Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation III
497 - Text-Message Videos to Prepare Pregnant Women for Neonatal Resuscitation Decision Making
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 497
Publication Number: 497.232
Publication Number: 497.232
Siobhan M. McDonnell, Medical College of Wisconsin, Germantown, WI, United States; Kathryn E. Flynn, Medical College of Wisconsin, MIlwaukee, WI, United States; Michael B. Pitt, University of Minnesota, Minneapolis, MN, United States; Jennifer J. McIntosh, Medical College of Wisconsin, Milwaukee, WI, United States; Kris A. Pizur-Barnekow, Families First, LLC, Eagle River, WI, United States; Una O. Kim, NorthShore University HealthSystem, Crystal Lake, IL, United States; Ruta Brazauskas, Medical College of Wisconsin, MILWAUKEE, WI, United States; Sheikh I. Ahamed, Marquette University, Milwaukee’s, WI, United States; Mir A. Basir, Medical College of Wisconsin, Wauwatosa, WI, United States
- SM
Siobhan M. McDonnell, MS (she/her/hers)
Clinical Research Assistant
Medical College of Wisconsin
Willmar, Minnesota, United States
Presenting Author(s)
Background: Preterm birth at 22-24 weeks gestational age (GA) is in the “gray zone” of viability. At this GA, the American College of Obstetricians and Gynecologists (ACOG) recommends that parents decide whether or not to initiate neonatal resuscitation at birth. However, pregnant women (PW) with preterm birth risk factors are usually not given information during prenatal care on the “gray zone” and the associated treatment options. This leaves parents unprepared for neonatal resuscitation decision making. To bridge this gap, we created the Preemie Prep for Parents (P3) smartphone program.
Objective: Determine if PW diagnosed with preterm birth risk factors will utilize the P3 program and learn about neonatal resuscitation decision making.
Design/Methods: This is an ancillary analysis of a larger study, ClinicalTrials.gov NCT04093492. Based on neonatal resuscitation guidelines, a multidisciplinary team (parents, clinicians, and health literacy experts) drafted 7 animated videos. Each video was tested in 4-6 lay users for understanding. 120 PW with preterm birth risk factors (multiples, short cervix, diabetes, hypertension, prior preterm birth or preeclampsia) were randomized 1:1 at 18-21 weeks GA to the P3 or ACOG group. The P3 group received text-messages with links to the P3 videos and the ACOG group received links to ACOG educational webpages. We measured PROMIS Anxiety at baseline, then knowledge of neonatal resuscitation decision making and PROMIS Anxiety at 25 weeks GA. Software tracked P3 video usage.
Results: Titles of the 7 neonatal resuscitation decision making videos and their use by PW are in Table 1. Of the P3 PW, 25% utilized all 7 videos and 62% utilized more than 1 video. When PW started a video, they utilized its entirety 85% of the time. Knowledge was greater in the P3 group than the ACOG group for information required for neonatal resuscitation decision making, including GA limit of viability (p < 0.001) and the potential treatment options (p < 0.001; Table 2). Among P3 PW, those who utilized the videos demonstrated greater knowledge than those who did not (Table 3). Anxiety in the P3 group did not change from baseline (p=0.753).Conclusion(s): To our knowledge, this is the first study preparing potential neonatal resuscitation decision makers during the prenatal period. Potential decision makers utilized the P3 videos without heightened anxiety and were more knowledgeable about information necessary for neonatal resuscitation decision making. The unique education offered in the P3 program may benefit at-risk parents.
Table 1.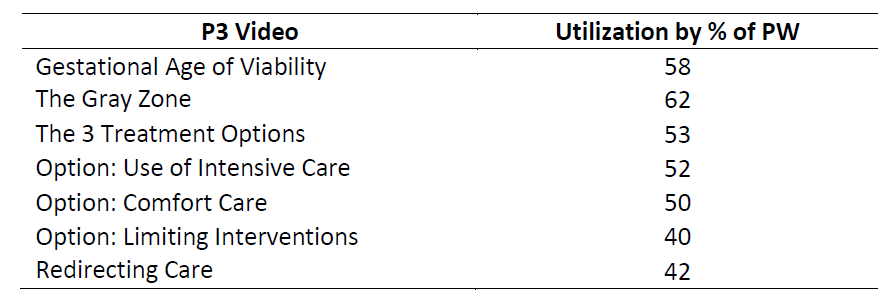 Proportion of pregnant women who utilized each neonatal resuscitation video.
Proportion of pregnant women who utilized each neonatal resuscitation video.
Table 2.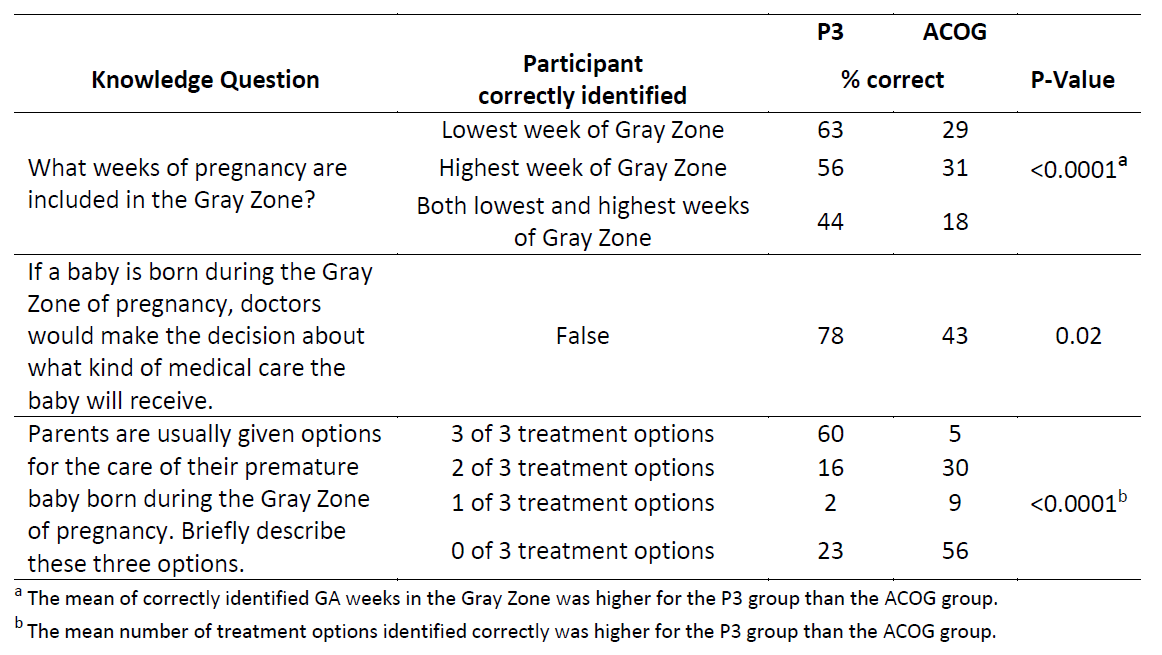 Knowledge items answered correctly by participating pregnant women.
Knowledge items answered correctly by participating pregnant women.
Objective: Determine if PW diagnosed with preterm birth risk factors will utilize the P3 program and learn about neonatal resuscitation decision making.
Design/Methods: This is an ancillary analysis of a larger study, ClinicalTrials.gov NCT04093492. Based on neonatal resuscitation guidelines, a multidisciplinary team (parents, clinicians, and health literacy experts) drafted 7 animated videos. Each video was tested in 4-6 lay users for understanding. 120 PW with preterm birth risk factors (multiples, short cervix, diabetes, hypertension, prior preterm birth or preeclampsia) were randomized 1:1 at 18-21 weeks GA to the P3 or ACOG group. The P3 group received text-messages with links to the P3 videos and the ACOG group received links to ACOG educational webpages. We measured PROMIS Anxiety at baseline, then knowledge of neonatal resuscitation decision making and PROMIS Anxiety at 25 weeks GA. Software tracked P3 video usage.
Results: Titles of the 7 neonatal resuscitation decision making videos and their use by PW are in Table 1. Of the P3 PW, 25% utilized all 7 videos and 62% utilized more than 1 video. When PW started a video, they utilized its entirety 85% of the time. Knowledge was greater in the P3 group than the ACOG group for information required for neonatal resuscitation decision making, including GA limit of viability (p < 0.001) and the potential treatment options (p < 0.001; Table 2). Among P3 PW, those who utilized the videos demonstrated greater knowledge than those who did not (Table 3). Anxiety in the P3 group did not change from baseline (p=0.753).Conclusion(s): To our knowledge, this is the first study preparing potential neonatal resuscitation decision makers during the prenatal period. Potential decision makers utilized the P3 videos without heightened anxiety and were more knowledgeable about information necessary for neonatal resuscitation decision making. The unique education offered in the P3 program may benefit at-risk parents.
Table 1.
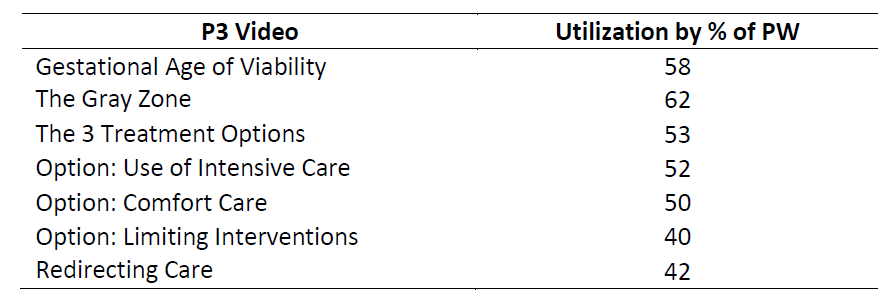 Proportion of pregnant women who utilized each neonatal resuscitation video.
Proportion of pregnant women who utilized each neonatal resuscitation video.Table 2.
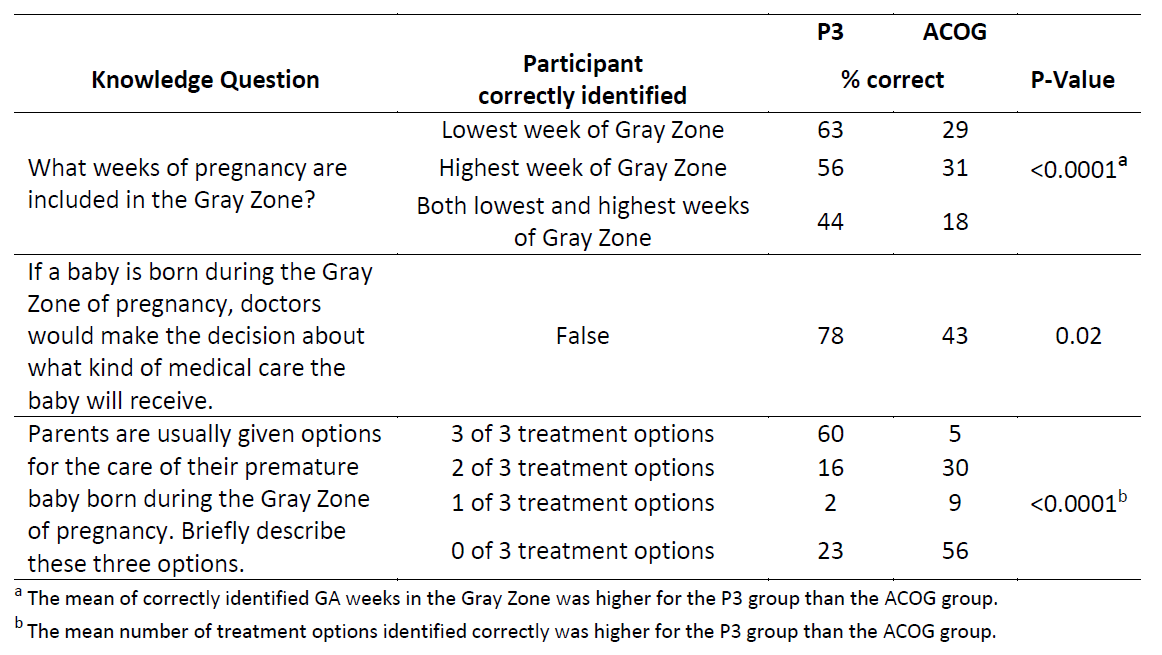 Knowledge items answered correctly by participating pregnant women.
Knowledge items answered correctly by participating pregnant women.