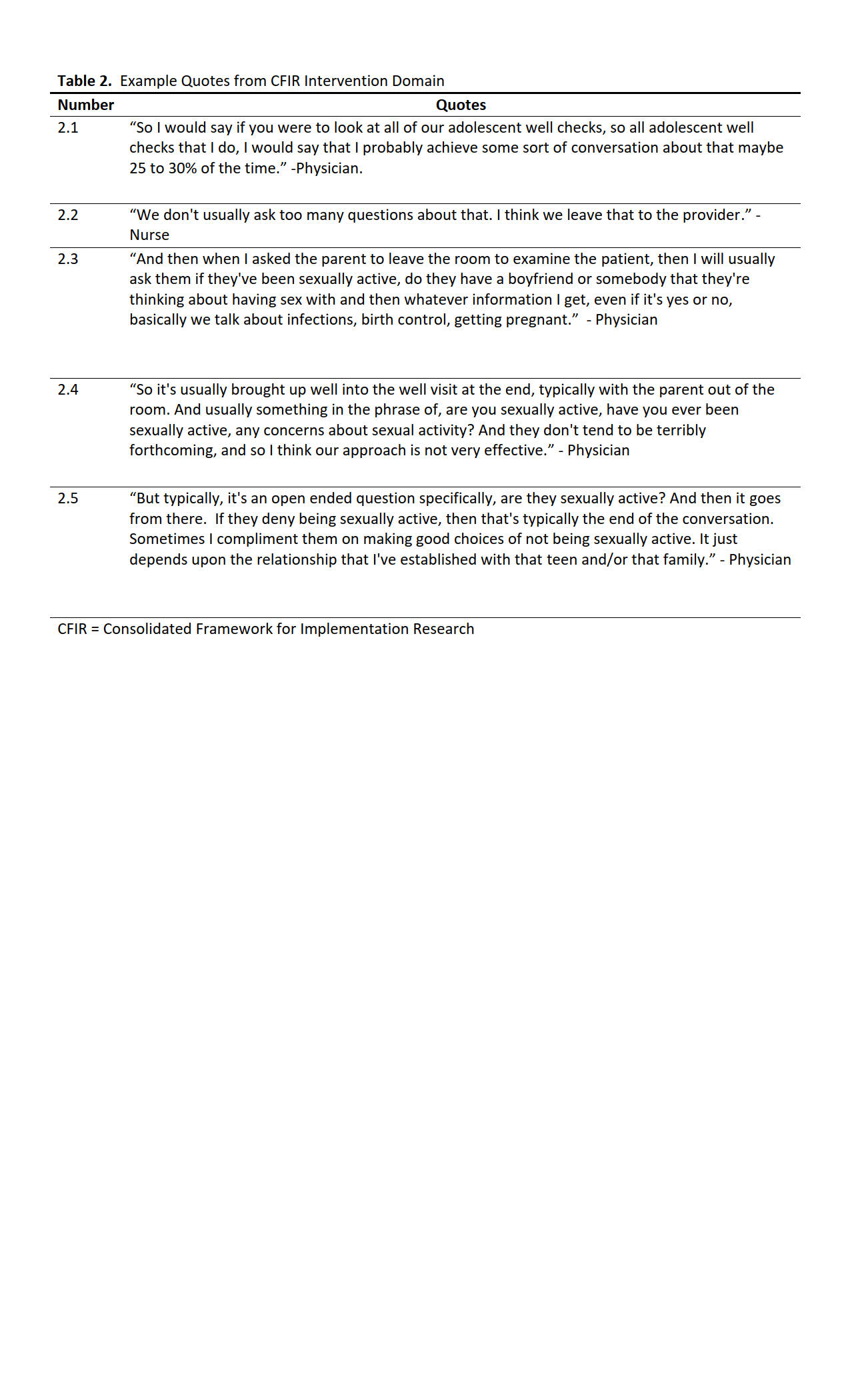 CFIR = Consolidated Framework for Implementation Research
CFIR = Consolidated Framework for Implementation Research