Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VII
374 - Procalcitonin as a Tool to Diagnose Bacterial Musculoskeletal Infections
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 374
Publication Number: 374.206
Publication Number: 374.206
Lyndsey K. van der Laan, University of Texas Southwestern Medical School, Dallas, TX, United States; Nakia N. Gaines, University of Texas Southwestern Medical School, Dallas, TX, United States; Ngoc L. Van Horn, University of Texas Southwestern Medical School, Dallas, TX, United States; Lawson A. Copley, University of Texas Southwestern Medical School, Dallas, TX, United States

Lyndsey K. van der Laan, MPH, MD
Pediatric Emergency Medicine Fellow
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: The Emergency Department (ED) is often the site of evaluation for children with musculoskeletal infection (MSI). It is challenging to distinguish those with infectious, reactive, inflammatory, neoplastic, or traumatic etiologies during a single, isolated ED visit due to the similarity and overlap of history, physical findings, and laboratory tests, which may evolve over time. Algorithms using clinical and laboratory risk factors, such as the Kocher Criteria, have been utilized with inconsistent findings. Procalcitonin (PCT) has shown promise as a biomarker for MSI in the literature.
Objective: The purpose of this study is to evaluate the merit and accuracy of commonly used clinical and laboratory parameters, including PCT, in the ED assessment of children with suspected MSI.
Design/Methods: Children who presented to the ED from July 2020 to November 2021 with concern for possible MSI were prospectively enrolled. Exclusion criteria: symptom duration > 28 days, pre-treatment with antibiotics, insufficient follow-up, fingertip infections, and failure to obtain a PCT. Follow-up in orthopedic clinic or by telephone determined outcomes of deep infection, superficial infection, and non-infection diagnoses.
Results: 85 met inclusion criteria including: deep infection (n=21); superficial infection (n=10); and no infection (n=54). Fever, WBC, ANC, Hgb, HCT, CRP, ESR and PCT significantly differentiated children with deep infection from those without (Table 1). ROC analysis found the highest AUC for fever, ESR, CRP, and PCT (Table 2). Parameters showed accuracy ranging from 48.2% (inability to bear weight) to 85.9% (Kocher + Caird > 3). PCT >0.1 ng/mL accurately predicted deep infection in 84.7% of cases, outperforming WBC, CRP, and ANC (Table 3). Using ROC cutoffs for CRP (3.3 mg/dL), ESR (18 mm/hr), PCT (0.1 ng/mL), and Temp (37.8° C) accuracy was improved to 89.4%, if 3 of 4 were positive, exceeding the diagnostic accuracy of admission (77.6%).Conclusion(s): There is no single parameter or biomarker which perfectly identifies the presence of MSI. While it is impractical to derive a final diagnosis in the ED, there is value in rapidly determining which children should be 1) admitted for further evaluation, 2) scheduled for an outpatient “second look” by a specialist or 3) allowed to follow up as needed. This study found that using utilizing PCT, CRP, ESR, and fever offers support for predictive judgment of pediatric MSI.
van der Laan CV 12.14.2021CV van der Laan.pdf
Table 2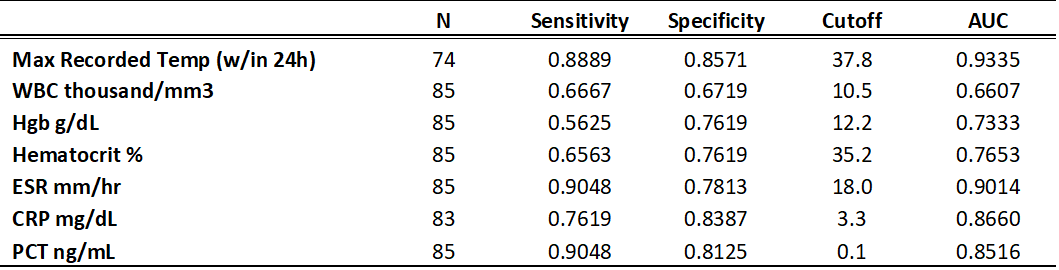 ROC analysis with outcome of deep infection on different variables
ROC analysis with outcome of deep infection on different variables
Objective: The purpose of this study is to evaluate the merit and accuracy of commonly used clinical and laboratory parameters, including PCT, in the ED assessment of children with suspected MSI.
Design/Methods: Children who presented to the ED from July 2020 to November 2021 with concern for possible MSI were prospectively enrolled. Exclusion criteria: symptom duration > 28 days, pre-treatment with antibiotics, insufficient follow-up, fingertip infections, and failure to obtain a PCT. Follow-up in orthopedic clinic or by telephone determined outcomes of deep infection, superficial infection, and non-infection diagnoses.
Results: 85 met inclusion criteria including: deep infection (n=21); superficial infection (n=10); and no infection (n=54). Fever, WBC, ANC, Hgb, HCT, CRP, ESR and PCT significantly differentiated children with deep infection from those without (Table 1). ROC analysis found the highest AUC for fever, ESR, CRP, and PCT (Table 2). Parameters showed accuracy ranging from 48.2% (inability to bear weight) to 85.9% (Kocher + Caird > 3). PCT >0.1 ng/mL accurately predicted deep infection in 84.7% of cases, outperforming WBC, CRP, and ANC (Table 3). Using ROC cutoffs for CRP (3.3 mg/dL), ESR (18 mm/hr), PCT (0.1 ng/mL), and Temp (37.8° C) accuracy was improved to 89.4%, if 3 of 4 were positive, exceeding the diagnostic accuracy of admission (77.6%).Conclusion(s): There is no single parameter or biomarker which perfectly identifies the presence of MSI. While it is impractical to derive a final diagnosis in the ED, there is value in rapidly determining which children should be 1) admitted for further evaluation, 2) scheduled for an outpatient “second look” by a specialist or 3) allowed to follow up as needed. This study found that using utilizing PCT, CRP, ESR, and fever offers support for predictive judgment of pediatric MSI.
van der Laan CV 12.14.2021CV van der Laan.pdf
Table 2
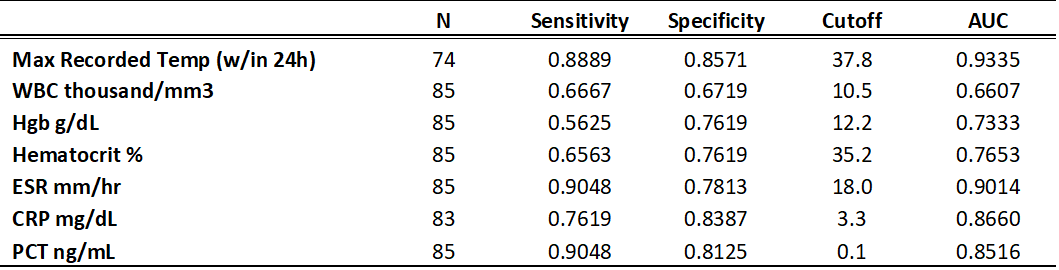 ROC analysis with outcome of deep infection on different variables
ROC analysis with outcome of deep infection on different variables