Neonatal Cardiac Physiology/Pathophysiology/Pulmonary Hypertension
Category: Abstract Submission
Neonatal Cardiac Physiology/Pathophysiology/ Pulmonary Hypertension I
194 - Effects of Maternal Preeclampsia on Hemodynamics of Very Low-Birth-Weight Infants
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 194
Publication Number: 194.219
Publication Number: 194.219
GoleNaz A. Kohbodi, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Bijan Siassi, LAC+USC Medical Center, Los Angeles, CA, United States; Rowena G. Cayabyab, LAC+USC MEDICAL CENTER, LOS ANGELES, CA, United States; Mahmood Ebrahimi, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Merujan Uzunyan, LAC+USC, LOS ANGELES, CA, United States; Lorayne Barton, LAC+USC Med Ctr, Los Angeles, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States
- GK
GoleNaz A. Kohbodi, MD
Fellow
UC Irvine
Irvine, California, United States
Presenting Author(s)
Background: Neonatal complications related to preeclampsia (PE) include growth restriction, prematurity, and morbidities related to neurodevelopment and cardiovascular system in later life. It’s been shown in studies that exposure to PE can lead to cardiac remodeling in the fetus and term infants, however, this has not been studied in very low birth weight (VLBW) infants.
Objective: The purpose of the study was to determine whether exposure to maternal PE is associated with hemodynamic changes and cardiac dysfunction in VLBW infants.
Design/Methods: This is a retrospective study of VLBW infants admitted to the neonatal intensive care unit born to mothers with PE (cases) and had echocardiograms. Cases were matched by birth weight to infants not exposed to PE (controls). Study period was May 2015 to October 2021. Exclusion criteria were presence of congenital heart disease and no echocardiogram in the first 7 days of life. Demographics, blood pressure (BP) during the first 3 days of life, clinical outcomes, placental pathology and echocardiographic findings were collected. Data was analyzed with Wilcoxon Sign Rank test, McNemar’s Test, and linear regression where appropriate.
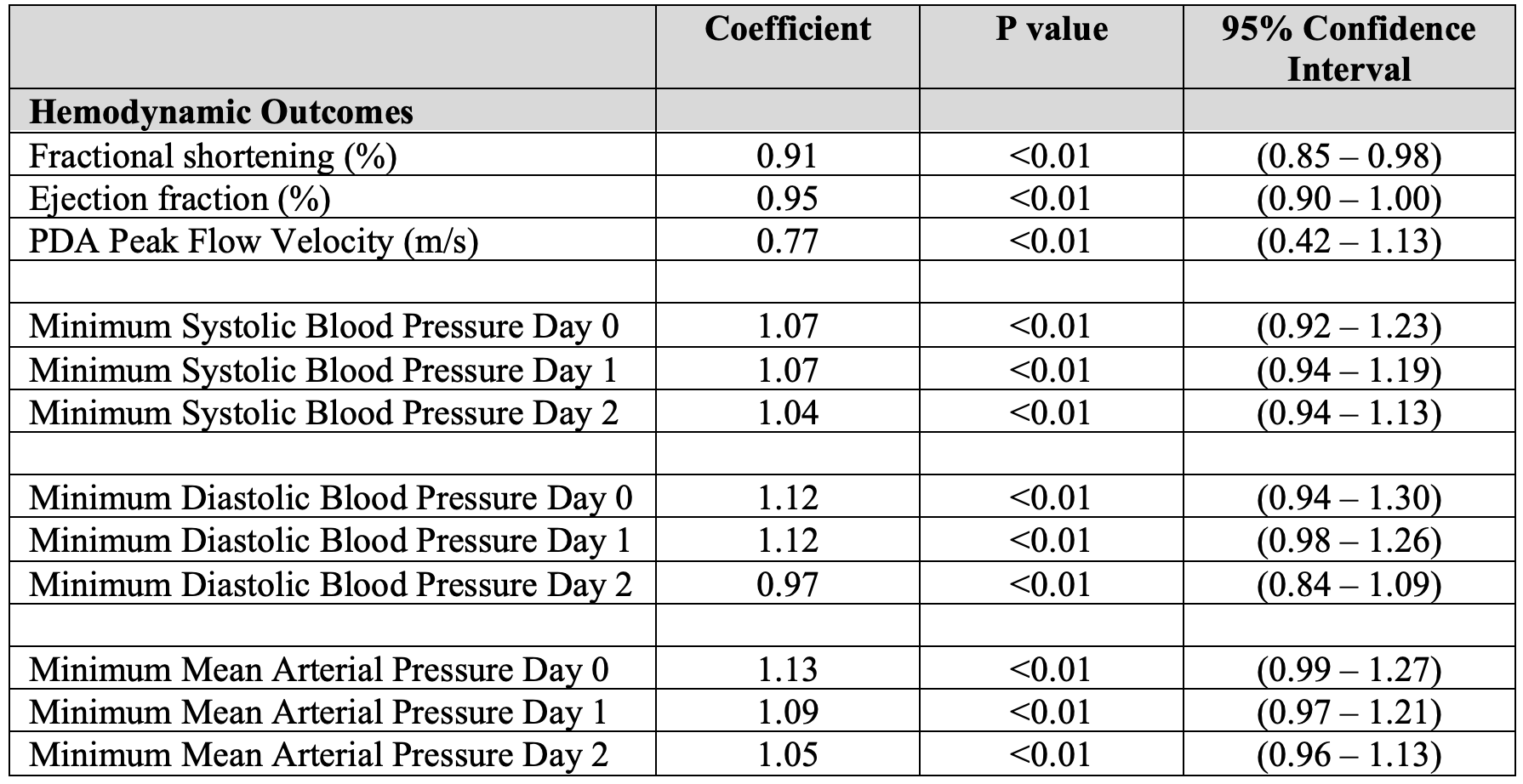
Results: There were 35 cases matched with controls. Infants exposed to PE were of higher gestational age (GA), growth restricted, with higher rate of placenta weighing less than 10th percentile for GA and lower rate of vasopressor resistant hypotension in the first 7 days of life. Radiologic diagnosis of cardiomegaly within the first 7-days of life was significantly higher in cases. (Table 1) During the first 2 days of life, the cases had significantly higher BP compared to controls. On echocardiography, cases had significantly lower ejection fraction (EF), fractional shortening (FS) and peak systolic flow velocity through patent ductus arteriosus (PDA) at 0.95, 0.91 and 0.77 of control values respectively. (Table 2) Lower peak flow velocity through PDA indicates higher pulmonary arterial pressure. Conclusion(s): Our data showed that VLBW infants born to preeclamptic mothers are growth restricted, have higher systemic vascular resistance as evidenced by elevated BP after birth and higher pulmonary vascular resistance suggested by lower peak flow velocity through PDA. Cardiomegaly, lower EF and FS are also likely due to increased systemic vascular resistance. These findings can probably be explained as a result of exposure to increased resistance to flow through the placenta. This information can be helpful for management of infants with hemodynamic compromise born to mothers with PE.
Table 1: Demographics, Clinical Outcomes, Radiologic and Placental Findings.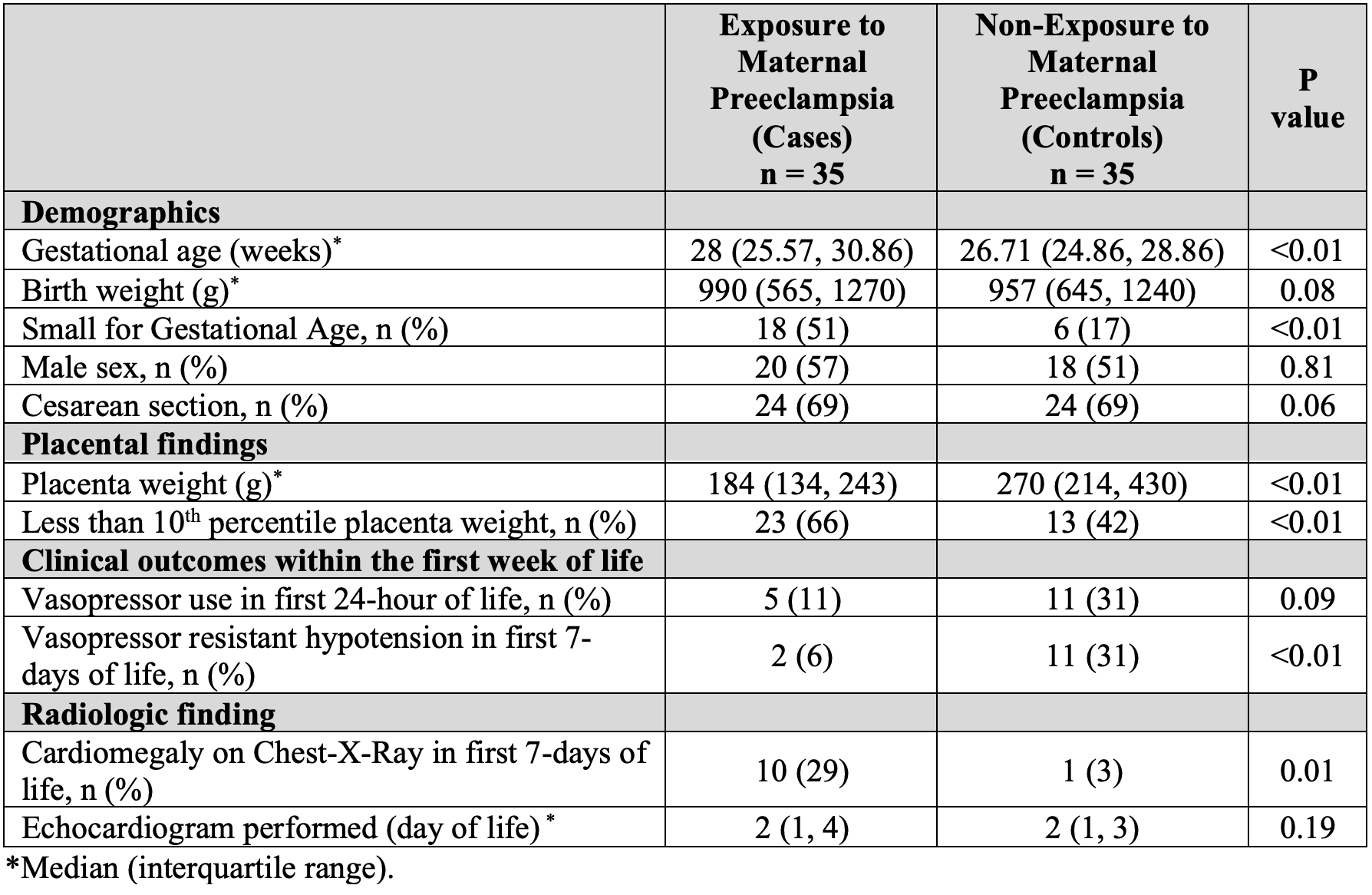
Table 2: Linear Regression of Echocardiographic and Blood Pressure Measurements in Cases Compared to Controls.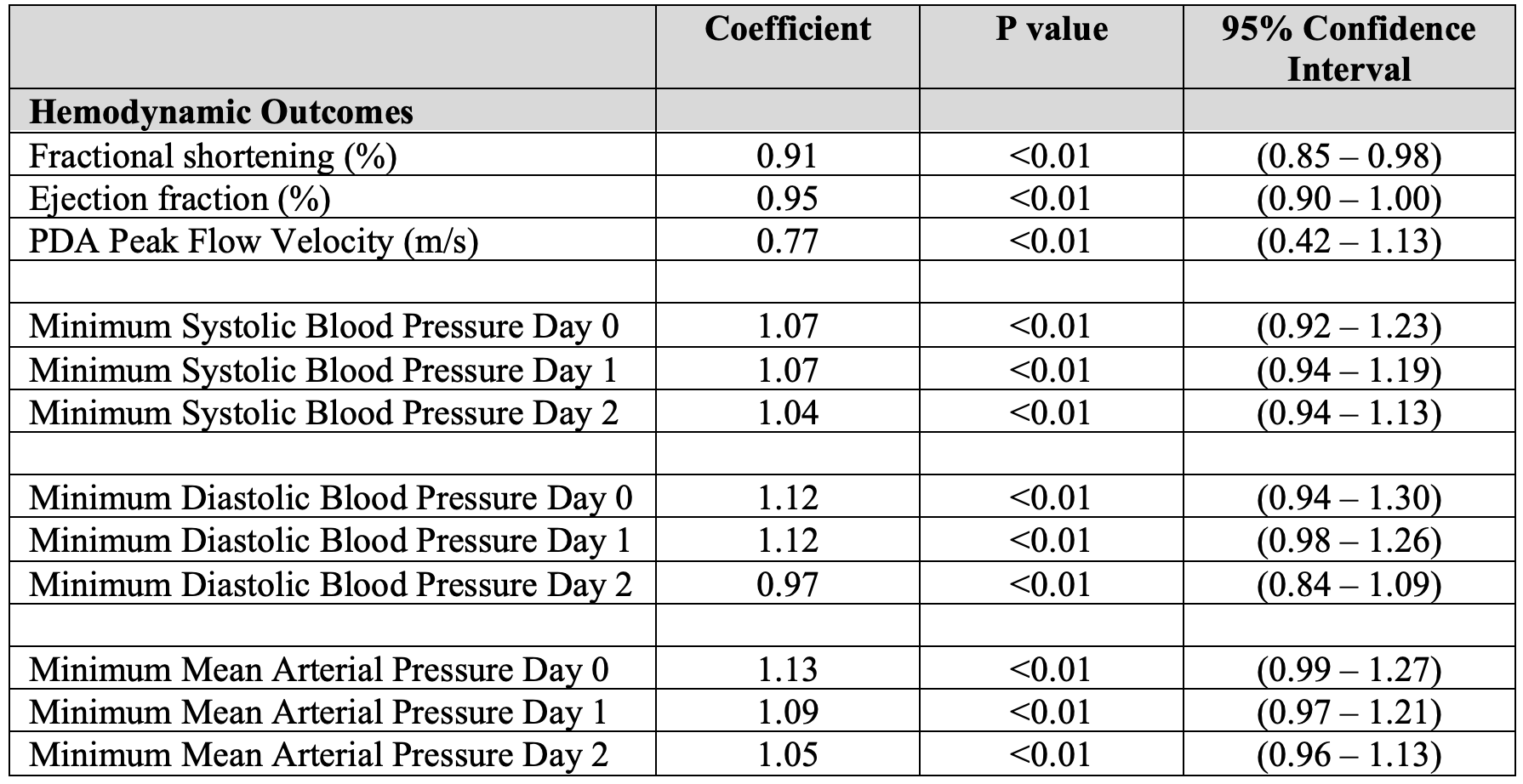
Objective: The purpose of the study was to determine whether exposure to maternal PE is associated with hemodynamic changes and cardiac dysfunction in VLBW infants.
Design/Methods: This is a retrospective study of VLBW infants admitted to the neonatal intensive care unit born to mothers with PE (cases) and had echocardiograms. Cases were matched by birth weight to infants not exposed to PE (controls). Study period was May 2015 to October 2021. Exclusion criteria were presence of congenital heart disease and no echocardiogram in the first 7 days of life. Demographics, blood pressure (BP) during the first 3 days of life, clinical outcomes, placental pathology and echocardiographic findings were collected. Data was analyzed with Wilcoxon Sign Rank test, McNemar’s Test, and linear regression where appropriate.
Results: There were 35 cases matched with controls. Infants exposed to PE were of higher gestational age (GA), growth restricted, with higher rate of placenta weighing less than 10th percentile for GA and lower rate of vasopressor resistant hypotension in the first 7 days of life. Radiologic diagnosis of cardiomegaly within the first 7-days of life was significantly higher in cases. (Table 1) During the first 2 days of life, the cases had significantly higher BP compared to controls. On echocardiography, cases had significantly lower ejection fraction (EF), fractional shortening (FS) and peak systolic flow velocity through patent ductus arteriosus (PDA) at 0.95, 0.91 and 0.77 of control values respectively. (Table 2) Lower peak flow velocity through PDA indicates higher pulmonary arterial pressure. Conclusion(s): Our data showed that VLBW infants born to preeclamptic mothers are growth restricted, have higher systemic vascular resistance as evidenced by elevated BP after birth and higher pulmonary vascular resistance suggested by lower peak flow velocity through PDA. Cardiomegaly, lower EF and FS are also likely due to increased systemic vascular resistance. These findings can probably be explained as a result of exposure to increased resistance to flow through the placenta. This information can be helpful for management of infants with hemodynamic compromise born to mothers with PE.
Table 1: Demographics, Clinical Outcomes, Radiologic and Placental Findings.
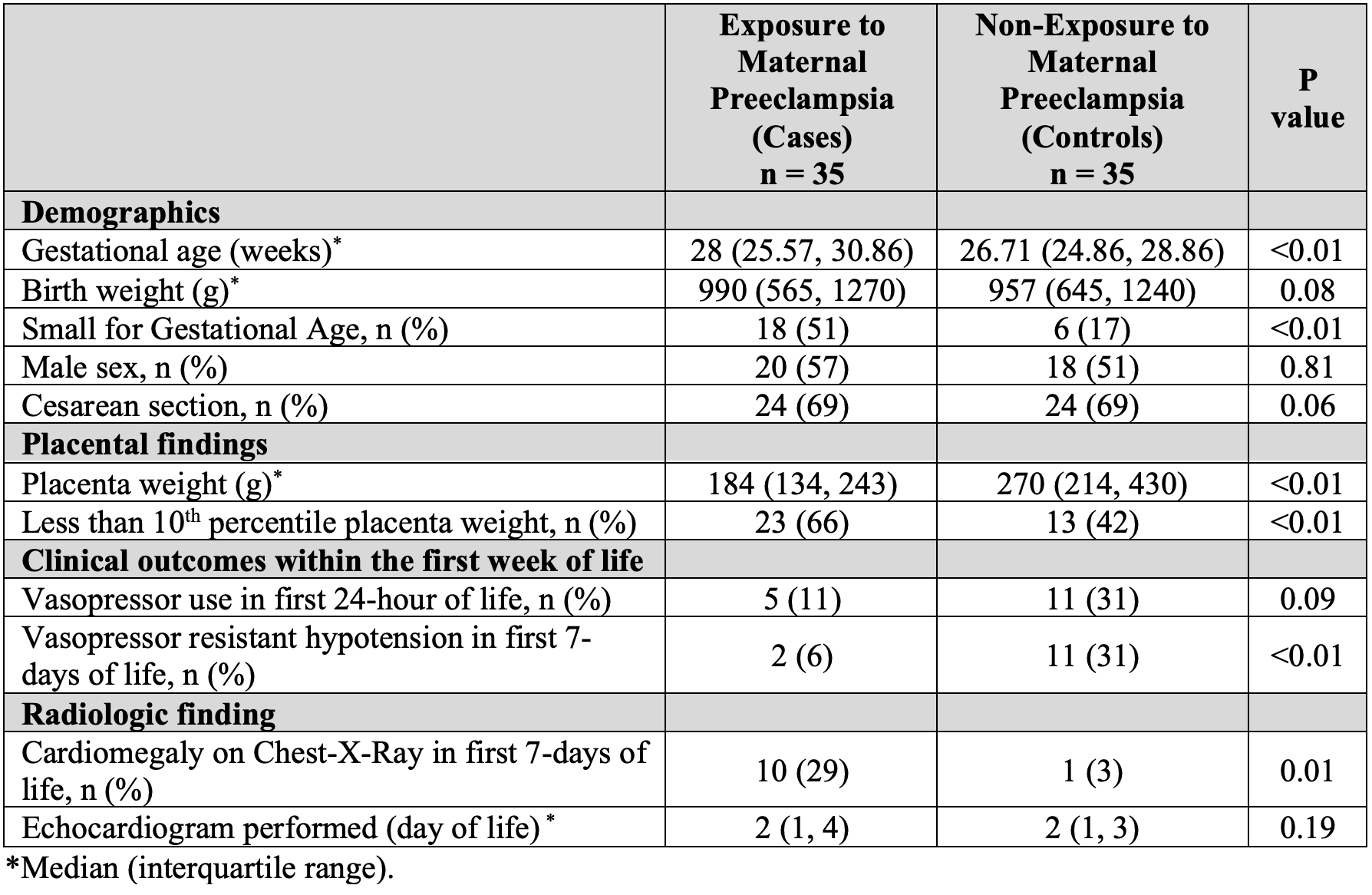
Table 2: Linear Regression of Echocardiographic and Blood Pressure Measurements in Cases Compared to Controls.