General Pediatrics: Primary Care/Prevention
Category: Abstract Submission
General Pediatrics III
165 - A preliminary assessment on the utility of universal pediatric lipid screening in an academic urban practice
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 165
Publication Number: 165.316
Publication Number: 165.316
John W. Harrington, Children's Hospital of The King's Daughters, Norfolk, VA, United States; Wais Mojadedi, Eastern Virginia Medical School, Norfolk, VA, United States; Francis Matilda, Eastern Virginia Medical School, Norfolk, VA, United States; Shreeyas Satish Kumar, Eastern Virginia Medical School, Springfield, VA, United States
John W. Harrington, MD (he/him/his)
Vice-President of Quality/Safety and Clinical Integration
CHKD
Norfolk, Virginia, United States
Presenting Author(s)
Background: 1 in 5 children under 18 years of age has a dyslipidemia. Given this prevalence, a universal screening guideline by the American Academy of Pediatrics (AAP) was implemented.
Objective: To assess if an abnormal screening lipid panel in children ages 9-11 affects a change in management in a single practice.
Design/Methods: A retrospective chart review on children aged 11-14, being followed concurrently over 2-3 years with no heritable dyslipidemia, by General Academic Pediatrics (GAP) at Children's Hospital of The King's Daughters (CHKD) was planned. Abstraction included; demographics, past medical and family history, BMI, lipid panel and related lab studies (including comprehensive metabolic panel, HgbA1C, TSH, and urinalysis), as well as therapies/medications following lipid panel, and referrals. Statistical analysis of categorical variables were assessed using chi-square or Fisher's exact test. A value-based assessment was performed using 2021 Medicare reimbursement levels.
Results: 984 patients were initially identified and 880 patients were included in the study. Of these, 424 patients received a screening lipid panel (48.2%) in accordance with the AAP guidelines, and 136 had at least one abnormal laboratory finding (32.5%). Those with at least one abnormality, 39 patients received a follow-up fasting lipid panel (28.7%), and it was determined that 11.4% of the screenings led to a modification and/or addition to the treatment plan, however no medications. There was no significance noted between the ordering of lipid panels and patient demographics such as gender, family history, or race (p = 0.94, 0.07, 0.22, 95% CI, respectively). Additionally, it was observed that children who received a lipid panel had a significantly higher BMI percentile (mean 79.1 vs 68.8, p < 0.001, 95% CI), and were of slightly younger age (mean 10.3 vs 10.5, p = 0.007, 95% CI). Using the 2021 Medicaid reimbursement schedules for an office visit, lipid panel, and a fasting lipid panel, we estimate a gross total cost of services that did not provide value to the patient at nearly $9989.Conclusion(s): The current guidelines for universal screening of lipid panels in the pediatric setting at age 9-11 remains somewhat controversial, since many children in this age group are never treated with statins. In addition, any management change would have been likely recommended based on their measured BMI. Overall, from a value-based care perspective, the healthcare benefit of lipid screening in children ages 9-11 is minimal and has a conservative increase in cost of $10,000 to one practice over a 2 year period.
Data Table.png) Data Table
Data Table
BMI % Frequencies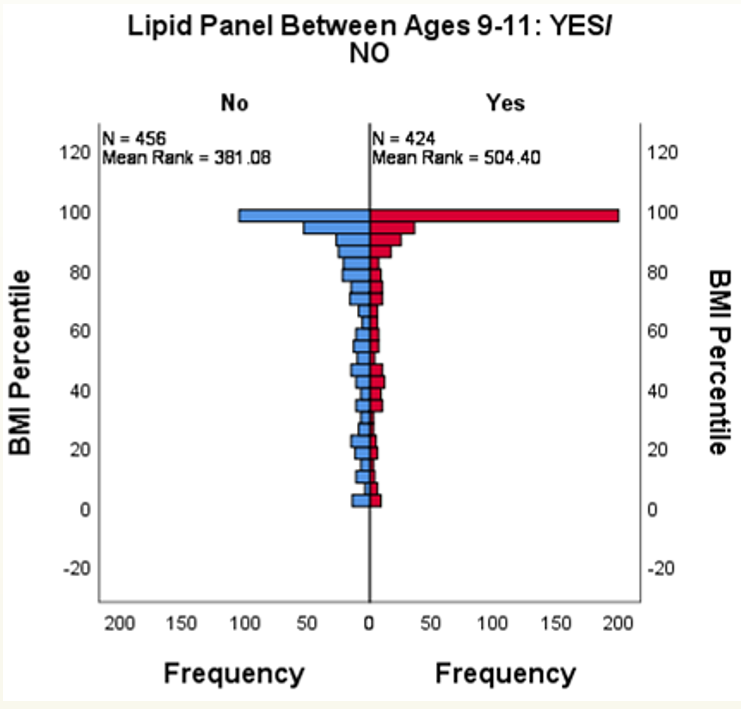 BMI % Frequencies
BMI % Frequencies
Objective: To assess if an abnormal screening lipid panel in children ages 9-11 affects a change in management in a single practice.
Design/Methods: A retrospective chart review on children aged 11-14, being followed concurrently over 2-3 years with no heritable dyslipidemia, by General Academic Pediatrics (GAP) at Children's Hospital of The King's Daughters (CHKD) was planned. Abstraction included; demographics, past medical and family history, BMI, lipid panel and related lab studies (including comprehensive metabolic panel, HgbA1C, TSH, and urinalysis), as well as therapies/medications following lipid panel, and referrals. Statistical analysis of categorical variables were assessed using chi-square or Fisher's exact test. A value-based assessment was performed using 2021 Medicare reimbursement levels.
Results: 984 patients were initially identified and 880 patients were included in the study. Of these, 424 patients received a screening lipid panel (48.2%) in accordance with the AAP guidelines, and 136 had at least one abnormal laboratory finding (32.5%). Those with at least one abnormality, 39 patients received a follow-up fasting lipid panel (28.7%), and it was determined that 11.4% of the screenings led to a modification and/or addition to the treatment plan, however no medications. There was no significance noted between the ordering of lipid panels and patient demographics such as gender, family history, or race (p = 0.94, 0.07, 0.22, 95% CI, respectively). Additionally, it was observed that children who received a lipid panel had a significantly higher BMI percentile (mean 79.1 vs 68.8, p < 0.001, 95% CI), and were of slightly younger age (mean 10.3 vs 10.5, p = 0.007, 95% CI). Using the 2021 Medicaid reimbursement schedules for an office visit, lipid panel, and a fasting lipid panel, we estimate a gross total cost of services that did not provide value to the patient at nearly $9989.Conclusion(s): The current guidelines for universal screening of lipid panels in the pediatric setting at age 9-11 remains somewhat controversial, since many children in this age group are never treated with statins. In addition, any management change would have been likely recommended based on their measured BMI. Overall, from a value-based care perspective, the healthcare benefit of lipid screening in children ages 9-11 is minimal and has a conservative increase in cost of $10,000 to one practice over a 2 year period.
Data Table
.png) Data Table
Data TableBMI % Frequencies
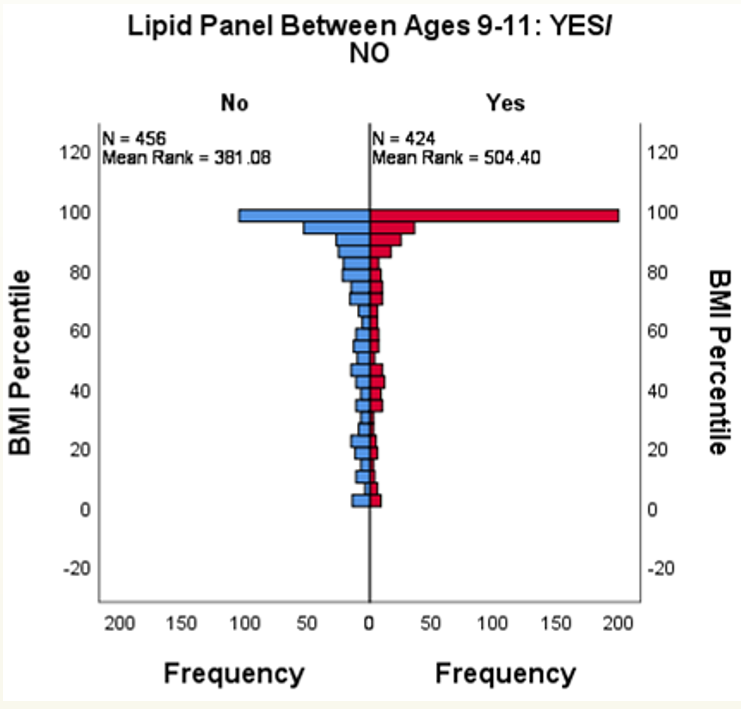 BMI % Frequencies
BMI % Frequencies