Emergency Medicine: Quality Improvement
Category: Abstract Submission
Emergency Medicine VI
354 - Integrating Cardiac Point-of-Care Ultrasound Into a Pediatric Emergency Sepsis Bundle
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 354
Publication Number: 354.205
Publication Number: 354.205
Jacob Hemberger, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Ethan S. Vorel, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Rachel Rempell, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Brandon Ku, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Fran Balamuth, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States

Jacob Hemberger, MD
Pediatric Emergency Medicine Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Cardiac point-of-care ultrasound (C-POCUS) is an emerging diagnostic tool in pediatric sepsis and is recommended by the recent Surviving Sepsis Guidelines to guide vasoactive medication choice in children with fluid refractory shock. The feasibility of integrating C-POCUS into early sepsis care in a pediatric ED is not known.
Objective:
To increase C-POCUS utilization in suspected sepsis cases in a large pediatric ED from a baseline of 3% to 50% within 12 months of project initiation.
Design/Methods:
We convened key stakeholders to define aims and identify key drivers. PDSA cycles included: 1) education on C-POCUS through division conferences and bedside training, 2) directed text alerts to C-POCUS trained providers working in the ED when a patient was being treated for sepsis, and 3) clinical decision support incorporating C-POCUS into the sepsis order set. 22 faculty and fellows credentialed in C-POCUS performed exams during the project period, and POCUS experts reviewed all ultrasound images for quality assurance. We used p-charts to track proportion of suspected sepsis cases utilizing C-POCUS and x-bar charts to track balancing metrics of time to fluid, antibiotic, and vasopressor administration. Finally, we explored univariate factors influencing rates of C-POCUS completion using chi-square testing.
Results: We identified 214 suspected sepsis cases during the project period. The proportion of patients with suspected sepsis who received a C-POCUS exam increased from 3% to 35%, with special cause variation (Figure 1). Balancing metrics were unchanged.
We reviewed 174 charts to identify factors impacting rates of C-POCUS completion (Table 1). We observed higher rates of C-POCUS completion with fellow presence in the ED, discharge diagnosis of multisystem inflammatory syndrome in children, and patients requiring hemodynamic support with at least two fluid boluses or a vasoactive medication. We saw a trend towards fewer C-POCUS exams performed for the sickest patients treated in the resuscitation bay or intubated, but this trend did not reach statistical significance.Conclusion(s):
We successfully increased C-POCUS utilization in patients with suspected sepsis from 3% to 35% in a large pediatric ED. Providers more often used C-POCUS for patients receiving hemodynamic support with high-volume fluid resuscitation or a vasoactive medication. Upcoming QI interventions include involving residents to obtain C-POCUS images and embedding text alerts into an EMR-based messaging platform. Next steps include determining the impact of C-POCUS on ED fluid and vasopressor decisions in pediatric sepsis.
CV (Jacob Hemberger)CV (Jake Hemberger).pdf
Table 1: Factors Influencing Rates of Cardiac POCUS Completion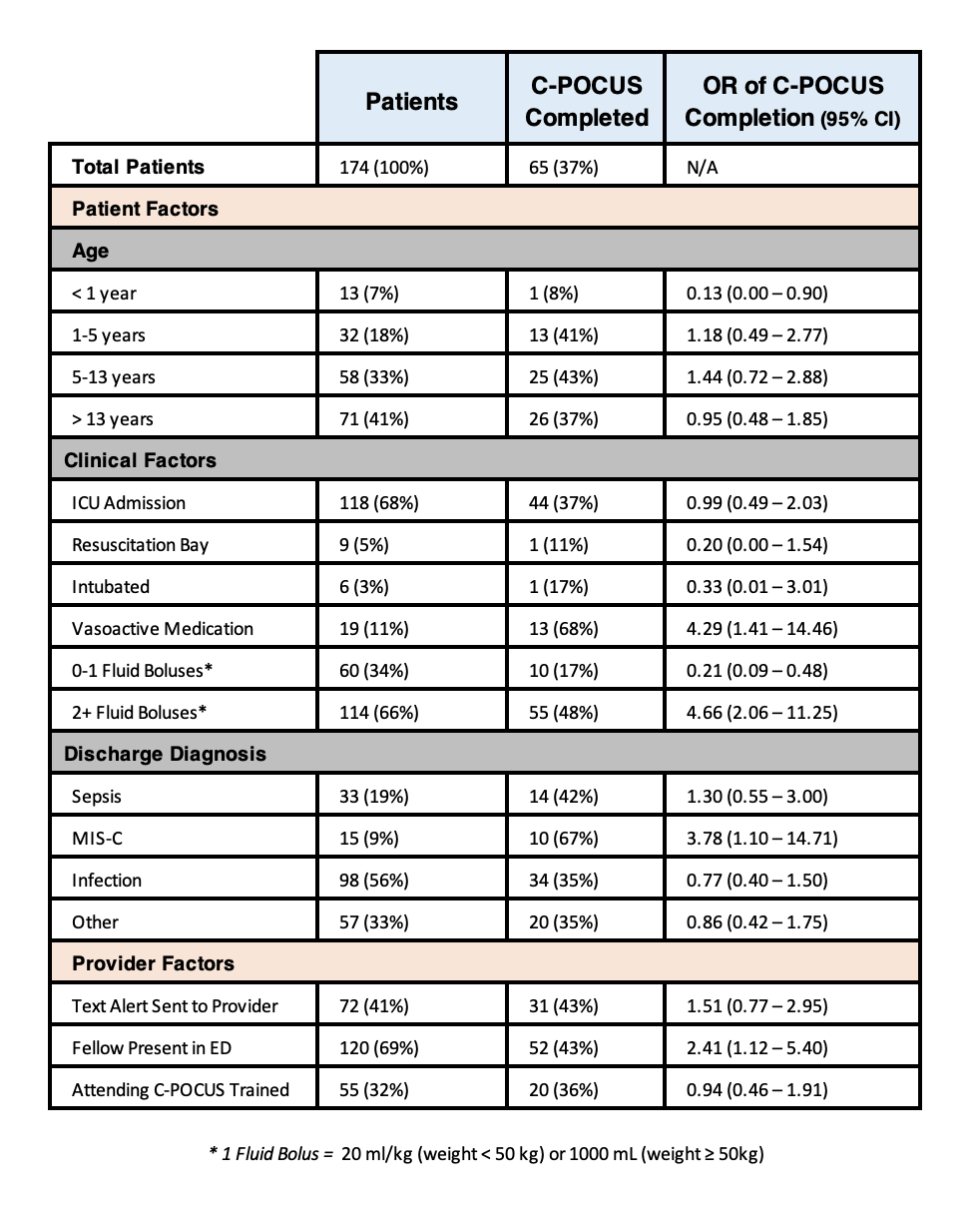 Patient and provider factors influencing likelihood of C-POCUS completion. MIS-C = multisystem inflammatory syndrome in children.
Patient and provider factors influencing likelihood of C-POCUS completion. MIS-C = multisystem inflammatory syndrome in children.
Cardiac point-of-care ultrasound (C-POCUS) is an emerging diagnostic tool in pediatric sepsis and is recommended by the recent Surviving Sepsis Guidelines to guide vasoactive medication choice in children with fluid refractory shock. The feasibility of integrating C-POCUS into early sepsis care in a pediatric ED is not known.
Objective:
To increase C-POCUS utilization in suspected sepsis cases in a large pediatric ED from a baseline of 3% to 50% within 12 months of project initiation.
Design/Methods:
We convened key stakeholders to define aims and identify key drivers. PDSA cycles included: 1) education on C-POCUS through division conferences and bedside training, 2) directed text alerts to C-POCUS trained providers working in the ED when a patient was being treated for sepsis, and 3) clinical decision support incorporating C-POCUS into the sepsis order set. 22 faculty and fellows credentialed in C-POCUS performed exams during the project period, and POCUS experts reviewed all ultrasound images for quality assurance. We used p-charts to track proportion of suspected sepsis cases utilizing C-POCUS and x-bar charts to track balancing metrics of time to fluid, antibiotic, and vasopressor administration. Finally, we explored univariate factors influencing rates of C-POCUS completion using chi-square testing.
Results: We identified 214 suspected sepsis cases during the project period. The proportion of patients with suspected sepsis who received a C-POCUS exam increased from 3% to 35%, with special cause variation (Figure 1). Balancing metrics were unchanged.
We reviewed 174 charts to identify factors impacting rates of C-POCUS completion (Table 1). We observed higher rates of C-POCUS completion with fellow presence in the ED, discharge diagnosis of multisystem inflammatory syndrome in children, and patients requiring hemodynamic support with at least two fluid boluses or a vasoactive medication. We saw a trend towards fewer C-POCUS exams performed for the sickest patients treated in the resuscitation bay or intubated, but this trend did not reach statistical significance.Conclusion(s):
We successfully increased C-POCUS utilization in patients with suspected sepsis from 3% to 35% in a large pediatric ED. Providers more often used C-POCUS for patients receiving hemodynamic support with high-volume fluid resuscitation or a vasoactive medication. Upcoming QI interventions include involving residents to obtain C-POCUS images and embedding text alerts into an EMR-based messaging platform. Next steps include determining the impact of C-POCUS on ED fluid and vasopressor decisions in pediatric sepsis.
CV (Jacob Hemberger)CV (Jake Hemberger).pdf
Table 1: Factors Influencing Rates of Cardiac POCUS Completion
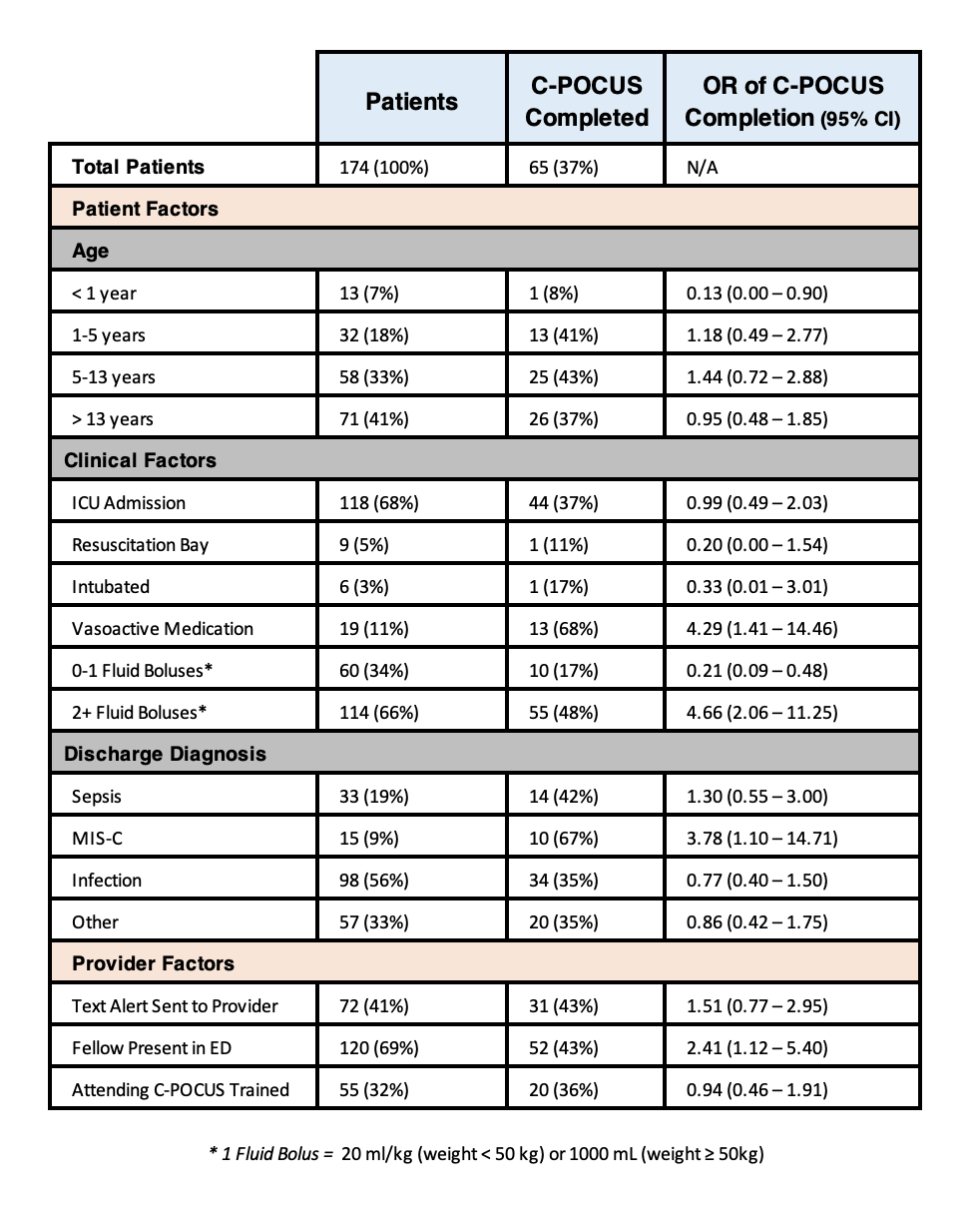 Patient and provider factors influencing likelihood of C-POCUS completion. MIS-C = multisystem inflammatory syndrome in children.
Patient and provider factors influencing likelihood of C-POCUS completion. MIS-C = multisystem inflammatory syndrome in children.