Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VII
371 - Outcomes of late-onset Group B Streptococcus bacteremia in infants attended at the pediatric emergency department and risk factors for severe infection
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 371
Publication Number: 371.206
Publication Number: 371.206
José Antonio Alonso Cadenas, Pediatric Emergency Department, Niño Jesús Children University Hospital, Madrid, Madrid, Spain; Francesco Giuseppe Ecclesia, Hospital Niño Jesús, Madrid, Madrid, Madrid, Spain; Borja Gomez, Pediatric Emergency Department. Cruces University Hospital, Barakaldo, Pais Vasco, Spain; Iker Gangoiti, Cruces University Hospital. Biocruces Bizkaia Health Research Institute. Bilbao, BILBAO, Pais Vasco, Spain; Susanna Hernández-Bou, Hospital Sant Joan de Déu Barcelona, ESPLUGUES DE LLOBREGAT, Catalonia, Spain; Mercedes de la Torre Espí, H. Infantil Universitario Niño Jesús, Madrid, Madrid, Spain
.jpg)
José Antonio Alonso Cadenas (he/him/his)
Pediatric Emergency Physician
Pediatric Emergency Department. Niño Jesús University Hospital
Madrid, Madrid, Spain
Presenting Author(s)
Background: Group B streptococcus (GBS) is the second most frequent pathogen involved in invasive bacterial infections in febrile infants younger than 3 months and the leading cause of sepsis and bacterial meningitis. GBS infection in these youngest infants is classified into early-onset disease (EOD: neonates 1-6 days old) and late-onset disease (LOD: infants 7-89 days old). Infection risk factors for EOD seem to be unrelated to LOD, but GBS exposures of infants with LOD occur in the home or in the community.
Objective: To describe clinical and epidemiological features and analytical characteristics of the infants attended in the Pediatric Emergency Departments (PEDs) and diagnosed with a LOD GBS bacteremia and to identify risk factors for severe infection and Pediatric Intensive Care Unit (PICU) admission.
Design/Methods: Sub-study of a multicentre cross-sectional prospective registry that included all the positive blood cultures (BCs) collected at 22 Spanish PEDs between 2011 and 2016. We analyzed the patients 7-89 days old with a positive BC by GBS. We defined severe infections as sepsis/septic shock or meningitis and bad outcome as presenting acute complications, sequelae or death. We considered GBS infection risk factors as maternal GBS colonization or delivery at < 37 weeks of gestation. We performed a multivariate analysis including clinical and analytical variables to identify independent risk factors for severe disease and PICU admission.
Results: Among 118 patients with LOD, 74 (62.7%) presented a severe infection: 66 sepsis/septic shock (11 with associated meningitis) and 8 meningitis without sepsis. Infants with severe infection had lower white blood cell and absolute neutrophil counts (table 1). However, presenting an altered Pediatric Assessment Triangle (PAT) upon arrival was the only independent risk factor for severe infection (table 2). Thirty-five patients (29.7%) were admitted to a PICU. Presenting leukopenia was an independent risk factor for PICU admission (table 3).
Six patients (5.1%) presented a bad outcome, including two deaths (1.7%). All of them presented an altered PAT and elevated procalcitonin values (>0.5 ng/ml) and were admitted to a PICU with sepsis/septic shock.Conclusion(s): Infants with a LOD by GBS frequently develop sepsis/septic shock and bacterial meningitis with not insignificant morbimortality. No risk factors for severe infection were identified except for the clinical appearance, whereas leukopenia was related to PICU admission.
Table 1. Clinical and epidemiological features and analytical characteristics of the infants with non-severe and severe late-onset Group B streptococcus infections.png) PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; IQR: interquartile range; ANC: absolute neutrophil count; n.s.: not significant.
PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; IQR: interquartile range; ANC: absolute neutrophil count; n.s.: not significant.
Table 2. Multivariate analysis to identify independent risk factors for severe infection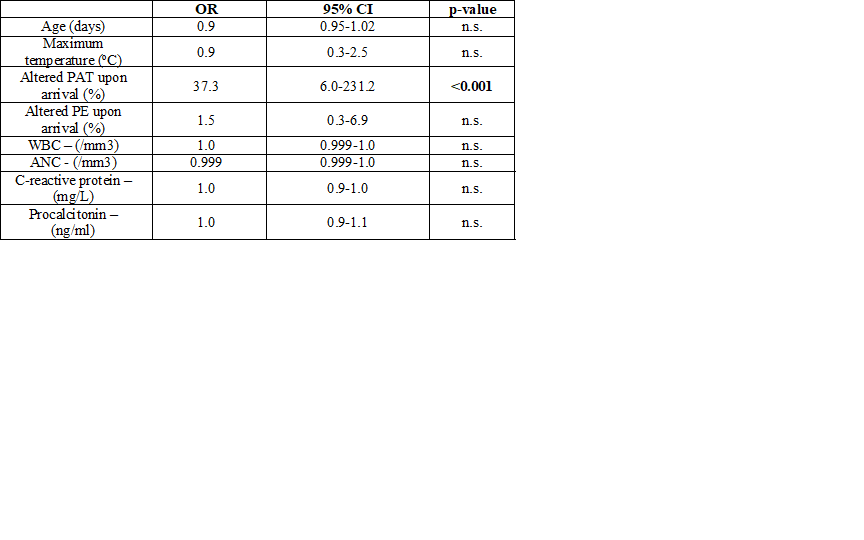 PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; ANC: absolute neutrophil count; OR: odds ratio; CI: confidence interval; n.s.: not significant.
PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; ANC: absolute neutrophil count; OR: odds ratio; CI: confidence interval; n.s.: not significant.
Objective: To describe clinical and epidemiological features and analytical characteristics of the infants attended in the Pediatric Emergency Departments (PEDs) and diagnosed with a LOD GBS bacteremia and to identify risk factors for severe infection and Pediatric Intensive Care Unit (PICU) admission.
Design/Methods: Sub-study of a multicentre cross-sectional prospective registry that included all the positive blood cultures (BCs) collected at 22 Spanish PEDs between 2011 and 2016. We analyzed the patients 7-89 days old with a positive BC by GBS. We defined severe infections as sepsis/septic shock or meningitis and bad outcome as presenting acute complications, sequelae or death. We considered GBS infection risk factors as maternal GBS colonization or delivery at < 37 weeks of gestation. We performed a multivariate analysis including clinical and analytical variables to identify independent risk factors for severe disease and PICU admission.
Results: Among 118 patients with LOD, 74 (62.7%) presented a severe infection: 66 sepsis/septic shock (11 with associated meningitis) and 8 meningitis without sepsis. Infants with severe infection had lower white blood cell and absolute neutrophil counts (table 1). However, presenting an altered Pediatric Assessment Triangle (PAT) upon arrival was the only independent risk factor for severe infection (table 2). Thirty-five patients (29.7%) were admitted to a PICU. Presenting leukopenia was an independent risk factor for PICU admission (table 3).
Six patients (5.1%) presented a bad outcome, including two deaths (1.7%). All of them presented an altered PAT and elevated procalcitonin values (>0.5 ng/ml) and were admitted to a PICU with sepsis/septic shock.Conclusion(s): Infants with a LOD by GBS frequently develop sepsis/septic shock and bacterial meningitis with not insignificant morbimortality. No risk factors for severe infection were identified except for the clinical appearance, whereas leukopenia was related to PICU admission.
Table 1. Clinical and epidemiological features and analytical characteristics of the infants with non-severe and severe late-onset Group B streptococcus infections
.png) PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; IQR: interquartile range; ANC: absolute neutrophil count; n.s.: not significant.
PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; IQR: interquartile range; ANC: absolute neutrophil count; n.s.: not significant.Table 2. Multivariate analysis to identify independent risk factors for severe infection
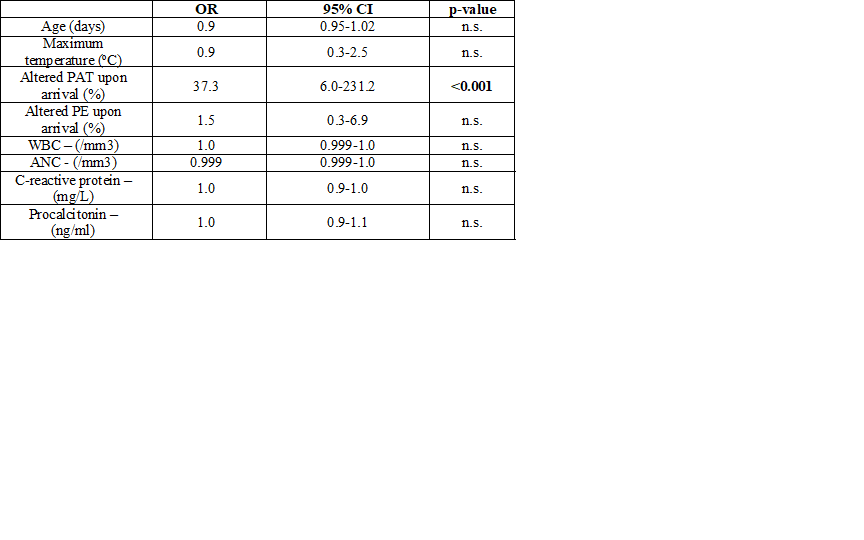 PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; ANC: absolute neutrophil count; OR: odds ratio; CI: confidence interval; n.s.: not significant.
PAT: Pediatric Assessment Triangle; PE: physical examination; WBC: white blood cell count; ANC: absolute neutrophil count; OR: odds ratio; CI: confidence interval; n.s.: not significant.