Quality Improvement/Patient Safety: All Areas
Category: Abstract Submission
Quality Improvement/Patient Safety III - Hospital-based QI and Patient Safety
390 - Quality Improvement for promoting antibiotic stewardship for admitted pediatric patients
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 390
Varshini Gali, Weill Cornell Medicine, New York, NY, United States; Theresa E. Scott, NewYork-Presbyterian Morgan Stanley Children's Hospital/Columbia University Medical Center and NewYork-Presbyterian Komansky Children’s Hospital/Weill Cornell Medical Center, New York, NY, United States; Nicole Gerber, Weill Cornell Medicine, New York, NY, United States; Jin-Young Han, Weill Cornell Medicine, New York, NY, United States; Snezana Nena Osorio, Weill Cornell Medicine, New York, NY, United States

Varshini Gali, BA
Medical Student
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Antibiotic stewardship is important in mitigating development of antibiotic resistant organisms and can be promoted through empiric antibiotic guidelines. At our institution, despite the existence of empiric antibiotic guidelines for pediatric patients, there is still variation in antibiotic prescribing practices, due in part to lack of awareness of the guidelines.
Objective: Increase the proportion of patients in the pediatric ED or the inpatient hospitalist service started on the appropriate empiric antibiotics for skin and soft tissue infections (SSTI), febrile urinary tract infections (UTI), acute osteomyelitis, and pneumonia (PNA) from 70% to 90% by June 2022.
Design/Methods: This observational study with planned sequential experimentation is a QI project underway in the pediatric hospitalist service and ED departments at a large urban medical center. Key stakeholders gathered to develop a driver diagram (Figure 1), tertiary drivers were used to design interventions, which were tested via PDSA cycles. Empiric antibiotic guidelines for febrile UTI, SSTI, PNA and acute osteomyelitis were assessed. We used the following measures: proportion of patients started on empiric antibiotics according to guidelines upon admission (outcome), proportion of providers who aware of the guidelines when prescribing antibiotics, proportion of providers who know how to access the guidelines when prescribing antibiotics (process), and escalation of care (e.g., rapid response team activation and/or transfer to pediatric intensive care unit (balancing). Measures were gathered via record review and baseline data was collected from 10/2020 through 3/2021. To date, one PDSA cycle was completed. Run charts are used to display/analyze the data. Run chart rules are applied to detect signal of change.
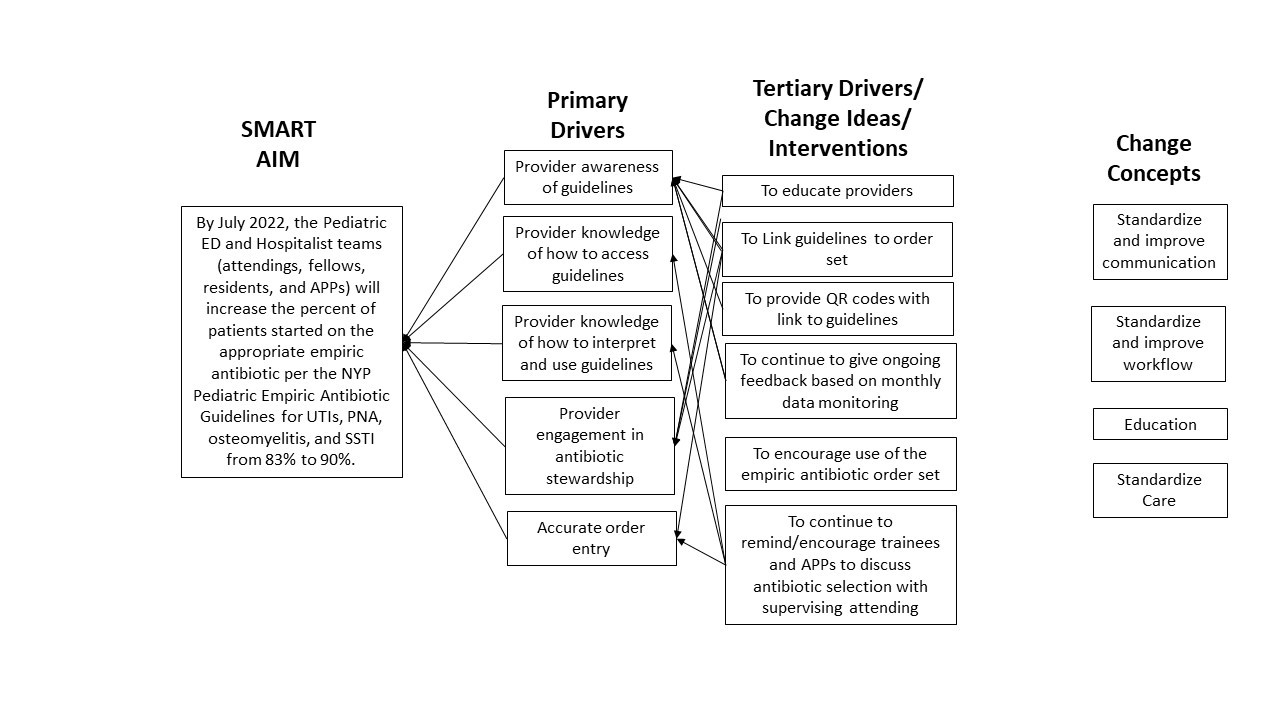
Results: To date, we reviewed 137 electronic health records. Overall median compliance with antibiotic guidelines was high (82.8%, Figure 2). Median guideline compliance by infectious category including UTI, SSTI, and PNA was 100%, 87.5%, and 83.5%, respectively. Out of five cases of osteomyelitis two cases were not compliant. Survey results demonstrated that 39% of providers were not aware of the guidelines, and of those aware of the guidelines, 35% did not know how to access them. Escalation of care was not required in any cases.Conclusion(s): Overall compliance with antibiotic prescribing guidelines was high. Next steps include repeat surveying of provider awareness levels after the education initiative and soliciting feedback from family and staff members on this stewardship initiative.
Figure 1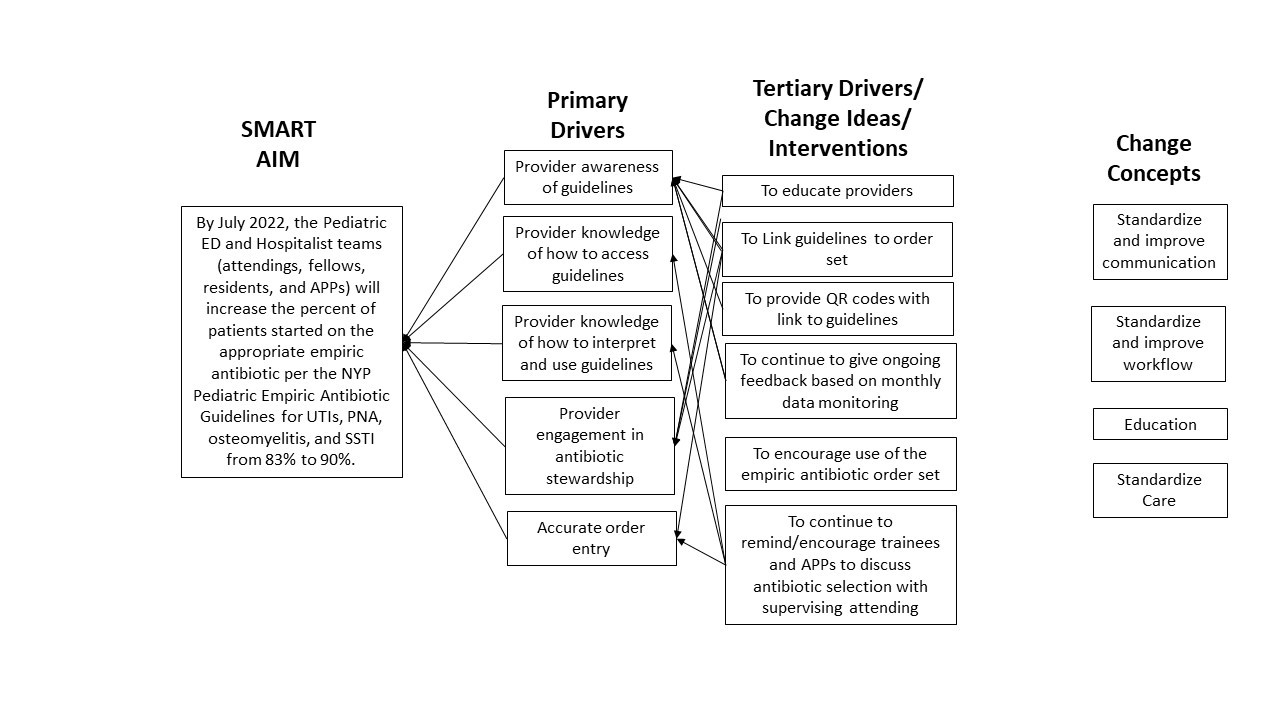 Key Driver Diagram
Key Driver Diagram
Figure 2.jpg) Run chart displaying baseline data, provider survey, and provider educational intervention
Run chart displaying baseline data, provider survey, and provider educational intervention
Objective: Increase the proportion of patients in the pediatric ED or the inpatient hospitalist service started on the appropriate empiric antibiotics for skin and soft tissue infections (SSTI), febrile urinary tract infections (UTI), acute osteomyelitis, and pneumonia (PNA) from 70% to 90% by June 2022.
Design/Methods: This observational study with planned sequential experimentation is a QI project underway in the pediatric hospitalist service and ED departments at a large urban medical center. Key stakeholders gathered to develop a driver diagram (Figure 1), tertiary drivers were used to design interventions, which were tested via PDSA cycles. Empiric antibiotic guidelines for febrile UTI, SSTI, PNA and acute osteomyelitis were assessed. We used the following measures: proportion of patients started on empiric antibiotics according to guidelines upon admission (outcome), proportion of providers who aware of the guidelines when prescribing antibiotics, proportion of providers who know how to access the guidelines when prescribing antibiotics (process), and escalation of care (e.g., rapid response team activation and/or transfer to pediatric intensive care unit (balancing). Measures were gathered via record review and baseline data was collected from 10/2020 through 3/2021. To date, one PDSA cycle was completed. Run charts are used to display/analyze the data. Run chart rules are applied to detect signal of change.
Results: To date, we reviewed 137 electronic health records. Overall median compliance with antibiotic guidelines was high (82.8%, Figure 2). Median guideline compliance by infectious category including UTI, SSTI, and PNA was 100%, 87.5%, and 83.5%, respectively. Out of five cases of osteomyelitis two cases were not compliant. Survey results demonstrated that 39% of providers were not aware of the guidelines, and of those aware of the guidelines, 35% did not know how to access them. Escalation of care was not required in any cases.Conclusion(s): Overall compliance with antibiotic prescribing guidelines was high. Next steps include repeat surveying of provider awareness levels after the education initiative and soliciting feedback from family and staff members on this stewardship initiative.
Figure 1
 Key Driver Diagram
Key Driver DiagramFigure 2
.jpg) Run chart displaying baseline data, provider survey, and provider educational intervention
Run chart displaying baseline data, provider survey, and provider educational intervention