Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: Potpourri
558 - Effect of early skin-to-skin contact on skin colonization in preterm infants: A pre- and post-implementation study
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 558
Poorva Deshpande, Mount Sinai Hospital, Mississauga, ON, Canada; Nosheen Akhtar, Mount Sinai Hospital, Toronto.Canada, Toronto, ON, Canada; Maura Helena Ferrari Resende, Sunnybrook Health Sciences Centre, Toronto, ON, Canada; Allison McGeer, University of Toronto Temerty Faculty of Medicine, Toronto, ON, Canada; Vibhuti S. Shah, Mount Sinai Hospital, MIssissauga, ON, Canada

Poorva Deshpande, MBBS, MRCPCP, MSc (she/her/hers)
Neonatologist
Mount Sinai Hospital
Toronto, Ontario, Canada
Presenting Author(s)
Background: Maternal skin-to-skin contact (MSSC) in neonates has been shown to reduce nosocomial infections. In preterm infants, early exposure to maternal community-acquired skin commensals may prevent skin colonization by hospital-acquired pathogens. However, the impact of early MSSC on skin colonization in preterm infants is unknown.
Objective: To compare the skin colonization pattern on days 2, 3 and 7 of life of preterm infants born at gestational age (GA) 28+0 – 31+6 weeks who received MSSC within 24 hours (h) from birth to those who did not.
Design/Methods: This pre- and post -implementation study was conducted in Level III NICU, Mount Sinai Hospital, Toronto. In our unit, early MSSC for stable preterm infants within first 24 h of life was implemented in April 2013. Infants born between GA 280 to 316 weeks before and after implementation were recruired. Exclusion criteria were rupture of membranes > 18 h, maternal chorioamnionitis, clinical instability (receiving mechanical ventilation, > 50% of supplemental oxygen on non-invasive ventilation, inotropes) and congenital or genetic abnormalities. Infants in the post-implementation group received MSSC within the first 24 h for a minimum duration of 30 minutes. For both groups, pooled skin swabs were obtained between 24- 36 h, 48 - 72 h and on day 7 of life from the groin, axilla and umbilicus. Pooled mouth and rectal swabs were obtained from infants on day 7 for Staphylococcus aureus (S. aureus) colonization. Maternal pooled nasal-rectal swabs were obtained during 7 days of birth for both groups. Organisms were categorized as pathogens or commensals as per Table 2. The primary outcome was rate of skin colonization with bacterial pathogens on days 2, 3 and 7 of life. The secondary outcome was rate of S. aureus colonization.
Results: Twenty-seven and 17 infants were included in the pre- and post-implementation group, respectively. Baseline characteristics are shown in Table 1. The duration of MSSC was statistically significantly higher in the first week of life in infants in the post-implementation group (p = 0.03). Colonization with pathogens vs. commensals or S. aureus did not differ between groups at any time points (Table 2). The skin was fully colonized in both groups by day 7.Conclusion(s): No differences were observed in skin or S. aureus colonization pattern in the first week of life in clinically stable preterm infants with early MSSC in first 24 hours. Studies with a larger sample and longitudinal microbiological data are required to evaluate the impact of MSSC on skin colonization.
Table 1: Baseline characteristics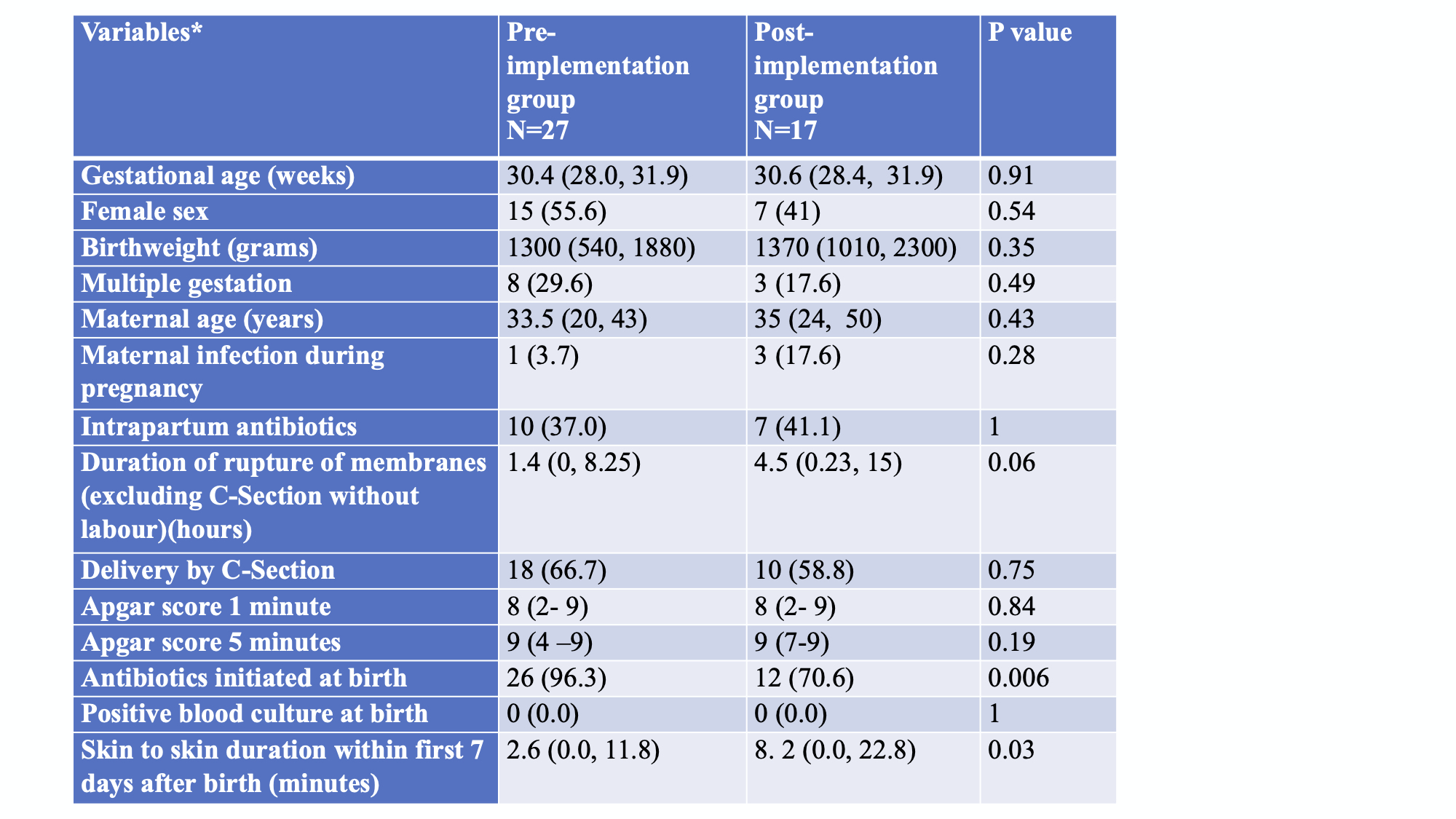 *Data are presented as median (range) or N (%) as appropriate
*Data are presented as median (range) or N (%) as appropriate
Table 2: Categorization of organisms.png)
Objective: To compare the skin colonization pattern on days 2, 3 and 7 of life of preterm infants born at gestational age (GA) 28+0 – 31+6 weeks who received MSSC within 24 hours (h) from birth to those who did not.
Design/Methods: This pre- and post -implementation study was conducted in Level III NICU, Mount Sinai Hospital, Toronto. In our unit, early MSSC for stable preterm infants within first 24 h of life was implemented in April 2013. Infants born between GA 280 to 316 weeks before and after implementation were recruired. Exclusion criteria were rupture of membranes > 18 h, maternal chorioamnionitis, clinical instability (receiving mechanical ventilation, > 50% of supplemental oxygen on non-invasive ventilation, inotropes) and congenital or genetic abnormalities. Infants in the post-implementation group received MSSC within the first 24 h for a minimum duration of 30 minutes. For both groups, pooled skin swabs were obtained between 24- 36 h, 48 - 72 h and on day 7 of life from the groin, axilla and umbilicus. Pooled mouth and rectal swabs were obtained from infants on day 7 for Staphylococcus aureus (S. aureus) colonization. Maternal pooled nasal-rectal swabs were obtained during 7 days of birth for both groups. Organisms were categorized as pathogens or commensals as per Table 2. The primary outcome was rate of skin colonization with bacterial pathogens on days 2, 3 and 7 of life. The secondary outcome was rate of S. aureus colonization.
Results: Twenty-seven and 17 infants were included in the pre- and post-implementation group, respectively. Baseline characteristics are shown in Table 1. The duration of MSSC was statistically significantly higher in the first week of life in infants in the post-implementation group (p = 0.03). Colonization with pathogens vs. commensals or S. aureus did not differ between groups at any time points (Table 2). The skin was fully colonized in both groups by day 7.Conclusion(s): No differences were observed in skin or S. aureus colonization pattern in the first week of life in clinically stable preterm infants with early MSSC in first 24 hours. Studies with a larger sample and longitudinal microbiological data are required to evaluate the impact of MSSC on skin colonization.
Table 1: Baseline characteristics
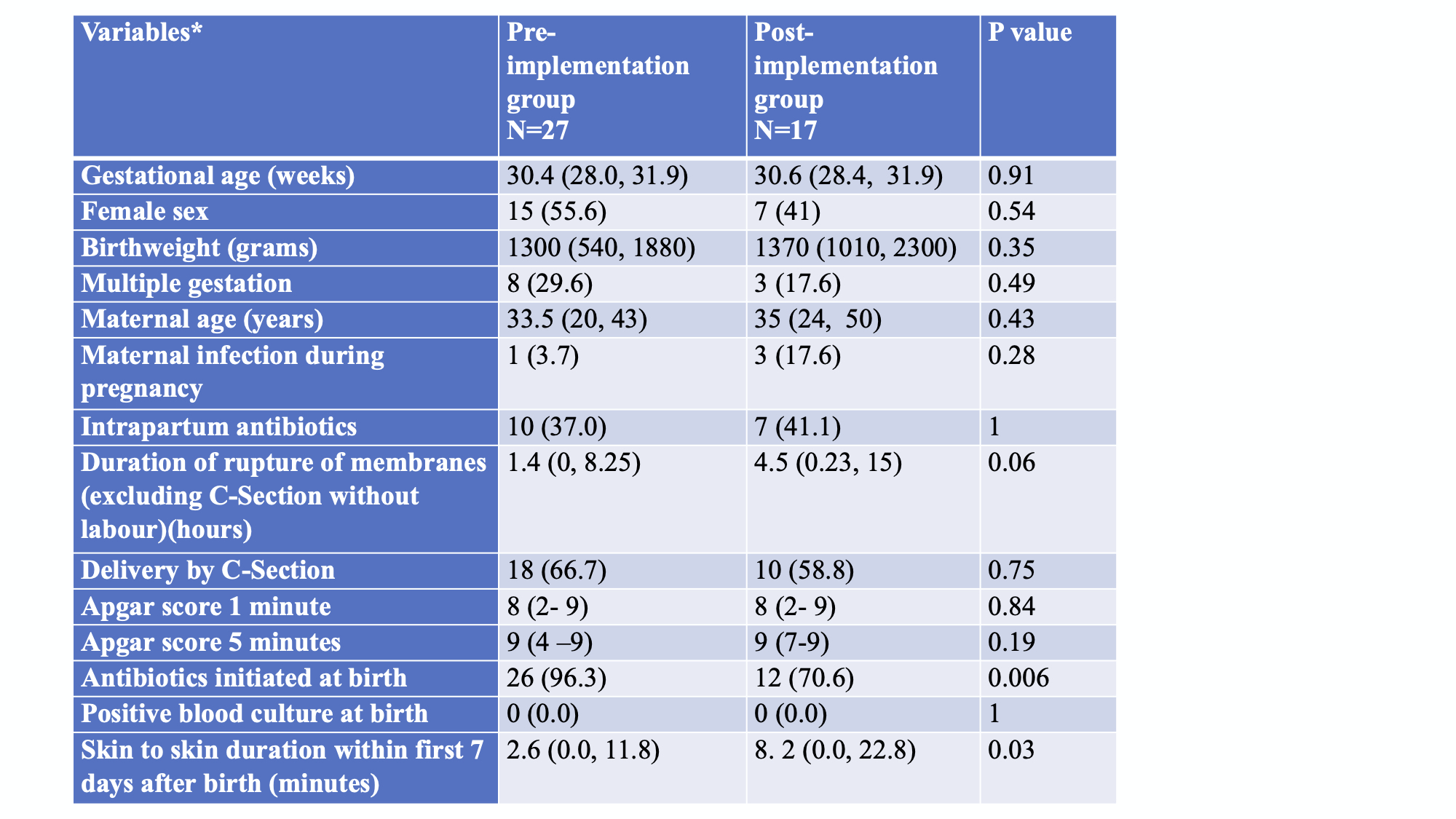 *Data are presented as median (range) or N (%) as appropriate
*Data are presented as median (range) or N (%) as appropriateTable 2: Categorization of organisms
.png)
