Back
Obesity
Category: Abstract Submission
Obesity I
515 - The Meaning of Genetic Obesity: Parental Perception of Genetic Testing for Children with Obesity
Saturday, April 23, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 515
Publication Number: 515.238
Publication Number: 515.238
Eileen A. Chaves, Nationwide Children's Hospital, Columbus, OH, United States; Amy R. Sharn, Naitonwide Children's Hospital Center for Healthy Weight & Nutrition, Columbus, OH, United States; Milena Senko, Nationwide Children's Hospital, Columbus, OH, United States; Jinyu Xu, Nationwide Children's Hospital, Columbus, OH, United States; Eneli U. Ihuoma, Nationwide Childrens Hospital/Ohio State University, Columbus, OH, United States
Eileen Chaves, PhD, MSc (she/her/hers)
Pediatric Psychologist/Assistant Clinical Professor of Pediatrics
Nationwide Children's Hospital
Worthington, Ohio, United States
Presenting Author(s)
Background: Recent studies suggest genes account for 40-80% of obesity risk. Children with certain gene mutations or variants may present with hyperphagia, reduced satiety, and suboptimal energy expenditure which are amplified in an obesogenic environment. Testing for polygenic risks for obesity in the clinical setting is increasing. Yet, how parents decide on testing for their child and their understanding of the results, particularly if negative or variants of unknown significance (VUS) is unclear. In addition, VUS results can be challenging for clinicians to know how to adequately counsel families due their uncertainty which further complicates how families with children with severe obesity understand the genetic test results.
Objective: Examine caregiver reasoning to have their child undergo polygenic testing for obesity and parental perceptions of genetic test results in order to better inform clinical care.
Design/Methods: This study used a mixed methods design. Inclusion criteria included participation in a study testing for mutations on the Melanocortin-4 Receptor (MC4R) pathway, aged 2-17 years, and history of severe obesity and hyperphagia. Caregiver-child dyads were recruited to ensure equal representation of genetic results across racial/ethnic subgroups (Non-Hispanic White, Black, Hispanic). A third of participants in the main study enrolled in the sub-study. Participants completed the Food Nutrition and Physical Activity Questionnaire (FNPA), where increasing score indicates more positive health behaviors and a survey measure of demographics (NHANES). Family functioning was assessed with the McMaster Family Assessment Device (FAD). Structured caregiver interviews were analyzed using grounded theory.
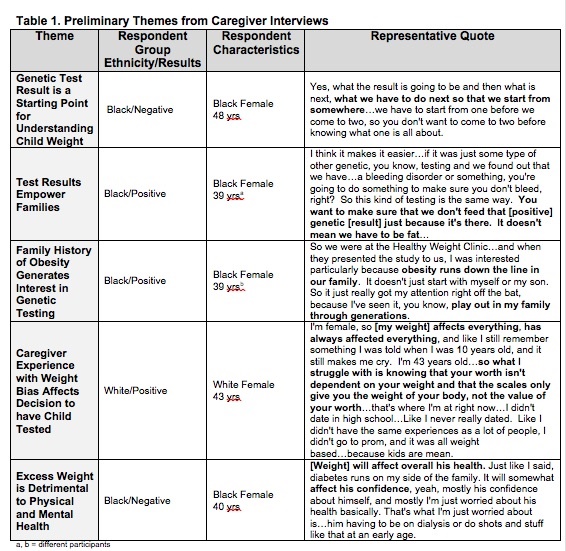
Results: Of the 20 caregivers, all were female, 55% were White, 45% Black and 5% Hispanic. The mean age was 42.3±6.5 years and BMI 40.5±7.9 kg/m2. Most of the children were male (55%), mean age and BMI were 10.0±4.7 years and 40.8±9.9 kg/m2, respectively. Mean FNPA score was 55.4±6.4 and 70% had non-problematic family functioning. Preliminary themes include genetic test result is starting point for understanding child weight status and having test results empower families. Additional themes included in Table 1.Conclusion(s): Caregivers expressed that having genetic testing helps to inform treatment decisions for their child's obesity. Understanding caregiver perceptions and expectations can guide clinicians on counseling and in the development of a clinical decision pathway for genetic testing for obesity.
Table 1. Preliminary Themes from Caregiver Interviews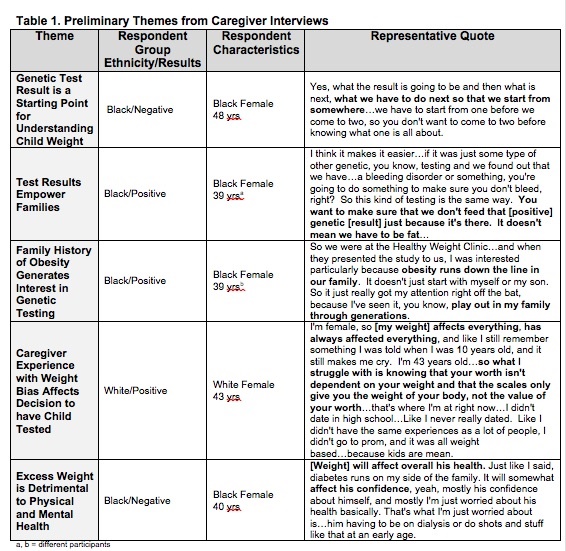
Objective: Examine caregiver reasoning to have their child undergo polygenic testing for obesity and parental perceptions of genetic test results in order to better inform clinical care.
Design/Methods: This study used a mixed methods design. Inclusion criteria included participation in a study testing for mutations on the Melanocortin-4 Receptor (MC4R) pathway, aged 2-17 years, and history of severe obesity and hyperphagia. Caregiver-child dyads were recruited to ensure equal representation of genetic results across racial/ethnic subgroups (Non-Hispanic White, Black, Hispanic). A third of participants in the main study enrolled in the sub-study. Participants completed the Food Nutrition and Physical Activity Questionnaire (FNPA), where increasing score indicates more positive health behaviors and a survey measure of demographics (NHANES). Family functioning was assessed with the McMaster Family Assessment Device (FAD). Structured caregiver interviews were analyzed using grounded theory.
Results: Of the 20 caregivers, all were female, 55% were White, 45% Black and 5% Hispanic. The mean age was 42.3±6.5 years and BMI 40.5±7.9 kg/m2. Most of the children were male (55%), mean age and BMI were 10.0±4.7 years and 40.8±9.9 kg/m2, respectively. Mean FNPA score was 55.4±6.4 and 70% had non-problematic family functioning. Preliminary themes include genetic test result is starting point for understanding child weight status and having test results empower families. Additional themes included in Table 1.Conclusion(s): Caregivers expressed that having genetic testing helps to inform treatment decisions for their child's obesity. Understanding caregiver perceptions and expectations can guide clinicians on counseling and in the development of a clinical decision pathway for genetic testing for obesity.
Table 1. Preliminary Themes from Caregiver Interviews