General Pediatrics: All Areas
Category: Abstract Submission
General Pediatrics II
605 - Drivers of decision-making about infant sleep practices in mothers with opioid use disorder
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 605
Publication Number: 605.209
Publication Number: 605.209
Tierney Morrison, Boston Children's Hospital, Boston, MA, United States; Katherine Standish, Boston University School of Medicine, Boston, MA, United States; Amita Wanar, Boston University School of Medicine, Northampton, MA, United States; Cara B. Safon, Boston University School of Public Health, Boston, MA, United States; Davida Schiff, Massachusetts General Hospital, Boston, MA, United States; Elisha Wachman, Boston Medical Center, Boston, MA, United States; Mari-Lynn Drainoni, Boston University School of Medicine, Boston, MA, United States; Eve R. Colson, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Lisa Crowell, Boston University School of Medicine, Belmont, MA, United States; Margaret Parker, Boston Medical Center, Boston, MA, United States

Tierney Morrison, MD
Clinical Fellow
Boston Children's Hospital
Wayland, Massachusetts, United States
Presenting Author(s)
Background: Infants born to mothers with opioid use disorder (OUD) have high risk of sudden unexplained infant death (SUID). Safe sleep practices (supine sleep and room sharing but not bedsharing) reduce risk of SUID. Factors that drive decision making in infant sleep practices among mothers with OUD are unclear.
Objective: To understand factors that drive decision-making regarding infant sleep practices among mothers with OUD using the Theory of Planned Behavior (TPB) framework.
Design/Methods: We conducted a qualitative study via in-depth, semi-structured interviews with mothers with OUD with term infants 2-6 months of age. We asked participants open ended questions about facilitators and barriers to following safe sleep recommendations using the domains of the TPB framework to guide the questions (attitudes, perceived control and self-efficacy, social norms). We iteratively created and refined codes and generated themes. We concluded data collection upon achieving thematic saturation.
Results: Twenty mothers caring for their infants were interviewed between August 2020 and October 2021. Regarding attitudes, mothers chose sleeping positions and locations that were perceived to be safer and more comfortable. With respect to perceived control, mothers described that they chose sleeping practices that minimized the negative impact of withdrawal symptoms and maximized safety. Mothers reported that external factors such as rules in residential treatment facilities regarding infant sleep impacted their decisions. In terms of self-efficacy, mothers considered their own exhaustion, needs and well-being in their decisions for infant sleep practices. Regarding social norms, hospital sleep modeling practices and messaging by providers, friends and family influenced their decisions about safe sleep (Tables 1-3).Conclusion(s): Mothers with OUD reported facilitators and barriers to following safe sleep recommendations, some of which were likely unique to their situation including caring for an infant experiencing ongoing withdrawal symptoms, mothers’ own treatment for OUD, and social support systems. Further investigation regarding the prevalence of these factors is needed to inform tailored interventions to promote safe sleep practices in this high-risk population.
Table 1: Examples of attitudes about infant sleep practices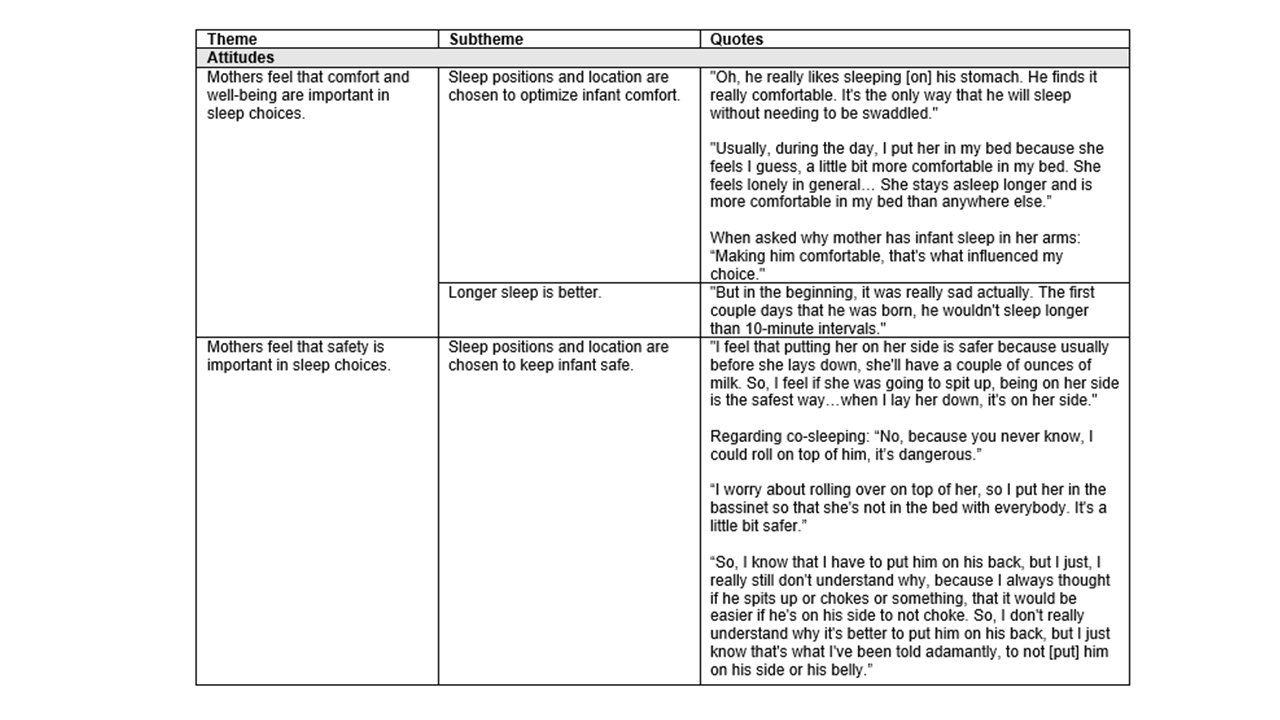
Table 2: Examples of perceived control over infant sleep practices.png)
Objective: To understand factors that drive decision-making regarding infant sleep practices among mothers with OUD using the Theory of Planned Behavior (TPB) framework.
Design/Methods: We conducted a qualitative study via in-depth, semi-structured interviews with mothers with OUD with term infants 2-6 months of age. We asked participants open ended questions about facilitators and barriers to following safe sleep recommendations using the domains of the TPB framework to guide the questions (attitudes, perceived control and self-efficacy, social norms). We iteratively created and refined codes and generated themes. We concluded data collection upon achieving thematic saturation.
Results: Twenty mothers caring for their infants were interviewed between August 2020 and October 2021. Regarding attitudes, mothers chose sleeping positions and locations that were perceived to be safer and more comfortable. With respect to perceived control, mothers described that they chose sleeping practices that minimized the negative impact of withdrawal symptoms and maximized safety. Mothers reported that external factors such as rules in residential treatment facilities regarding infant sleep impacted their decisions. In terms of self-efficacy, mothers considered their own exhaustion, needs and well-being in their decisions for infant sleep practices. Regarding social norms, hospital sleep modeling practices and messaging by providers, friends and family influenced their decisions about safe sleep (Tables 1-3).Conclusion(s): Mothers with OUD reported facilitators and barriers to following safe sleep recommendations, some of which were likely unique to their situation including caring for an infant experiencing ongoing withdrawal symptoms, mothers’ own treatment for OUD, and social support systems. Further investigation regarding the prevalence of these factors is needed to inform tailored interventions to promote safe sleep practices in this high-risk population.
Table 1: Examples of attitudes about infant sleep practices
Table 2: Examples of perceived control over infant sleep practices
.png)
