Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: CMV, HIV, Syphilis, Immunology
318 - Persistent elevation of soluble IL-2 receptor alpha contributes to lymphopenia in extremely premature infants with capillary leak syndrome
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 318
Publication Number: 318.124
Publication Number: 318.124
Timothy J. Boly, University of Iowa Hospitals and Clinics, Iowa City, IA, United States; Austin Paden, University of Iowa Stead Family Children's Hospital, Iowa City, IA, United States; Jennifer Bermick, University of Iowa, Iowa City, IA, United States

Timothy J. Boly, DO (he/him/his)
Instructor of Pediatrics
University of Iowa
Iowa City, IA, United States
Presenting Author(s)
Background: Extremely premature infants can develop capillary leak syndrome (CLS) in response to a significant inflammatory event, such as sepsis, spontaneous intestinal perforation, or necrotizing enterocolitis. CLS contributes to an increased risk of morbidity and mortality for these infants. Clinically, we have found that these infants develop a prolonged lymphopenia that persists after the resolution of CLS. Little is known about the cytokine profile of CLS in premature infants.
Objective: To characterize longitudinal serum cytokine and T lymphocyte populations in extremely preterm infants with CLS.
Design/Methods: Two infants who developed CLS in 2021 were included. Clinical information was obtained via review of the electronic medical record. Residual clinical blood samples were collected longitudinally. Serum levels of IL-1B, sIL2Ra, IL-6, IL-8, IL-10, IP-10, MCP-1, MIP-1a, and TNFa were quantified by multiplex protein assay. Isolated buffy coats were incubated with antibodies targeting CD3, CD4, CD8, CD25, and Foxp3 to assess for T lymphocyte subsets by flow cytometry.
Results: At the time of the inciting inflammatory event, both infants had significant elevation in pro-inflammatory cytokines and chemokines, including IL-1B, sIL2Ra, IL-6, IL-8, MCP-1 and TNFa. These pro-inflammatory proteins returned to baseline levels within 4 days, but sIL2Ra remained elevated above baseline concentrations for up to 8 weeks. Serum sIL2Ra levels correlated inversely with total lymphocyte count (Fig 1). Flow cytometry evaluation of the lymphocytes demonstrated a two- to three-fold increase in regulatory T cells (Tregs, CD4+CD25+Foxp3+) and a decline in CD4+ T cells after the onset of CLS, which persisted for the duration of the lymphopenic period (Fig 2). There was no effect on CD8+ T cells.Conclusion(s): Following a significant inflammatory event, extremely premature infants have prolonged elevation of sIL2Ra. This is likely due to the predominant Treg population, meant to limit further inflammation-related injury. This prolonged elevation leads to lymphopenia, which increases susceptibility to secondary infections. In vitro assays are currently being developed to further study the effect of sIL2Ra on neonatal T lymphocytes.
Figure 1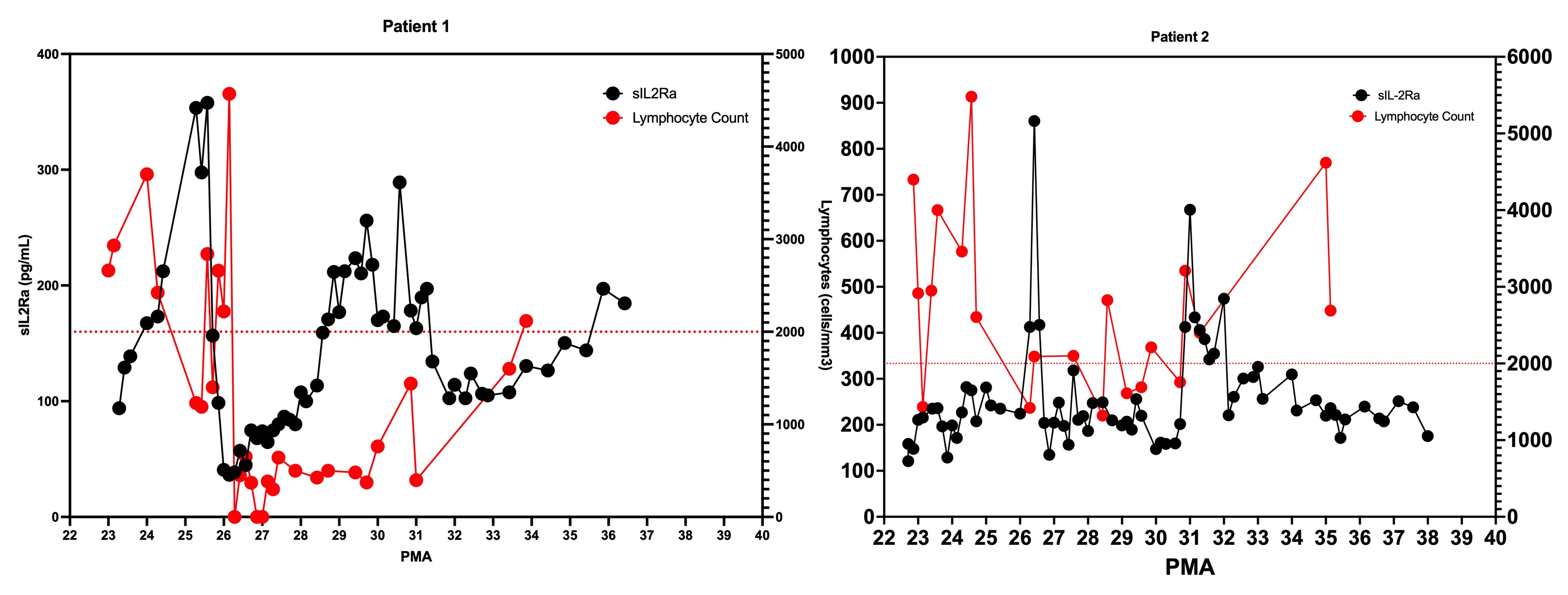 Serum sIL2Ra levels (left axis) as compared to peripheral lymphocyte count (right axis) for Patients 1 and 2. During periods of elevated sIL2Ra, there is an associated decrease in lymphocytes. Horizontal dashed line represents lymphopenia threshold.
Serum sIL2Ra levels (left axis) as compared to peripheral lymphocyte count (right axis) for Patients 1 and 2. During periods of elevated sIL2Ra, there is an associated decrease in lymphocytes. Horizontal dashed line represents lymphopenia threshold.
Figure 2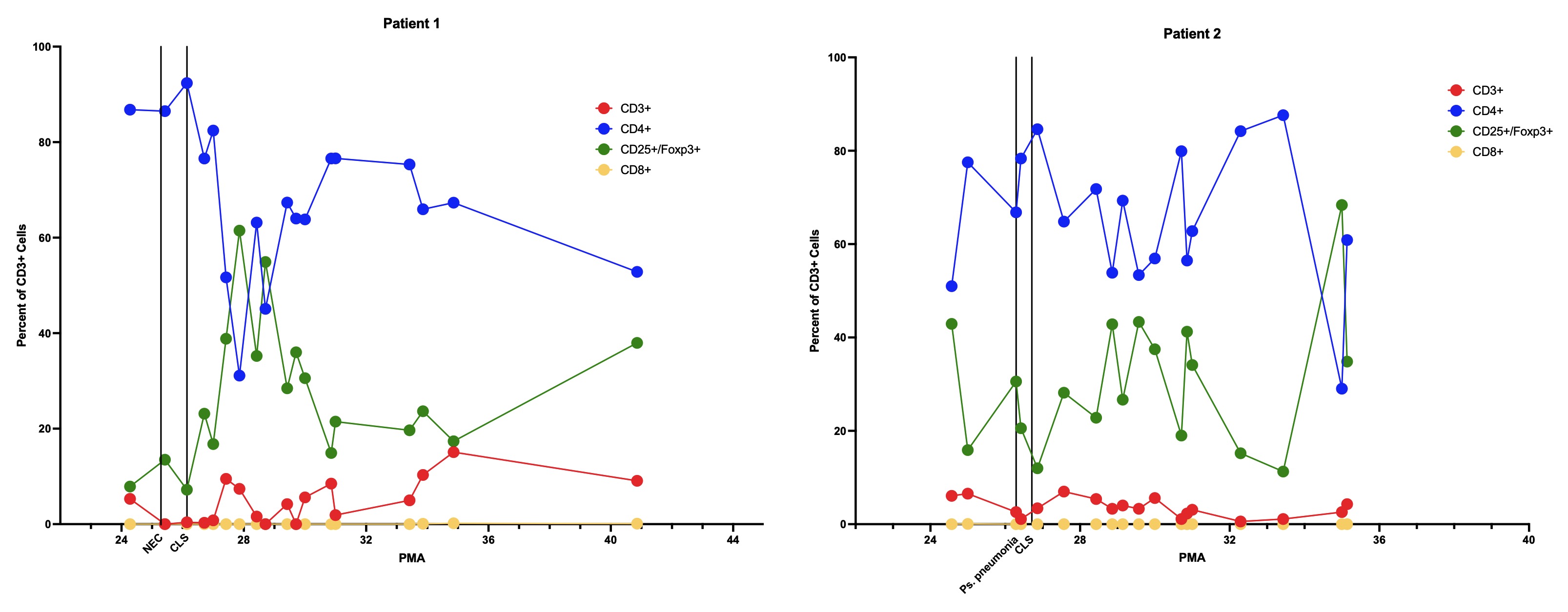 Subpopulations of T lymphocytes, expressed as percent of total CD3+ cells. Red: CD3+ only; blue: CD4+; green: CD25+/Foxp3+; yellow: CD8+. Significant illness and onset of CLS expressed by vertical lines.
Subpopulations of T lymphocytes, expressed as percent of total CD3+ cells. Red: CD3+ only; blue: CD4+; green: CD25+/Foxp3+; yellow: CD8+. Significant illness and onset of CLS expressed by vertical lines.
Objective: To characterize longitudinal serum cytokine and T lymphocyte populations in extremely preterm infants with CLS.
Design/Methods: Two infants who developed CLS in 2021 were included. Clinical information was obtained via review of the electronic medical record. Residual clinical blood samples were collected longitudinally. Serum levels of IL-1B, sIL2Ra, IL-6, IL-8, IL-10, IP-10, MCP-1, MIP-1a, and TNFa were quantified by multiplex protein assay. Isolated buffy coats were incubated with antibodies targeting CD3, CD4, CD8, CD25, and Foxp3 to assess for T lymphocyte subsets by flow cytometry.
Results: At the time of the inciting inflammatory event, both infants had significant elevation in pro-inflammatory cytokines and chemokines, including IL-1B, sIL2Ra, IL-6, IL-8, MCP-1 and TNFa. These pro-inflammatory proteins returned to baseline levels within 4 days, but sIL2Ra remained elevated above baseline concentrations for up to 8 weeks. Serum sIL2Ra levels correlated inversely with total lymphocyte count (Fig 1). Flow cytometry evaluation of the lymphocytes demonstrated a two- to three-fold increase in regulatory T cells (Tregs, CD4+CD25+Foxp3+) and a decline in CD4+ T cells after the onset of CLS, which persisted for the duration of the lymphopenic period (Fig 2). There was no effect on CD8+ T cells.Conclusion(s): Following a significant inflammatory event, extremely premature infants have prolonged elevation of sIL2Ra. This is likely due to the predominant Treg population, meant to limit further inflammation-related injury. This prolonged elevation leads to lymphopenia, which increases susceptibility to secondary infections. In vitro assays are currently being developed to further study the effect of sIL2Ra on neonatal T lymphocytes.
Figure 1
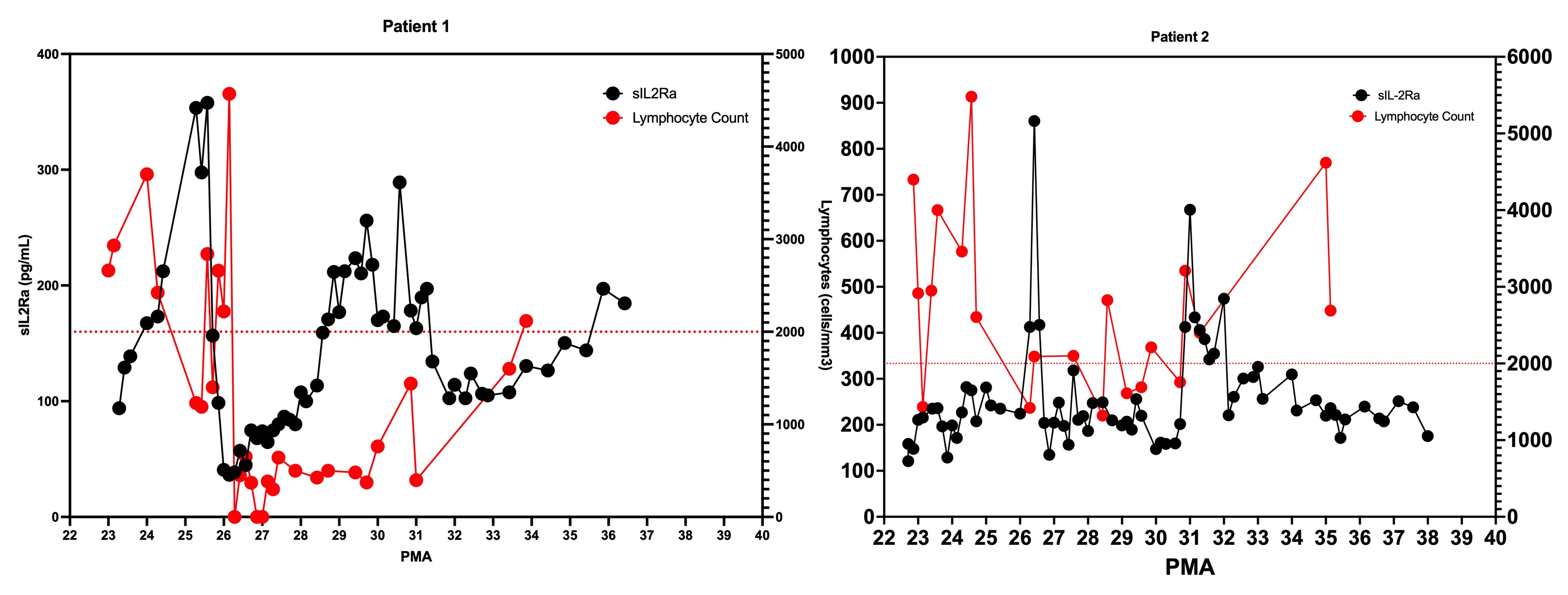 Serum sIL2Ra levels (left axis) as compared to peripheral lymphocyte count (right axis) for Patients 1 and 2. During periods of elevated sIL2Ra, there is an associated decrease in lymphocytes. Horizontal dashed line represents lymphopenia threshold.
Serum sIL2Ra levels (left axis) as compared to peripheral lymphocyte count (right axis) for Patients 1 and 2. During periods of elevated sIL2Ra, there is an associated decrease in lymphocytes. Horizontal dashed line represents lymphopenia threshold.Figure 2
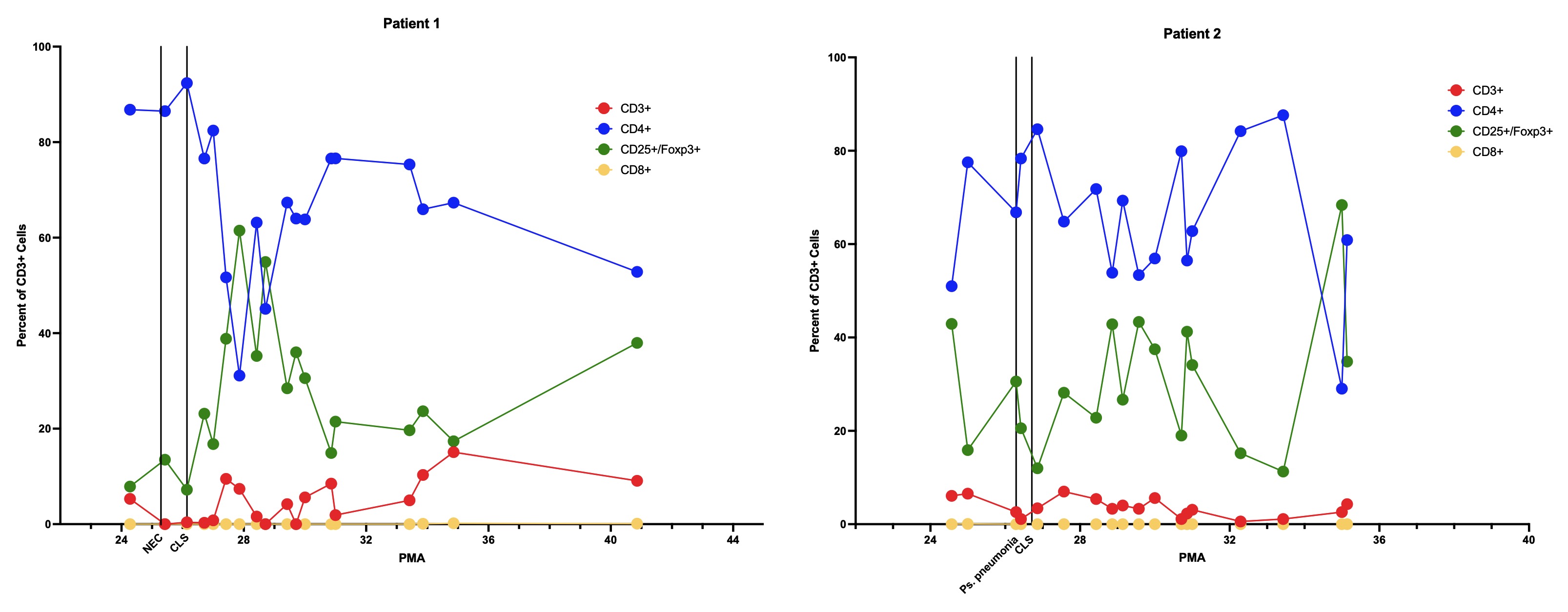 Subpopulations of T lymphocytes, expressed as percent of total CD3+ cells. Red: CD3+ only; blue: CD4+; green: CD25+/Foxp3+; yellow: CD8+. Significant illness and onset of CLS expressed by vertical lines.
Subpopulations of T lymphocytes, expressed as percent of total CD3+ cells. Red: CD3+ only; blue: CD4+; green: CD25+/Foxp3+; yellow: CD8+. Significant illness and onset of CLS expressed by vertical lines.