Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Education/Research/QI Potpourri
312 - Bringing Nocturnist Needs into the Light of Day: A Professional Development Needs Assessment of Overnight Hospitalists
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 312
Publication Number: 312.322
Publication Number: 312.322
Grant C. Smith, University of Colorado School of Medicine, Denver, CO, United States; Lauren R. Anderson, University of Colorado, Aurora, CO, United States; Sonja I. Ziniel, University of Colorado School of Medicine, Aurora, CO, United States

Grant C. Smith, MD, MSc
Instructor
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: Since the Accreditation Council for Graduate Medical Education introduced new guidelines in 2011 that emphasized attending supervision of residents, it has become increasingly common for academic children’s hospitals to hire nocturnists to assure around-the-clock attending physician presence. At our institution, the nocturnist role has been filled by early career hospitalists, often directly out of training. Empirically, our nocturnists have found the lack of feedback or collaboration with senior faculty overnight daunting. While some studies have investigated the effect of a nocturnist presence on resident education and safety, little is known about the professional development needs of overnight faculty.
Objective: Describe the current state of performance feedback available to pediatric hospitalist nocturnists and assess faculty feedback needs.
Design/Methods: In the spring of 2021, a web-based survey was distributed to University of Colorado pediatric hospitalist physicians who work overnight shifts at our academic children’s hospital. The survey included questions regarding satisfaction with performance feedback, preferred domains for feedback, and demographics. Participants were additionally asked about interest in participating in peer feedback as a means to improve performance feedback.
Results: Eleven nocturnists completed the survey, a 92% response rate. Nearly all respondents (91%) had finished clinical training within the last five years, and two-thirds worked at least half of their shifts overnight. Fifty-four percent reported never receiving actionable feedback in their nocturnist role. No respondent was “very satisfied” with the amount of feedback received, with 82% reporting no or little satisfaction. Patient care was identified as the area where feedback was most desired, with 73% indicating this was most important, followed by teaching. Respondents were also asked to rate 15 different skills in terms of feedback importance (Figure 1), and among these, direct admission triage was deemed most important, with 73% rating it as “pretty important” or “very important.” All respondents indicated some interest participating in peer feedback.Conclusion(s): Our survey results demonstrate a clear need to provide and improve feedback to early career hospitalists who work overnight, particularly in the domains of clinical care and medical education. With limited personnel overnight, peer feedback may be the most effective strategy for enhancing feedback. Given strong local interest in peer feedback, we plan to develop a formal feedback program.
Specific Feedback Interests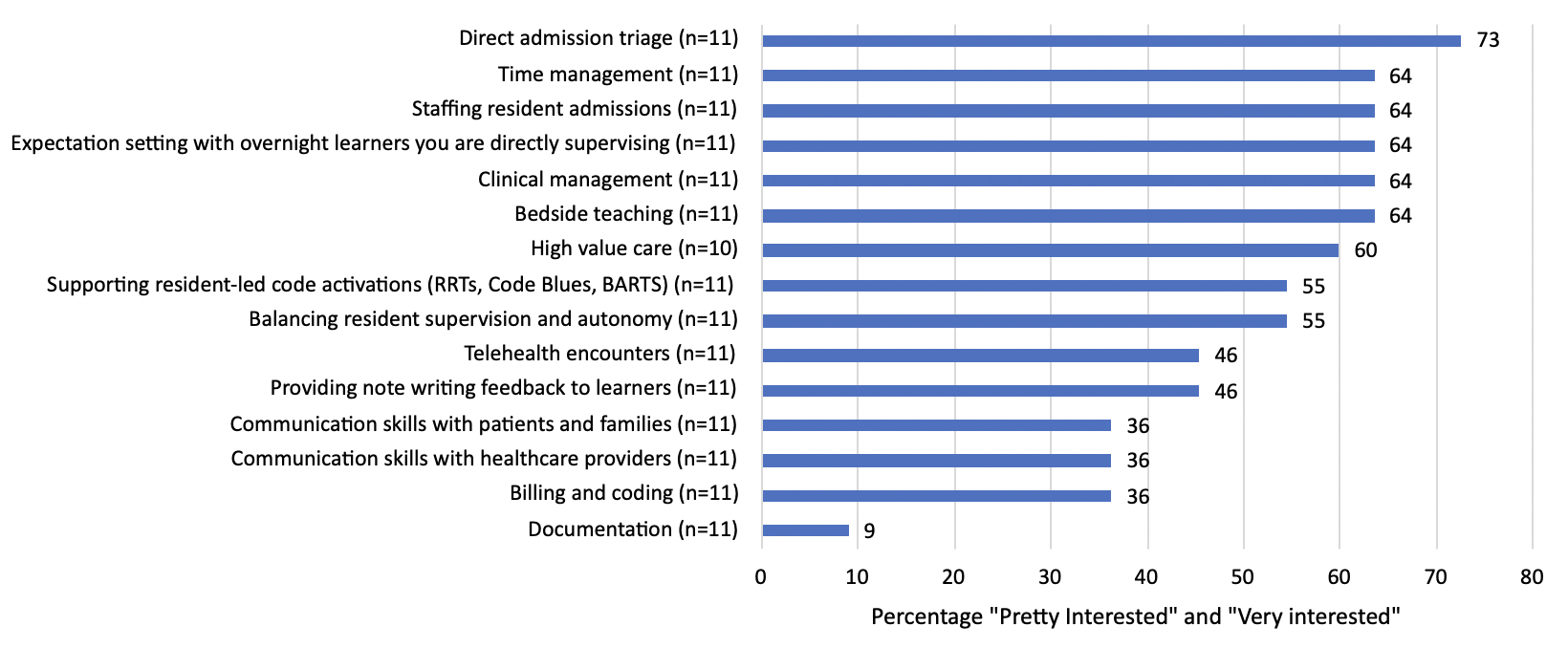 Survey participants rated interest in receiving feedback on 15 skills on a scale from 1 ("not interested") to 5 ("very interested").
Survey participants rated interest in receiving feedback on 15 skills on a scale from 1 ("not interested") to 5 ("very interested").
Objective: Describe the current state of performance feedback available to pediatric hospitalist nocturnists and assess faculty feedback needs.
Design/Methods: In the spring of 2021, a web-based survey was distributed to University of Colorado pediatric hospitalist physicians who work overnight shifts at our academic children’s hospital. The survey included questions regarding satisfaction with performance feedback, preferred domains for feedback, and demographics. Participants were additionally asked about interest in participating in peer feedback as a means to improve performance feedback.
Results: Eleven nocturnists completed the survey, a 92% response rate. Nearly all respondents (91%) had finished clinical training within the last five years, and two-thirds worked at least half of their shifts overnight. Fifty-four percent reported never receiving actionable feedback in their nocturnist role. No respondent was “very satisfied” with the amount of feedback received, with 82% reporting no or little satisfaction. Patient care was identified as the area where feedback was most desired, with 73% indicating this was most important, followed by teaching. Respondents were also asked to rate 15 different skills in terms of feedback importance (Figure 1), and among these, direct admission triage was deemed most important, with 73% rating it as “pretty important” or “very important.” All respondents indicated some interest participating in peer feedback.Conclusion(s): Our survey results demonstrate a clear need to provide and improve feedback to early career hospitalists who work overnight, particularly in the domains of clinical care and medical education. With limited personnel overnight, peer feedback may be the most effective strategy for enhancing feedback. Given strong local interest in peer feedback, we plan to develop a formal feedback program.
Specific Feedback Interests
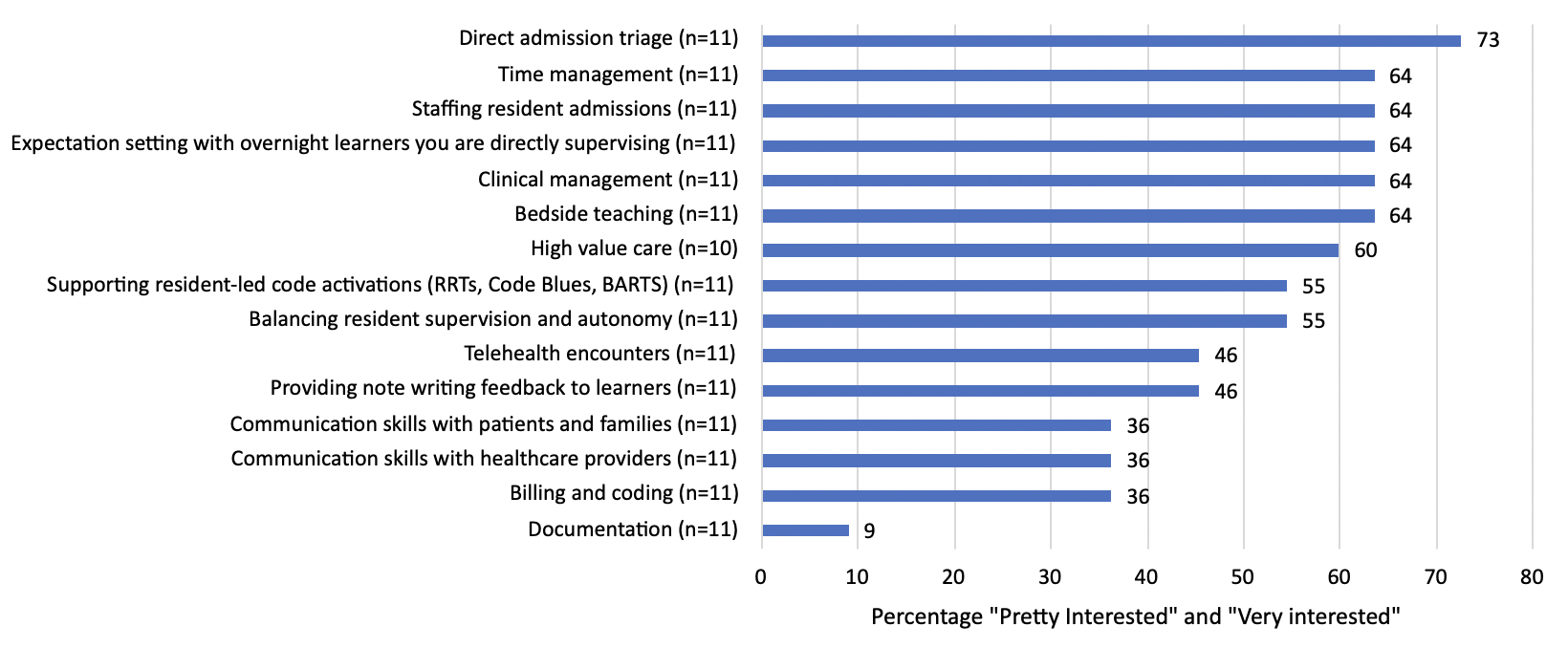 Survey participants rated interest in receiving feedback on 15 skills on a scale from 1 ("not interested") to 5 ("very interested").
Survey participants rated interest in receiving feedback on 15 skills on a scale from 1 ("not interested") to 5 ("very interested").