Back
Critical Care
Category: Abstract Submission
Critical Care II
20 - Hemorrhagic Complications and Outcomes of Children with Acute Promyelocytic Leukemia at Initial Presentation: A Multicenter Cohort Study
Saturday, April 23, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 20
Publication Number: 20.201
Publication Number: 20.201
Ariella Barhen, Nicklaus Children's Hospital, Miami, FL, United States; Prithvi Raj Sendi Keshavamurthy, Nicklaus Children’s Hospital, Miami, FL, United States; Paul A. Martinez, Nicklaus Children’s Hospital, Miami, FL, United States; Guillermo De Angulo, Herbert Wertheim School of Medicine, Miami, FL, United States; Balagangadhar R. Totapally, Nicklaus Children’s Hospital, Miami, FL, United States

Prithvi Raj Sendi Keshavamurthy, MD
Clinical Assistant Professor of Pediatrics
Nicklaus Children’s Hospital
Miami, Florida, United States
Presenting Author(s)
Background: Acute promyelocytic leukemia (APL) is an uncommon subtype of acute myeloid leukemia that is associated with hemorrhagic complications and early death.
Objective: Our primary objective was to describe the frequency of hemorrhagic complications and outcomes associated with APL during the initial admission using the Pediatric Health Information System (PHIS) database. Our secondary objectives were to describe the frequency of various interventions and blood product utilization.
Design/Methods: After an IRB approval, we performed a retrospective cross-sectional analysis using the PHIS database from January 2016 to June 2020. Data of children aged 1 month to 18 years of age, with a diagnosis of APL not in remission during their initial admission were extracted. Any child who received a hematopoietic stem cell transplant, methotrexate, or 6-mercaptopurine was excluded. Demographic characteristics, resource utilization, and outcomes were compared between two groups: those who developed hemorrhagic complications and those who did not. Descriptive statistics, Chi-square, Fisher’s exact, and Mann-Whitney tests were used to compare the groups.
Results: In our cohort of 173 patients with APL, the majority were White (56.6%), non-Hispanic (54.9%), and male (54.9%; Table 1). Hemorrhagic complications (intracranial, GI, or pulmonary) occurred in 32%. Children with hemorrhagic complications were more likely to have acute respiratory failure (OR 2.27; CI 1.01-5.11), coagulopathy or DIC (OR 2.07; CI 1.08-3.97), stroke (ischemic or hemorrhagic) (OR 38.7; CI 4.9-303.1), and cerebral edema (OR 19.3; CI 2.4-158.8; Table 2). Children with hemorrhagic complications experienced more ICU admissions, mechanical ventilation, and brain CT scans, and they also received transfusions, low molecular weight heparin, hydroxyurea, and rasburicase more frequently (p < 0.05; Table 3). The median length of stay and mortality rate were not different between the groups. The median length of stay of children who died was significantly lower (5 days; IQR 2-13; p=0.003). Among children who did not survive, death occurred within 10 days of admission in the majority (78%).Conclusion(s): Approximately one-third of children with APL have hemorrhagic complications at initial presentation. Children who experience hemorrhagic complications are more likely to be White, non-Hispanic males. They have a higher risk of associated respiratory and neurologic complications. The use of hydroxyurea and rasburicase more frequently in children with APL and hemorrhagic complications suggests that these children had higher initial white cell counts.
Table 1: Demographic characteristics of children with APL with and without hemorrhagic complications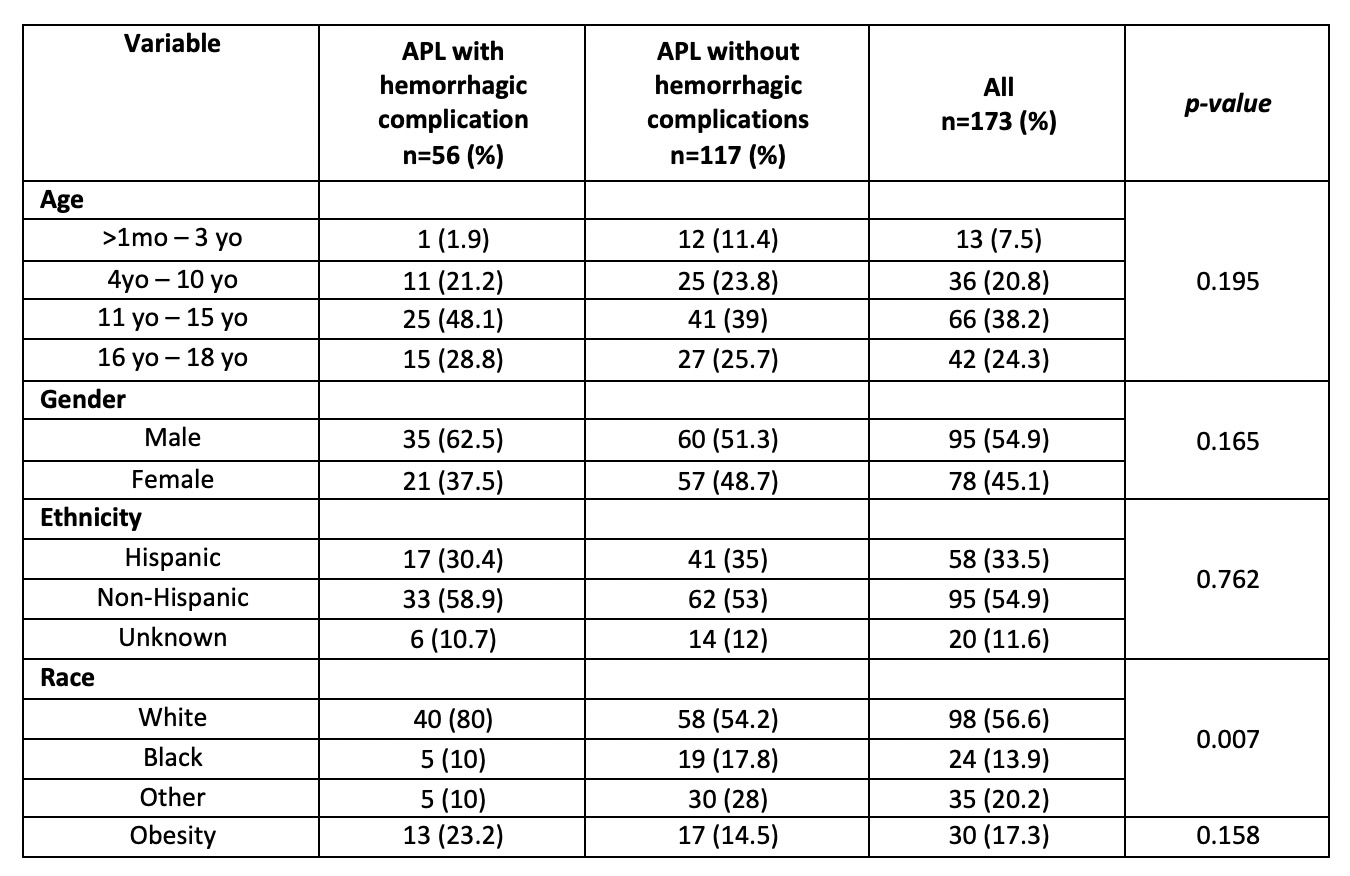
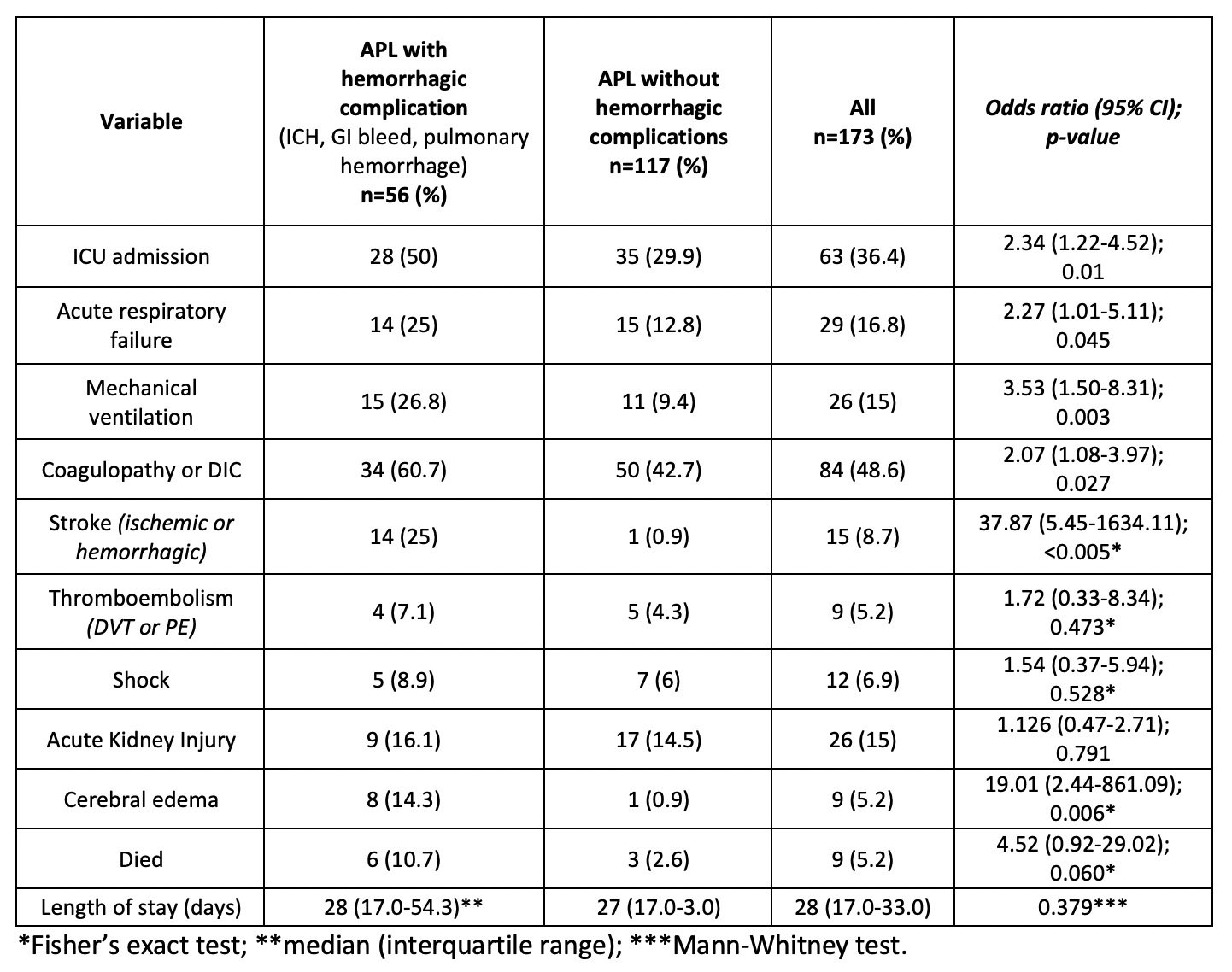
Table 2: Complications in children with APL with and without hemorrhagic complications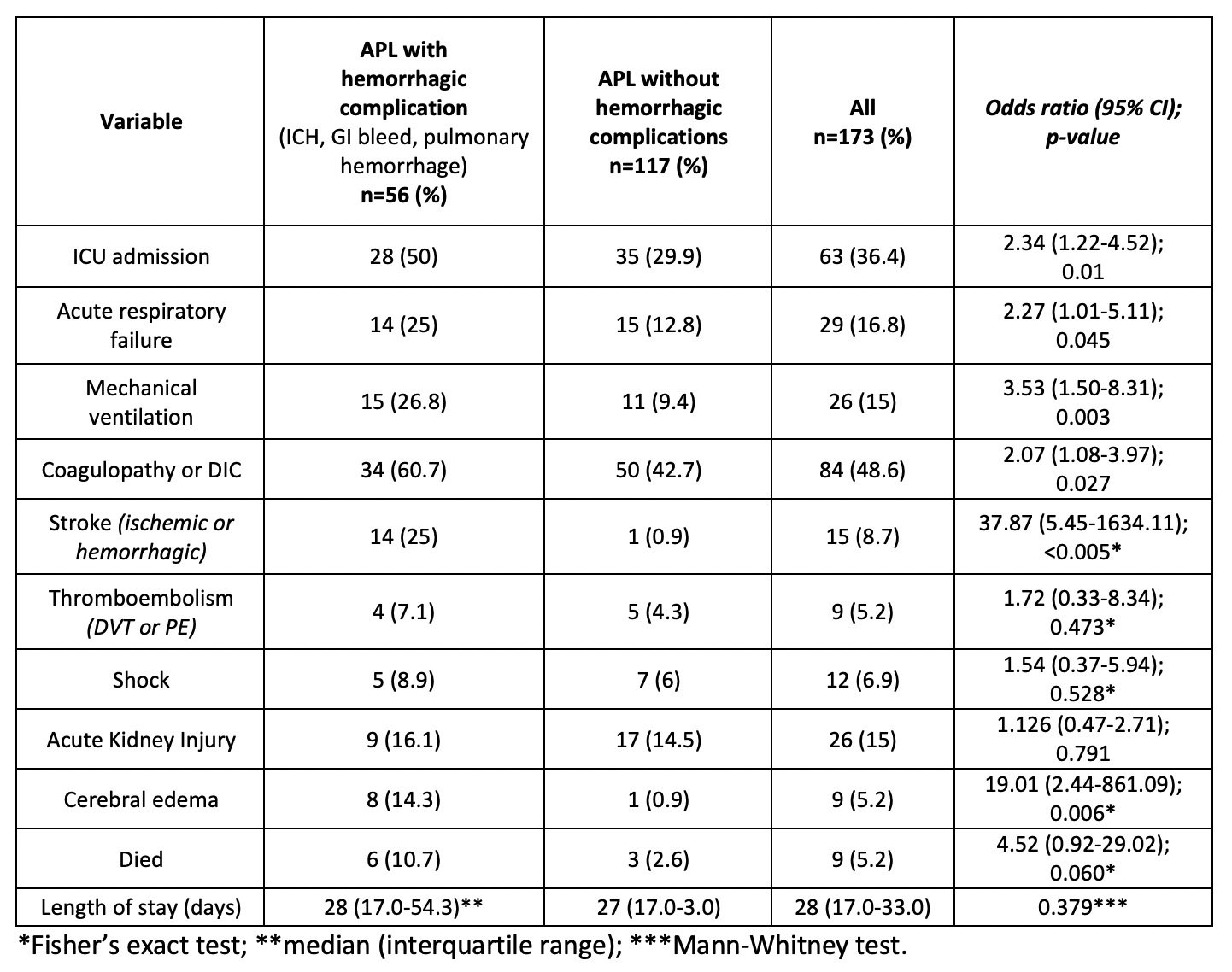
Objective: Our primary objective was to describe the frequency of hemorrhagic complications and outcomes associated with APL during the initial admission using the Pediatric Health Information System (PHIS) database. Our secondary objectives were to describe the frequency of various interventions and blood product utilization.
Design/Methods: After an IRB approval, we performed a retrospective cross-sectional analysis using the PHIS database from January 2016 to June 2020. Data of children aged 1 month to 18 years of age, with a diagnosis of APL not in remission during their initial admission were extracted. Any child who received a hematopoietic stem cell transplant, methotrexate, or 6-mercaptopurine was excluded. Demographic characteristics, resource utilization, and outcomes were compared between two groups: those who developed hemorrhagic complications and those who did not. Descriptive statistics, Chi-square, Fisher’s exact, and Mann-Whitney tests were used to compare the groups.
Results: In our cohort of 173 patients with APL, the majority were White (56.6%), non-Hispanic (54.9%), and male (54.9%; Table 1). Hemorrhagic complications (intracranial, GI, or pulmonary) occurred in 32%. Children with hemorrhagic complications were more likely to have acute respiratory failure (OR 2.27; CI 1.01-5.11), coagulopathy or DIC (OR 2.07; CI 1.08-3.97), stroke (ischemic or hemorrhagic) (OR 38.7; CI 4.9-303.1), and cerebral edema (OR 19.3; CI 2.4-158.8; Table 2). Children with hemorrhagic complications experienced more ICU admissions, mechanical ventilation, and brain CT scans, and they also received transfusions, low molecular weight heparin, hydroxyurea, and rasburicase more frequently (p < 0.05; Table 3). The median length of stay and mortality rate were not different between the groups. The median length of stay of children who died was significantly lower (5 days; IQR 2-13; p=0.003). Among children who did not survive, death occurred within 10 days of admission in the majority (78%).Conclusion(s): Approximately one-third of children with APL have hemorrhagic complications at initial presentation. Children who experience hemorrhagic complications are more likely to be White, non-Hispanic males. They have a higher risk of associated respiratory and neurologic complications. The use of hydroxyurea and rasburicase more frequently in children with APL and hemorrhagic complications suggests that these children had higher initial white cell counts.
Table 1: Demographic characteristics of children with APL with and without hemorrhagic complications
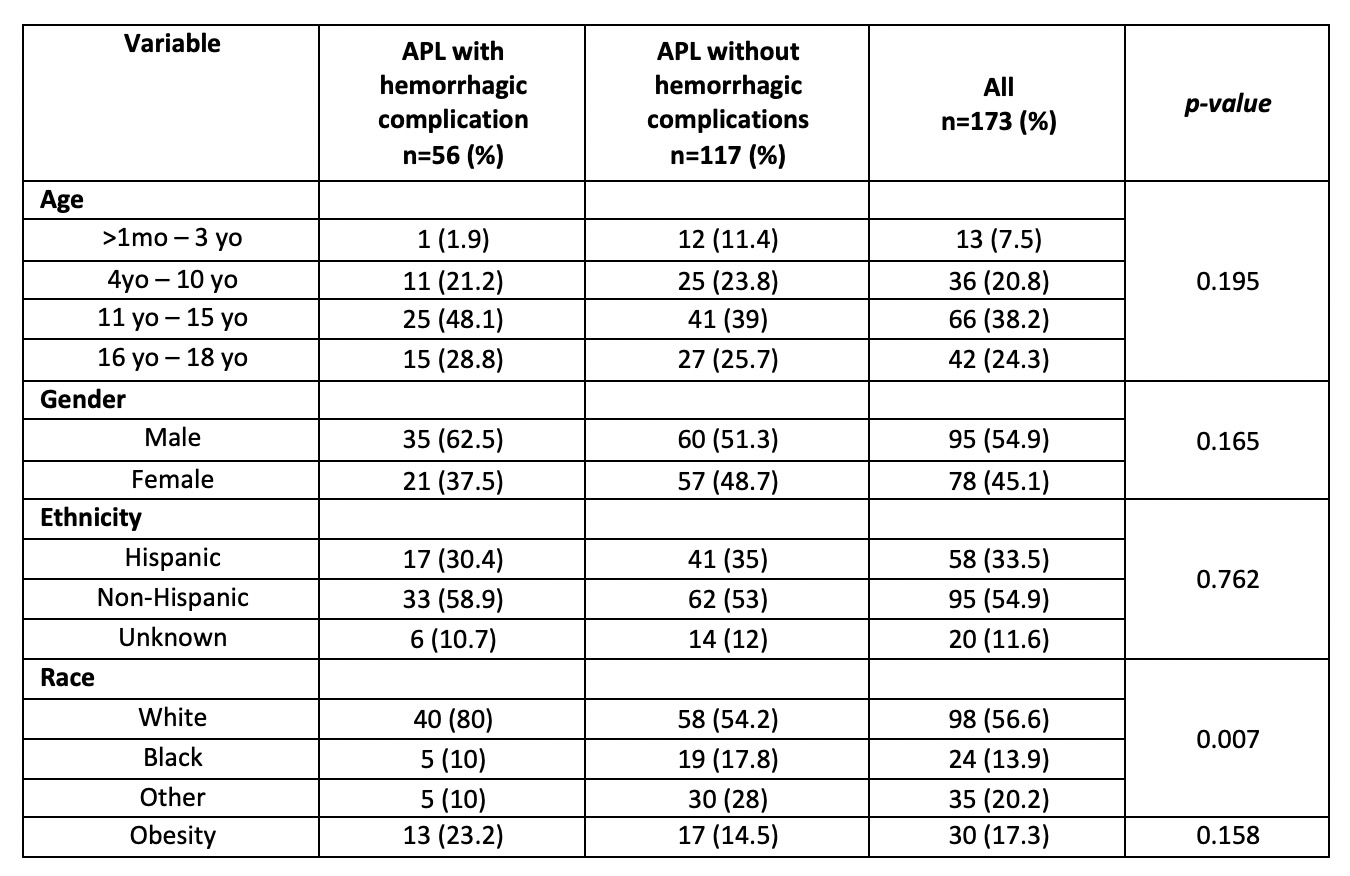
Table 2: Complications in children with APL with and without hemorrhagic complications