Hypertension
Category: Abstract Submission
Hypertension I
80 - Can In-vivo Early Gestation Placental Magnetic Resonance Imaging Predict Ischemic Placental Disease?
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 80
Publication Number: 80.324
Publication Number: 80.324
Brian Lee, UCLA Mattel Childrens Hospital, Los Angeles, CA, United States; Arya Aliabadi, UCLA David Geffen School of Medicine, Los Angeles, CA, United States; Kyung H. Sung, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Carla janzen, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Peggy S. Sullivan, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Sherin U. Devaskar, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States

Brian Lee, MD
Fellow
UCLA Mattel Childrens Hospital
Los Angeles, California, United States
Presenting Author(s)
Background: Ischemic placental disease (IPD) manifests clinically as preeclampsia, fetal growth restriction, or placental abruption, and is a risk factor for the development of long-term cardiovascular disorders in both the mother and the neonate. Similar uterine artery Doppler ultrasound findings and placental histology between these conditions suggest a common pathophysiological mechanism in early pregnancy. As the uterine artery pulsatility index (PI) has poor sensitivity and predictive value for IPD, our group developed a novel, multi-parametric (mp-) MRI using a multi-delay, pseudo-continuous arterial-spin-labeling sequence (pCASL) to simultaneously measure placental structure and function.
Objective: Our objective is to test the hypothesis that placental mp-MRI in early pregnancy can aid in the prediction of IPD, impacting maternal and neonatal cardiovascular disease.
Design/Methods: 200 women were recruited in the first trimester of pregnancy. We recorded the pregnancy course through four visits (at 11-14 weeks, 19-22 weeks, 36 weeks, and at delivery), focusing on the development of IPD. Uterine artery Doppler ultrasound was performed at 11-14 and 19-22 weeks of gestation. Placental pCASL mp-MRI was performed at 14-16 and 19-22 weeks of gestation. Imaging software was used to measure maternal to placental blood flow (PBF), regions of high placental blood flow (hPBF), and placental volume.
Results: 179 maternal-infant dyads were analyzed. 44 women developed IPD (24.5%), and 135 women did not develop IPD (75.5%).
At the first MRI timepoint (14-16 weeks), there were 117 controls and 44 IPD cases with MRI scans. There was no difference in placental volume or arterial transit time (ATT) between the groups (p = 0.71 and p = 0.26, respectively). In contrast, PBF was significantly lower in the IPD group than the control group (55.9 mL/min vs 64.2 mL/min respectively, p = 0.043; Figure 1). hPBF was also significantly lower in the IPD group than the control group (192.2 vs. 238.8 mL/min, p = 0.01; Figure 2).
At the second MRI timepoint (19-22 weeks), there were 111 controls and 42 IPD cases with MRI scans. There was no difference in placental volume or ATT between the groups (p = 0.85 and p = 0.39, respectively). In contrast to the first MRI timepoint, there was no significant difference in PBF or hPBF between the groups (p = 0.32 and p = 0.16, respectively).Conclusion(s): pCASL mp-MRI of early-gestation (14-16 weeks) placental blood flow may predict IPD. Our studies potentially have a major impact on maternal and neonatal development of long-term cardiovascular disease.
Supported by NIH U01-HD087221
Brian Lee _ Curriculum Vitae.pdf
Figure 2: high Placental blood flow at first MRI timepoint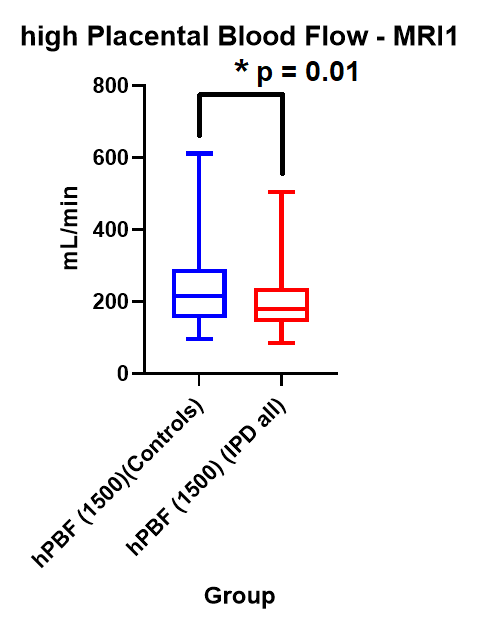 High placental blood flow (hPBF) at first MRI timepoint (14 – 16 weeks GA). Average hPBF for the control group and IPD group is 238.8 mL/min vs 192.2 mL/min, respectively.
High placental blood flow (hPBF) at first MRI timepoint (14 – 16 weeks GA). Average hPBF for the control group and IPD group is 238.8 mL/min vs 192.2 mL/min, respectively.
Objective: Our objective is to test the hypothesis that placental mp-MRI in early pregnancy can aid in the prediction of IPD, impacting maternal and neonatal cardiovascular disease.
Design/Methods: 200 women were recruited in the first trimester of pregnancy. We recorded the pregnancy course through four visits (at 11-14 weeks, 19-22 weeks, 36 weeks, and at delivery), focusing on the development of IPD. Uterine artery Doppler ultrasound was performed at 11-14 and 19-22 weeks of gestation. Placental pCASL mp-MRI was performed at 14-16 and 19-22 weeks of gestation. Imaging software was used to measure maternal to placental blood flow (PBF), regions of high placental blood flow (hPBF), and placental volume.
Results: 179 maternal-infant dyads were analyzed. 44 women developed IPD (24.5%), and 135 women did not develop IPD (75.5%).
At the first MRI timepoint (14-16 weeks), there were 117 controls and 44 IPD cases with MRI scans. There was no difference in placental volume or arterial transit time (ATT) between the groups (p = 0.71 and p = 0.26, respectively). In contrast, PBF was significantly lower in the IPD group than the control group (55.9 mL/min vs 64.2 mL/min respectively, p = 0.043; Figure 1). hPBF was also significantly lower in the IPD group than the control group (192.2 vs. 238.8 mL/min, p = 0.01; Figure 2).
At the second MRI timepoint (19-22 weeks), there were 111 controls and 42 IPD cases with MRI scans. There was no difference in placental volume or ATT between the groups (p = 0.85 and p = 0.39, respectively). In contrast to the first MRI timepoint, there was no significant difference in PBF or hPBF between the groups (p = 0.32 and p = 0.16, respectively).Conclusion(s): pCASL mp-MRI of early-gestation (14-16 weeks) placental blood flow may predict IPD. Our studies potentially have a major impact on maternal and neonatal development of long-term cardiovascular disease.
Supported by NIH U01-HD087221
Brian Lee _ Curriculum Vitae.pdf
Figure 2: high Placental blood flow at first MRI timepoint
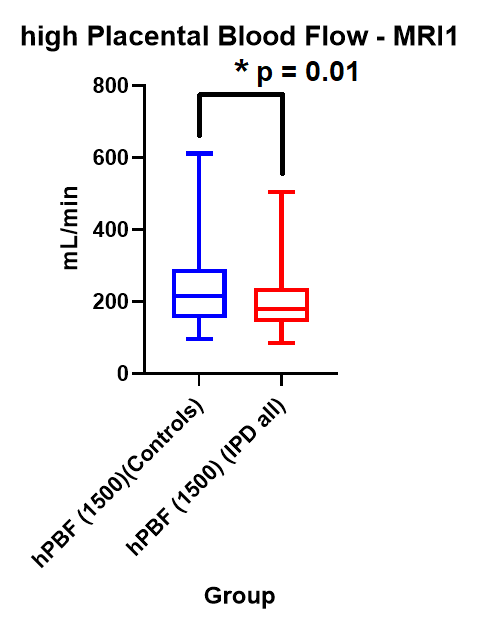 High placental blood flow (hPBF) at first MRI timepoint (14 – 16 weeks GA). Average hPBF for the control group and IPD group is 238.8 mL/min vs 192.2 mL/min, respectively.
High placental blood flow (hPBF) at first MRI timepoint (14 – 16 weeks GA). Average hPBF for the control group and IPD group is 238.8 mL/min vs 192.2 mL/min, respectively.