Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VI
363 - Ultrasound Guided Peripheral IV Access Curriculum for the Pediatric Emergency Department: a pilot study.
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 363
Publication Number: 363.205
Publication Number: 363.205
Samuel Dillman, Children's Mercy Hospitals and Clinics, PRAIRIE VILLAGE, KS, United States; Chris Kennedy, Children's Mercy Hospitals and Clinics, kansas city, MO, United States; Frances Turcotte Benedict, Children's Mercy Hospitals and Clinics, Overland Park, KS, United States

Samuel Dillman, MD
Pediatric Emergency Medicine Fellow
Children's Mercy Hospitals and Clinics
PRAIRIE VILLAGE, Kansas, United States
Presenting Author(s)
Background:
Up to 50% of children have difficult venous access. Studies in the Pediatric Emergency department (PED) have shown that ultrasound guided peripheral IV (USGPIV) access has decreased IV access time and ED length of stay. Barriers for use include lack of training and comfort with the procedure.
Objective: Our objectives are to pilot and evaluate USGPIV training for Pediatric Emergency Medicine (PEM) physicians and nurses.
Design/Methods: The course included a 4-hour, hands-on session with US IV training using a blue phantom task trainer in conjunction with the Vascular Access Team (VAT) for PEM physicians and nurses. Participants’ skills were accessed by the trainers in two ways: 1. Consensus-based stepwise checklist 2. Global assessment of performance (1=Novice to 5= Expert). Obtained pre and post course and participant self-assessments by web-based survey (RedCap). Self-reported confidence with USGPIV was collected pre and post training and 3 months after training. Pre-post confidence mean scores were calculated for each participant and compared using a paired t-test (p value of < .05). Data collection included discipline and prior traditional IV or ultrasound experience. Course-based questions included if the training was an appropriate use of time, would be recommended to colleagues, and if it would be utilized in future practice. (5-point Likert scales: e.g. Novice to expert).
Results: 23 providers were trained, 65% PEM physicians and 35% nurses. Skills assessment results for all participants are presented in table 1 with scores indicating an excellent rating (mean of 439) with subjective ratings most frequently indicating a competent trainee. Table 2 illustrates a statistically significant increase in self-reported confidence in USGPIV placement post training (p < 0.0003). Three months post survey, confidence in skills significantly decreased (p < 0.01). Table 3 illustrates that trainees recommend training to other providers, thought it was a good use of their time, and agreed they would utilize USGPIV access in their clinical practice. Conclusion(s): The training to date has shown acceptability, perceived increase in confidence, and excellent scores on training evaluations. Confidence decreased 4 months post training. Further steps include quality improvement of decreasing time to IV access in difficult access patients through utilization of USGPIV with patient data showing a 56-minute time to IV access for difficult venous access patients at our institution.
CV DillmanCV Dillman .pdf
Table 2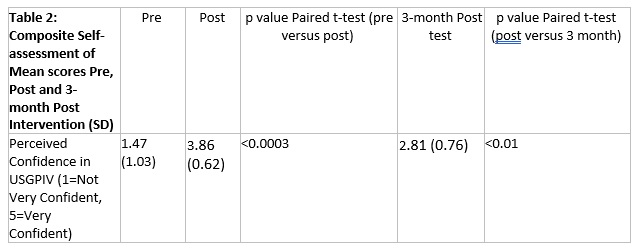 Composite Self-assessment of Mean scores Pre, Post and 3- month Post Intervention (SD)
Composite Self-assessment of Mean scores Pre, Post and 3- month Post Intervention (SD)
Up to 50% of children have difficult venous access. Studies in the Pediatric Emergency department (PED) have shown that ultrasound guided peripheral IV (USGPIV) access has decreased IV access time and ED length of stay. Barriers for use include lack of training and comfort with the procedure.
Objective: Our objectives are to pilot and evaluate USGPIV training for Pediatric Emergency Medicine (PEM) physicians and nurses.
Design/Methods: The course included a 4-hour, hands-on session with US IV training using a blue phantom task trainer in conjunction with the Vascular Access Team (VAT) for PEM physicians and nurses. Participants’ skills were accessed by the trainers in two ways: 1. Consensus-based stepwise checklist 2. Global assessment of performance (1=Novice to 5= Expert). Obtained pre and post course and participant self-assessments by web-based survey (RedCap). Self-reported confidence with USGPIV was collected pre and post training and 3 months after training. Pre-post confidence mean scores were calculated for each participant and compared using a paired t-test (p value of < .05). Data collection included discipline and prior traditional IV or ultrasound experience. Course-based questions included if the training was an appropriate use of time, would be recommended to colleagues, and if it would be utilized in future practice. (5-point Likert scales: e.g. Novice to expert).
Results: 23 providers were trained, 65% PEM physicians and 35% nurses. Skills assessment results for all participants are presented in table 1 with scores indicating an excellent rating (mean of 439) with subjective ratings most frequently indicating a competent trainee. Table 2 illustrates a statistically significant increase in self-reported confidence in USGPIV placement post training (p < 0.0003). Three months post survey, confidence in skills significantly decreased (p < 0.01). Table 3 illustrates that trainees recommend training to other providers, thought it was a good use of their time, and agreed they would utilize USGPIV access in their clinical practice. Conclusion(s): The training to date has shown acceptability, perceived increase in confidence, and excellent scores on training evaluations. Confidence decreased 4 months post training. Further steps include quality improvement of decreasing time to IV access in difficult access patients through utilization of USGPIV with patient data showing a 56-minute time to IV access for difficult venous access patients at our institution.
CV DillmanCV Dillman .pdf
Table 2
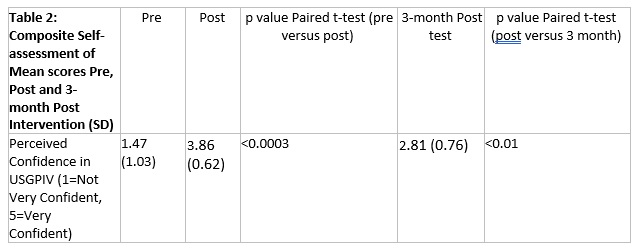 Composite Self-assessment of Mean scores Pre, Post and 3- month Post Intervention (SD)
Composite Self-assessment of Mean scores Pre, Post and 3- month Post Intervention (SD)