Infectious Diseases
Category: Abstract Submission
Infectious Diseases: COVID-19
295 - COVID-19 in Children: Worsening Outcomes During Delta Variant Wave
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 295
Publication Number: 295.215
Publication Number: 295.215
Christiana Smith-Anderson, University of Colorado, Aurora, CO, United States; Lori Silveira, University of Colorado School of Medicine, Aurora, CO, United States; Monika Jelic, University of Colorado School of Medicine, Aurora, CO, United States; Sean Lang, University of Colorado Anschutz, Aurora, CO, United States; Shane Curran-Hays, University of Colorado School of Medicine, Denver, CO, United States; Ye Ji Choi, University of Colorado, Aurora, CO, United States; JoEllen Fresia, University of Colorado School of Medicine, Parker, CO, United States; Brian M. Carter, University of Colorado School of Medicine, Denver, CO, United States; Shea Boyer, University of Colorado School of Medicine, Denver, CO, United States; Lisa Abuogi, University of Colorado, Denver, Aurora, CO, United States

Christiana Smith-Anderson, MD, MSc
Assistant Professor of Pediatrics
University of Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: Pediatric cases of COVID-19 surged in the summer/fall of 2021 coinciding with the SARS-CoV-2 Delta variant. It is unclear whether the Delta variant caused more severe illness among pediatric patients.
Objective: We leveraged the Children and COVID-19 in Colorado database to determine whether differences exist in demographics, underlying comorbidities, presenting symptoms, and outcomes among children requiring hospital admission due to the SARS-CoV-2 Delta variant vs. wild type virus.
Design/Methods: We performed a retrospective review of children < 21 years with symptomatic COVID-19 and detectable SARS-CoV-2 NAAT hospitalized at Children’s Hospital Colorado during pre-Delta (Mar-Nov 2020) and Delta (Jun-Sep 2021) periods. We compared variables using Fisher’s exact or Pearson’s chi square tests for categorical variables and Wilcoxon rank sum tests for continuous variables.
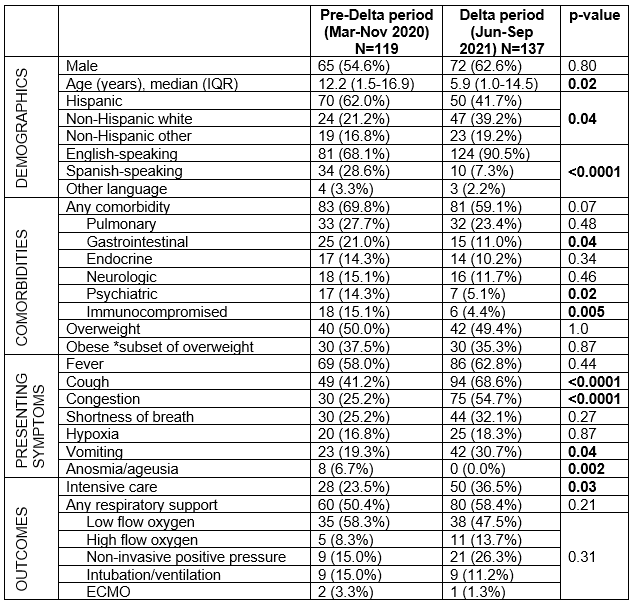
Results: There were 119 children hospitalized with symptomatic COVID-19 during the pre-Delta and 137 in the Delta period. There was a slight male predominance in both periods. Children hospitalized during the Delta period were younger, with median (interquartile range) age of 5.9 (1.0-14.5) vs. 12.2 (1.5-16.9) years, p=0.02; and were less likely to identify as Hispanic and Spanish-speaking, compared to the pre-Delta period (Table). There was a trend toward decreasing proportions of hospitalized children with underlying comorbidities in the Delta vs. pre-Delta period (59.1% vs. 69.8%; p=0.07). The most prevalent types of comorbidities were similar between periods; but the proportion of hospitalized immunocompromised patients was lower in the Delta vs. pre-Delta period (p=0.005). Half of all children were overweight/obese in both periods. Similar proportions of hospitalized children required respiratory support in both periods, but more children required intensive care in the Delta vs. pre-Delta periods (36.5% vs. 23.5%, p=0.03). Conclusion(s): Children hospitalized with the Delta variant of COVID-19 were younger, less likely to be Hispanic, and had fewer comorbidities than children hospitalized with wild type SARS-CoV-2. Children hospitalized with the Delta variant were more likely to require ICU admission compared to children hospitalized with wild type SARS-CoV-2, which may indicate increased severity of the Delta variant in the pediatric population. Close monitoring of pediatric outcomes is needed as new SARS-CoV-2 variants emerge.
Table. Comparison of characteristics of hospitalized children with symptomatic SARS-COV-2 during the Delta vs. pre-Delta periods.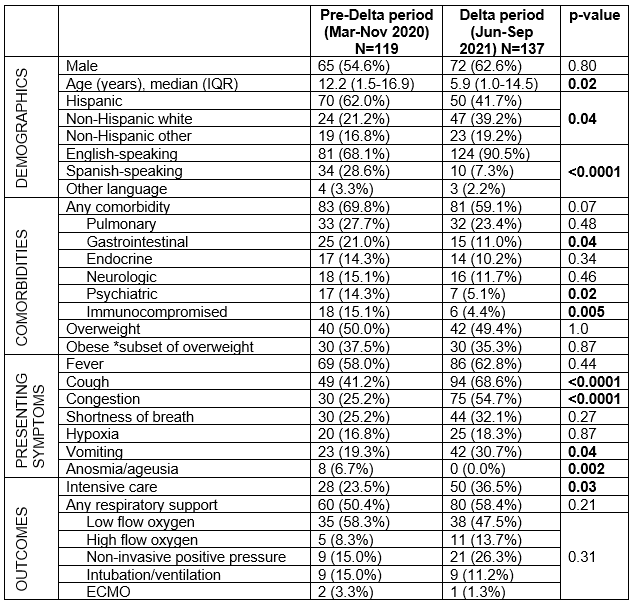
Objective: We leveraged the Children and COVID-19 in Colorado database to determine whether differences exist in demographics, underlying comorbidities, presenting symptoms, and outcomes among children requiring hospital admission due to the SARS-CoV-2 Delta variant vs. wild type virus.
Design/Methods: We performed a retrospective review of children < 21 years with symptomatic COVID-19 and detectable SARS-CoV-2 NAAT hospitalized at Children’s Hospital Colorado during pre-Delta (Mar-Nov 2020) and Delta (Jun-Sep 2021) periods. We compared variables using Fisher’s exact or Pearson’s chi square tests for categorical variables and Wilcoxon rank sum tests for continuous variables.
Results: There were 119 children hospitalized with symptomatic COVID-19 during the pre-Delta and 137 in the Delta period. There was a slight male predominance in both periods. Children hospitalized during the Delta period were younger, with median (interquartile range) age of 5.9 (1.0-14.5) vs. 12.2 (1.5-16.9) years, p=0.02; and were less likely to identify as Hispanic and Spanish-speaking, compared to the pre-Delta period (Table). There was a trend toward decreasing proportions of hospitalized children with underlying comorbidities in the Delta vs. pre-Delta period (59.1% vs. 69.8%; p=0.07). The most prevalent types of comorbidities were similar between periods; but the proportion of hospitalized immunocompromised patients was lower in the Delta vs. pre-Delta period (p=0.005). Half of all children were overweight/obese in both periods. Similar proportions of hospitalized children required respiratory support in both periods, but more children required intensive care in the Delta vs. pre-Delta periods (36.5% vs. 23.5%, p=0.03). Conclusion(s): Children hospitalized with the Delta variant of COVID-19 were younger, less likely to be Hispanic, and had fewer comorbidities than children hospitalized with wild type SARS-CoV-2. Children hospitalized with the Delta variant were more likely to require ICU admission compared to children hospitalized with wild type SARS-CoV-2, which may indicate increased severity of the Delta variant in the pediatric population. Close monitoring of pediatric outcomes is needed as new SARS-CoV-2 variants emerge.
Table. Comparison of characteristics of hospitalized children with symptomatic SARS-COV-2 during the Delta vs. pre-Delta periods.