Hypertension
Category: Abstract Submission
Hypertension I
77 - Association of self-report of sleep practices with cardiovascular disease risk factors among youth with obesity and elevated blood pressure
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 77
Publication Number: 77.324
Publication Number: 77.324
Jeffrey S. Garofano, Johns Hopkins University, BALTIMORE, MD, United States; Catherine K. Perez, Johns Hopkins Children's Center, Miami, FL, United States; Sruthi Parthasarathy, Johns Hopkins University School of Medicine, Sugar Land, TX, United States; Michael T. Smith, johnshopkinsU, Baltimore, MD, United States; Carisa Parrish, Johns Hopkins Children's Center, Baltimore, MD, United States; Tammy M. Brady, Johns Hopkins University, Baltimore, MD, United States

Jeffrey Garofano, PhD
Instructor
Johns Hopkins University School of Medicine
BALTIMORE, Maryland, United States
Presenting Author(s)
Background: Obesity and elevated blood pressure (BP) in childhood are risk factors for the development of cardiovascular disease (CVD) in adulthood. Self-reported poor sleep in adults is associated with a 48% greater likelihood of developing hypertension; however, evidence on sleep and CVD in children is more limited.
Objective: Among youth with obesity and elevated BP, determine (1) if self-reported sleep practices differ from those reported in the general pediatric population and (2) how their sleep practices relate to CVD risk factors.
Design/Methods: A cross-sectional analysis of youth were evaluated in a multidisciplinary pediatric obesity and hypertension clinic from 5/2021-10/2021. All patients underwent standardized assessment of cardiovascular (CV) functioning and sleep practices (i.e., the Pediatric Sleep Practices Questionnaire, PSPQ), with higher scores reflecting greater severity. Independent sample t-tests and Fisher’s exact test were used for comparisons with a nationally representative sample (Metzer et al., 2021). Associations were evaluated using Spearman’s Rank-Order Correlations.
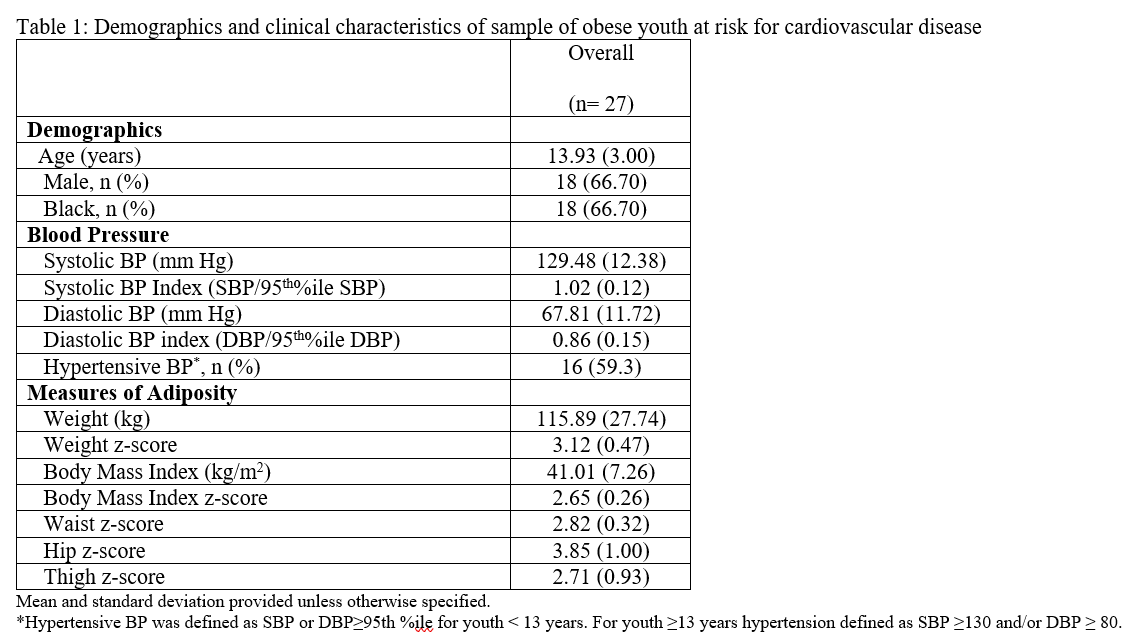
Results: The study’s sample included 27 youth with mean age 13.93 years (SD 3.00), 67% male, and 67% Black. Mean BMI was 41.01 kg/m2 (z-score= 2.65), average of mean triplicate manual BPs was 129/68, and 59% had a hypertensive BP (Table 1). After correction for age, 28% and 16% self-reported insufficient sleep during the week and weekend, respectively. Compared to a nationally representative sample (n=307), the study sample had greater difficulties in 3 of 7 PSPQ indices, including technology use before bed, inconsistent sleep routine, and had higher overall total score (indicating greater sleep difficulty, Table 2). Correlation analyses revealed moderate to strong associations between BP and technology use before bed and change in weekday vs weekend sleep opportunity (Table 3). Adiposity (hip, thigh) had a strong association with sleep opportunity, change in weekday vs weekend sleep opportunity, and total PSPQ score.Conclusion(s): Suboptimal sleep practices, including inconsistent sleep routines and technology use before bed, are more prevalent among youth with obesity and elevated BP than a national sample, with some sleep practices associated with BP and adiposity. Standardized sleep assessment may provide a clinical opportunity to augment CVD risk reduction strategies via improvement of sleep behavior in youth at elevated risk.
Demographics and clinical characteristics of sample of obese youth at risk for cardiovascular disease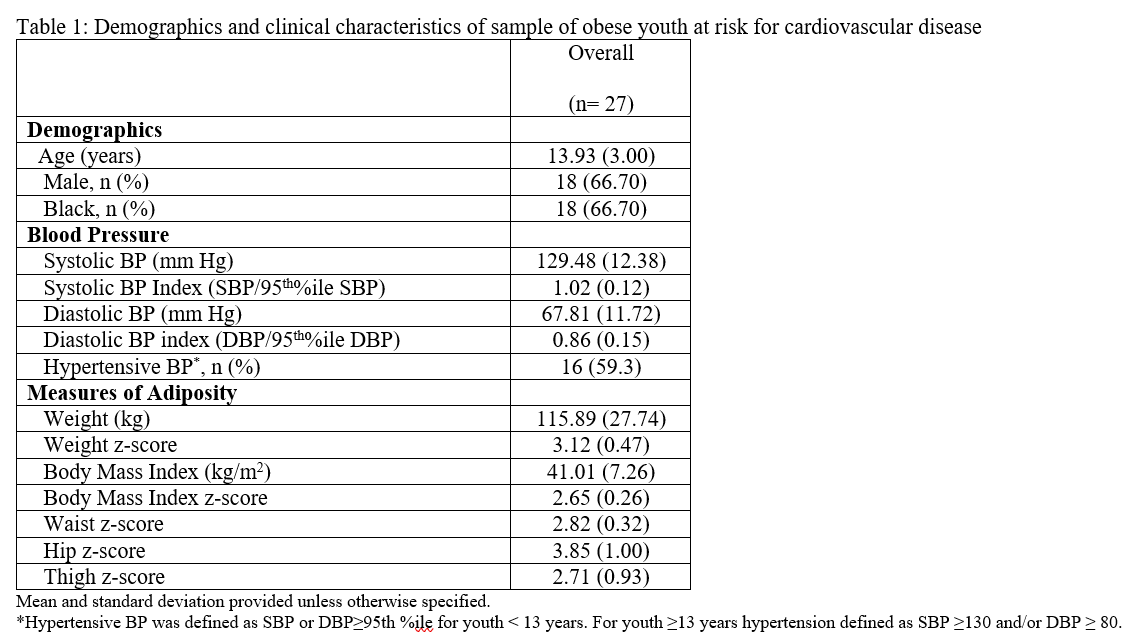
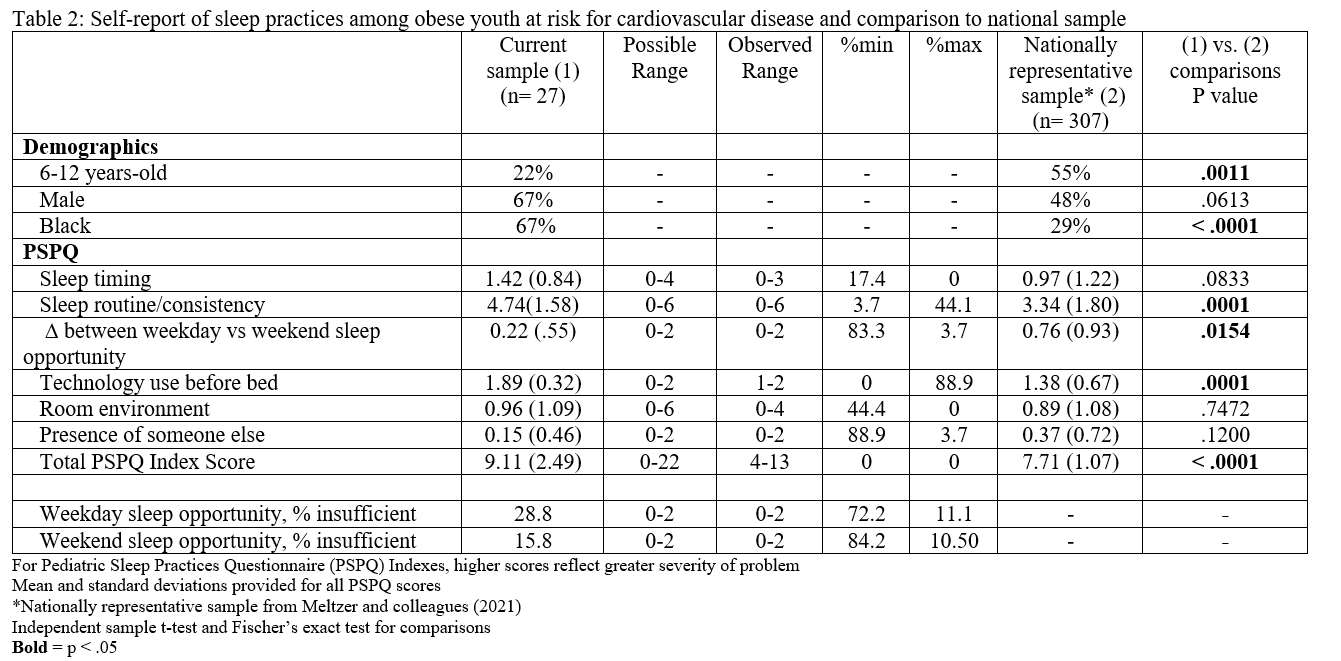
Self-report of sleep practices among obese youth at risk for cardiovascular disease and comparison to national sample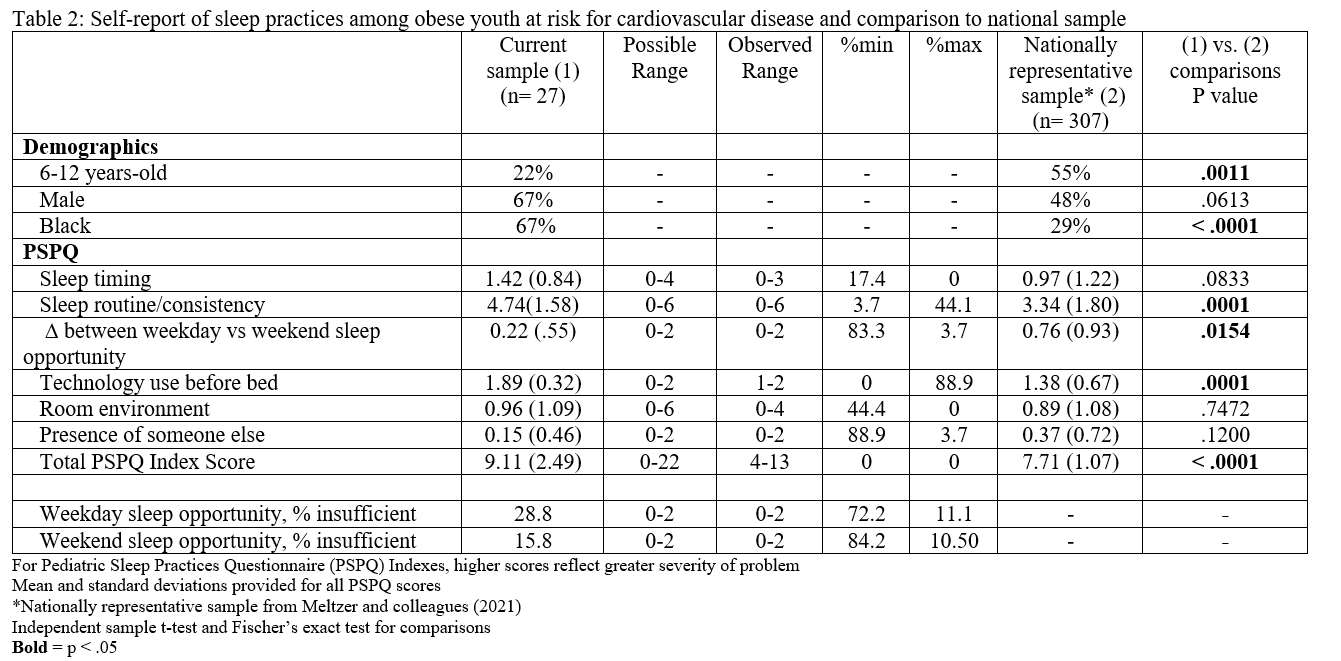
Objective: Among youth with obesity and elevated BP, determine (1) if self-reported sleep practices differ from those reported in the general pediatric population and (2) how their sleep practices relate to CVD risk factors.
Design/Methods: A cross-sectional analysis of youth were evaluated in a multidisciplinary pediatric obesity and hypertension clinic from 5/2021-10/2021. All patients underwent standardized assessment of cardiovascular (CV) functioning and sleep practices (i.e., the Pediatric Sleep Practices Questionnaire, PSPQ), with higher scores reflecting greater severity. Independent sample t-tests and Fisher’s exact test were used for comparisons with a nationally representative sample (Metzer et al., 2021). Associations were evaluated using Spearman’s Rank-Order Correlations.
Results: The study’s sample included 27 youth with mean age 13.93 years (SD 3.00), 67% male, and 67% Black. Mean BMI was 41.01 kg/m2 (z-score= 2.65), average of mean triplicate manual BPs was 129/68, and 59% had a hypertensive BP (Table 1). After correction for age, 28% and 16% self-reported insufficient sleep during the week and weekend, respectively. Compared to a nationally representative sample (n=307), the study sample had greater difficulties in 3 of 7 PSPQ indices, including technology use before bed, inconsistent sleep routine, and had higher overall total score (indicating greater sleep difficulty, Table 2). Correlation analyses revealed moderate to strong associations between BP and technology use before bed and change in weekday vs weekend sleep opportunity (Table 3). Adiposity (hip, thigh) had a strong association with sleep opportunity, change in weekday vs weekend sleep opportunity, and total PSPQ score.Conclusion(s): Suboptimal sleep practices, including inconsistent sleep routines and technology use before bed, are more prevalent among youth with obesity and elevated BP than a national sample, with some sleep practices associated with BP and adiposity. Standardized sleep assessment may provide a clinical opportunity to augment CVD risk reduction strategies via improvement of sleep behavior in youth at elevated risk.
Demographics and clinical characteristics of sample of obese youth at risk for cardiovascular disease
Self-report of sleep practices among obese youth at risk for cardiovascular disease and comparison to national sample