Back
Public Health & Prevention
Category: Abstract Submission
Public Health & Prevention III
492 - Changes in Collaborative Practice between Nurse Home Visitors and Community Service Providers: A Longitudinal Survey Analysis
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 492
Publication Number: 492.344
Publication Number: 492.344
Venice N. Williams, University of Colorado School of Medicine, Golden, CO, United States; Carol Franco, University of Colorado Anschutz Medical Campus, Johnstown, CO, United States; Connie Lopez, University of Colorado School of Medicine, Thornton, CO, United States; Michael D. Knudtson, University of Colorado School of Medicine, Denver, CO, United States; Mandy Allison, University of Colorado School of Medicine, Denver, CO, United States; Gregory Tung, Colorado School of Public Health, Aurora, CO, United States
Venice N. Williams, PhD, MPH (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Evidence-based home visiting programs improve the health of families experiencing adversities. Collaboration between home visitors and other community service providers such as primary care, mental health, housing, nutrition services, and child welfare is essential to achieve positive outcomes. Collaboration between these providers is based on relationships supported by organizational factors.
Objective: To assess changes in collaborative dynamics between Nurse-Family Partnership (NFP) home visitors and other community providers serving mothers and children across all U.S. NFP implementation sites.
Design/Methods: We conducted an internet survey of nursing supervisors from all NFP implementation sites regarding collaborative practices between home visitors and other community providers in 2018, 2020, and 2021. The survey included the validated 7-item Relational Coordination Scale and adapted items from the Interagency Collaboration Activities Scale on shared resources. Data were analyzed with descriptive statistics; responses over time were matched by team number and compared using paired t-tests.
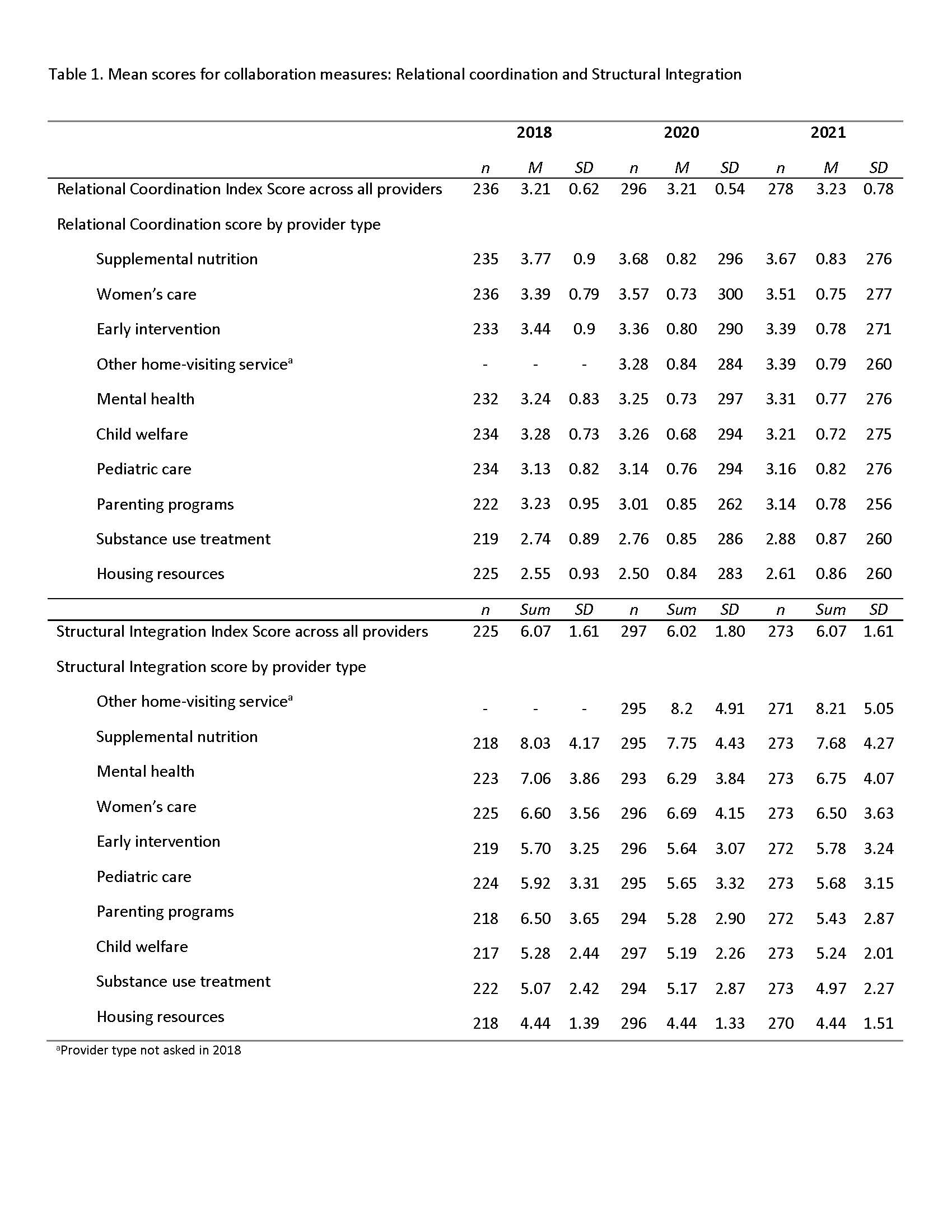
Results: The response rate was 71% (263/370) in 2018, 83% (312/383) in 2020, and 83% (345/414) in 2021. Relational coordination scores, which are relative measures, ranged from 1 to 5; highest with supplemental nutrition services (M = 3.77, 3.68, 3.67 across the three years), lowest with housing (M = 2.55, 2.50, 2.61), and moderate with pediatric care providers (M = 3.13, 3.14, 3.16). The greatest integration of resources was with other home visiting services (sum = 8.20, 8.21 in 2020 and 2021), least with housing (sum = 4.44 across all three years), and moderate with pediatric care (sum = 5.92, 5.65, 5.68); with a range of 1-20 where higher scores indicated greater integration of resources. There were small decreases in coordination with supplemental nutrition from 2018 to 2020 (M = 3.85 vs 3.73; p=0.03), decreases in coordination with parenting programs (M= 3.28 vs. 3.10; p=0.04) and increases in coordination with women’s care providers (M = 3.46 vs. 3.66; p=0.00).Conclusion(s): Home visitors collaborate with community providers with variation in the degree of collaboration across sites and by provider type within a site. Changes in collaboration over time were small, suggesting targeted interventions may be needed to improve coordination and integration of resources between nurse home visitors and other community providers. Collaboration measures used in this study may inform the development and evaluation of future interventions to improve collaboration between community providers.
Table 1. Mean scores for collaboration measures: Relational coordination and Structural Integration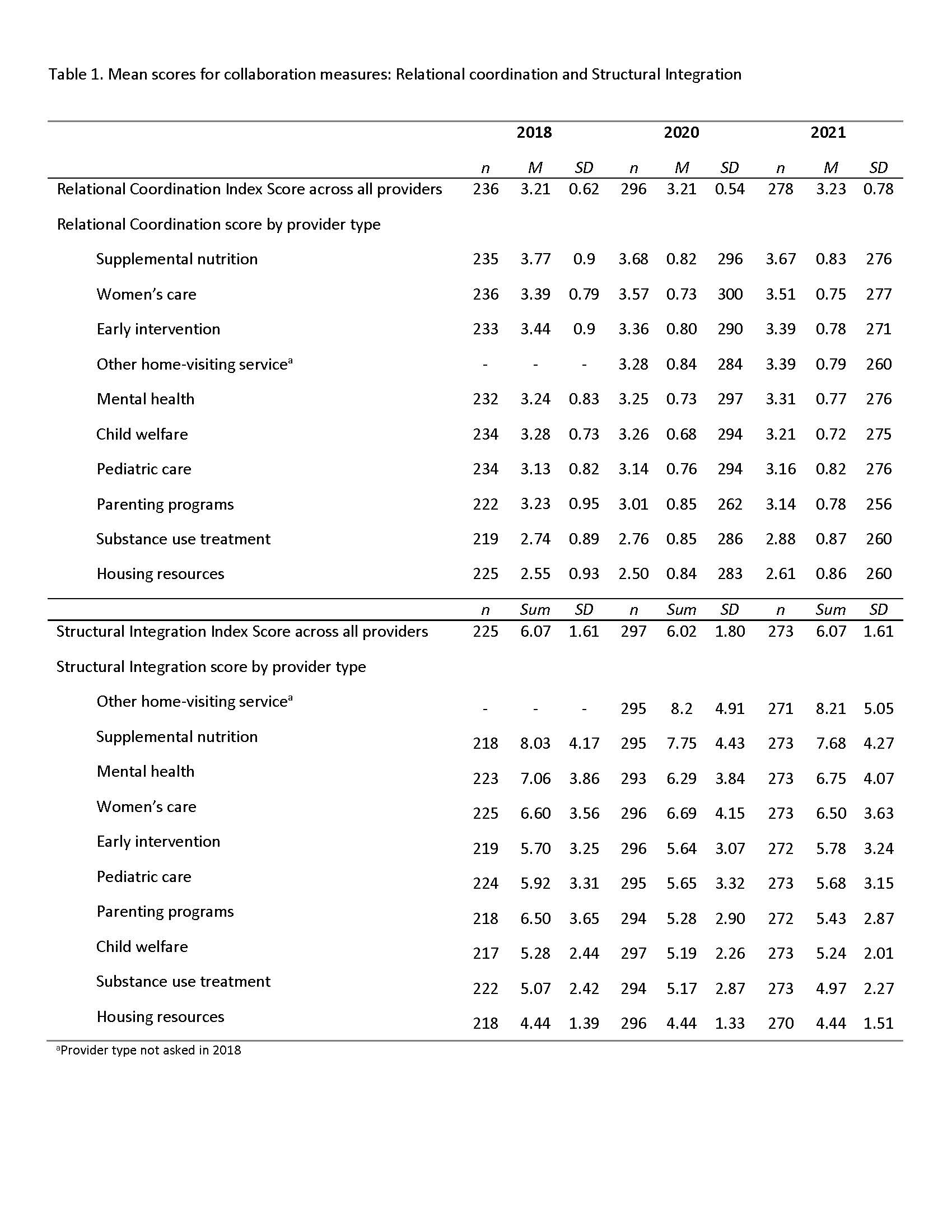
Objective: To assess changes in collaborative dynamics between Nurse-Family Partnership (NFP) home visitors and other community providers serving mothers and children across all U.S. NFP implementation sites.
Design/Methods: We conducted an internet survey of nursing supervisors from all NFP implementation sites regarding collaborative practices between home visitors and other community providers in 2018, 2020, and 2021. The survey included the validated 7-item Relational Coordination Scale and adapted items from the Interagency Collaboration Activities Scale on shared resources. Data were analyzed with descriptive statistics; responses over time were matched by team number and compared using paired t-tests.
Results: The response rate was 71% (263/370) in 2018, 83% (312/383) in 2020, and 83% (345/414) in 2021. Relational coordination scores, which are relative measures, ranged from 1 to 5; highest with supplemental nutrition services (M = 3.77, 3.68, 3.67 across the three years), lowest with housing (M = 2.55, 2.50, 2.61), and moderate with pediatric care providers (M = 3.13, 3.14, 3.16). The greatest integration of resources was with other home visiting services (sum = 8.20, 8.21 in 2020 and 2021), least with housing (sum = 4.44 across all three years), and moderate with pediatric care (sum = 5.92, 5.65, 5.68); with a range of 1-20 where higher scores indicated greater integration of resources. There were small decreases in coordination with supplemental nutrition from 2018 to 2020 (M = 3.85 vs 3.73; p=0.03), decreases in coordination with parenting programs (M= 3.28 vs. 3.10; p=0.04) and increases in coordination with women’s care providers (M = 3.46 vs. 3.66; p=0.00).Conclusion(s): Home visitors collaborate with community providers with variation in the degree of collaboration across sites and by provider type within a site. Changes in collaboration over time were small, suggesting targeted interventions may be needed to improve coordination and integration of resources between nurse home visitors and other community providers. Collaboration measures used in this study may inform the development and evaluation of future interventions to improve collaboration between community providers.
Table 1. Mean scores for collaboration measures: Relational coordination and Structural Integration