Obesity
Category: Abstract Submission
Obesity I
516 - Weight gain trajectories to distinguish children with Rapid-onset Obesity with Hypothalamic dysfunction, Hypoventilation, and Autonomic Dysregulation (ROHHAD) vs. non-syndromic obesity
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 516
Publication Number: 516.238
Publication Number: 516.238
Kamya L. Bijawat, Northwestern University The Feinberg School of Medicine, Redmond, WA, United States; Casey Rand, Ann & Robert H. Lurie Children's Hospital of Chicago, chicago, IL, United States; Tracey Stewart, Lurie Children's Hospital, Chicago, IL, United States; Debra E. Weese-Mayer, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
.jpg)
Kamya L. Bijawat, BA
Medical Student (Fourth Year)
Northwestern University The Feinberg School of Medicine
Redmond, Washington, United States
Presenting Author(s)
Background: ROHHAD presents as rapid weight gain over a limited time period in seemingly healthy children ages 1.5-10 years. If identification is delayed, affected children are at risk of death from cardiorespiratory failure. However, an accessible/consistent biomarker to distinguish ROHHAD from non-syndromic obesity patients is elusive. We hypothesized that the weight gain trajectory may serve as an early biomarker to distinguish ROHHAD from non-syndromic obesity.
Objective: To evaluate the weight gain trajectory of ROHHAD patients compared to non-syndromic obesity patients.
Design/Methods: Serial weights/heights were extracted from medical records for 73 ROHHAD patients and an obese comparison cohort (OCC). OCC included patients in EMR between ages 1.5-10 years who, after 1 or more BMI measurement below the NICHD obesity threshold, met the NICHD obesity diagnostic criteria at later measurement and who did not have any ROHHAD-phenotype-related comorbidities. The distribution of maximum weight gain slopes, maximum percentile slopes, and maximum modified percentile slopes (better reflecting large weight gains >95th percentile at a given age) were determined for ROHHAD and OCC and evaluated for sensitivity and specificity in separating ROHHAD patients from the OCC at different thresholds. Receiver Operator Characteristic (ROC) curves were plotted from these sensitivity and specificity values, and the area under the ROC curve calculated. Significance was applied to p< 0.05.
Results: Adequate records during the rapid-onset weight gain window were identified from 59 ROHHAD patients (50% females) and a 10-fold sized OCC. ROHHAD weight slopes were >OCC, with median maximum gain of 21.5 vs. 7.5 kg/year, respectively (p < 0.05). ROHHAD percentile slopes were >OCC, with median percentile point gain of 80 vs. 4 percentile points/year, respectively (p < 0.05). ROHHAD modified percentile slopes were >OCC, with median modified percentile slope of 125 vs. 21 points/year, respectively (p < 0.05). Higher sensitivity but lower specificity was found for lower slope thresholds (p < 0.05). Percentile slope had lower performance (p < 0.05) than weight and modified percentile slopes, which had similar performance (Figure 1).Conclusion(s): Weight gain trajectory slopes introduce a biomarker to raise suspicion of ROHHAD in a child with rapid weight gain. A composite weight trajectory/endocrine biomarker may provide early identification and introduction of life-saving management before symptoms are irreversible and risk of death from cardiorespiratory failure ensues.
Figure 1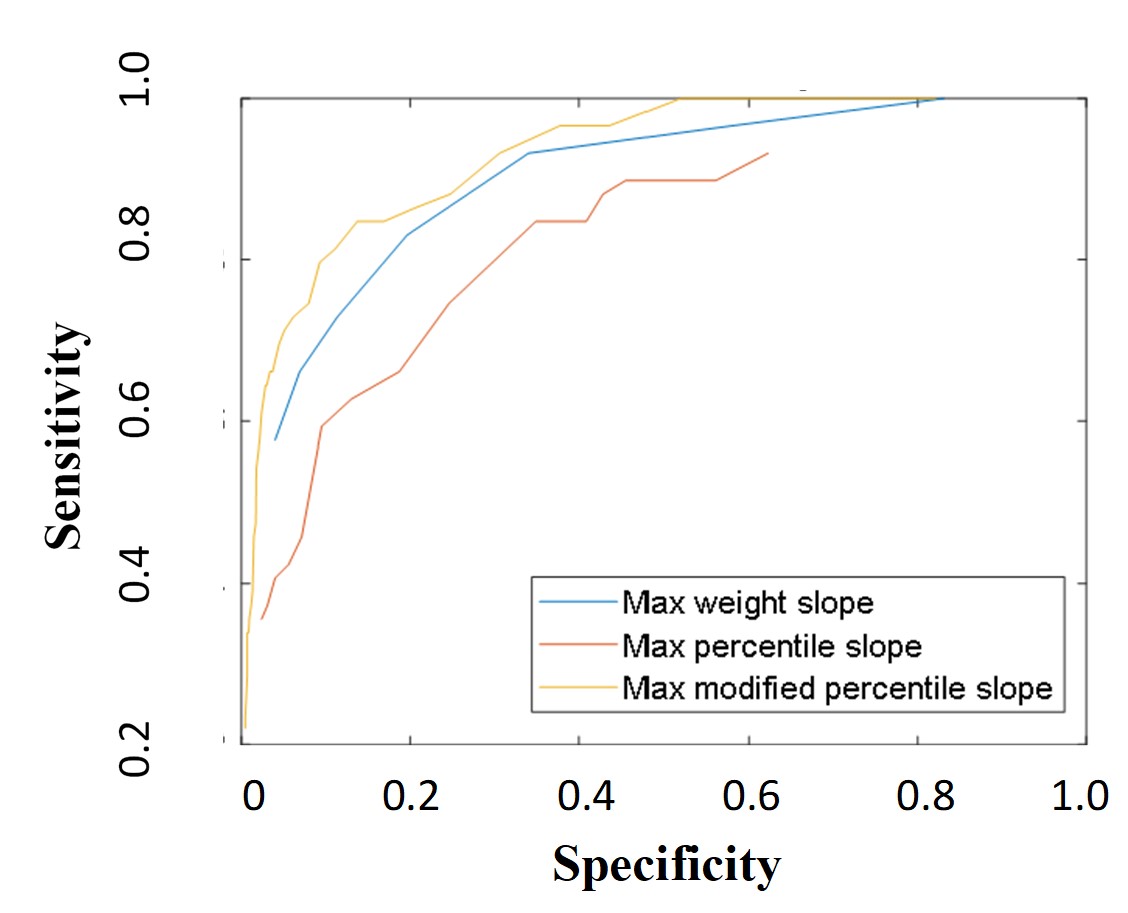 Receiver Operator Characteristic comparison for maximum (max) weight, percentile, and modified percentile slopes comparing ROHHAD and obese comparison patient cohorts
Receiver Operator Characteristic comparison for maximum (max) weight, percentile, and modified percentile slopes comparing ROHHAD and obese comparison patient cohorts
Objective: To evaluate the weight gain trajectory of ROHHAD patients compared to non-syndromic obesity patients.
Design/Methods: Serial weights/heights were extracted from medical records for 73 ROHHAD patients and an obese comparison cohort (OCC). OCC included patients in EMR between ages 1.5-10 years who, after 1 or more BMI measurement below the NICHD obesity threshold, met the NICHD obesity diagnostic criteria at later measurement and who did not have any ROHHAD-phenotype-related comorbidities. The distribution of maximum weight gain slopes, maximum percentile slopes, and maximum modified percentile slopes (better reflecting large weight gains >95th percentile at a given age) were determined for ROHHAD and OCC and evaluated for sensitivity and specificity in separating ROHHAD patients from the OCC at different thresholds. Receiver Operator Characteristic (ROC) curves were plotted from these sensitivity and specificity values, and the area under the ROC curve calculated. Significance was applied to p< 0.05.
Results: Adequate records during the rapid-onset weight gain window were identified from 59 ROHHAD patients (50% females) and a 10-fold sized OCC. ROHHAD weight slopes were >OCC, with median maximum gain of 21.5 vs. 7.5 kg/year, respectively (p < 0.05). ROHHAD percentile slopes were >OCC, with median percentile point gain of 80 vs. 4 percentile points/year, respectively (p < 0.05). ROHHAD modified percentile slopes were >OCC, with median modified percentile slope of 125 vs. 21 points/year, respectively (p < 0.05). Higher sensitivity but lower specificity was found for lower slope thresholds (p < 0.05). Percentile slope had lower performance (p < 0.05) than weight and modified percentile slopes, which had similar performance (Figure 1).Conclusion(s): Weight gain trajectory slopes introduce a biomarker to raise suspicion of ROHHAD in a child with rapid weight gain. A composite weight trajectory/endocrine biomarker may provide early identification and introduction of life-saving management before symptoms are irreversible and risk of death from cardiorespiratory failure ensues.
Figure 1
 Receiver Operator Characteristic comparison for maximum (max) weight, percentile, and modified percentile slopes comparing ROHHAD and obese comparison patient cohorts
Receiver Operator Characteristic comparison for maximum (max) weight, percentile, and modified percentile slopes comparing ROHHAD and obese comparison patient cohorts