Asthma
Category: Abstract Submission
Asthma
38 - Effectiveness Of Objective Verification Of Inhaler Technique In Pediatric Asthma Patients Aged 4 to 18
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 38
Publication Number: 38.300
Publication Number: 38.300
Ninabahen Dave, University of Mississippi School of Medicine, jackson, MS, United States; Robert A. Greer, University of South Alabama Children's and Women's Hospital, Mobile, AL, United States; Jagdish Desai, University of Mississippi School of Medicine, Jackson, MS, United States; Taylor Mabry, UMMC, Brandon, MS, United States

Ninabahen Dave, MD
Associate Professor of Pediatrics
University of Mississippi School of Medicine
jackson, Mississippi, United States
Presenting Author(s)
Background: Asthma is a common respiratory disease characterized by airway hyperresponsiveness and reversible airflow obstruction for which the mainstay of treatment is inhaled medicines directly into the lungs. Treatment involves both the patient's willingness to use the medication as well as their ability to use the proper technique of the specific inhaler device required for administration. Improper inhaler technique can lead to decreased delivery of medication to its target in the bronchial tree resulting in inadequately controlled asthma as well as increased side effects from asthma medications. Per 2018 GINA guidelines, all asthmatic patients should have their inhaler technique reviewed every visit and validate their ability to use the device; however, the methodology is not specified.
The ACT has been designated as a core measure for research of asthma by the NIH. Difference of 3 points in ACT score suggests change in asthma control.
Objective: To find an appreciable difference in asthma control of patients taught inhaler technique subjectively compared to patients with objective verification using Aerosol Inhalation Monitor (AIM) Vitalograph.
Design/Methods: A retrospective chart review of patients with a current diagnosis of asthma was performed before and after the implementation of AIM Vitalograph between July 2015 to September 2017. Before September 2016, all patients were taught the inhaler technique subjectively. Asthma control was assessed using the standardized Asthma Control Test (ACT) for the corresponding age groups as a standard of care. ACT scores of each eligible patient were collected at the initial visit (baseline visit) and two more visits after that within 12 months of follow-up. Mean differences from baseline visit to the first (∆ACT1) and second follow-up visit (∆ACT2) were compared between two groups.
Results: A total of 31 and 35 eligible patient’s charts were reviewed for objective and subjective verification groups, respectively. No significant difference was observed in baseline characteristics. The median ACT score improvement (∆ACT1) for objective verification was 2.5 and 0.0 for the subjective verification group with a statistically trending p-value of 0.08. The median ACT score improvement (∆ACT2) for objective verification was 3.5, and 0.0 for the subjective verification group with a statistically significant p-value of 0.02.Conclusion(s): Our results provide proof of concept that objective verification of inhaler technique in asthmatics may help to improve control as indicated by the ACT score. Prospective studies with adequate power are required to confirm these findings.
ACT Score Improvement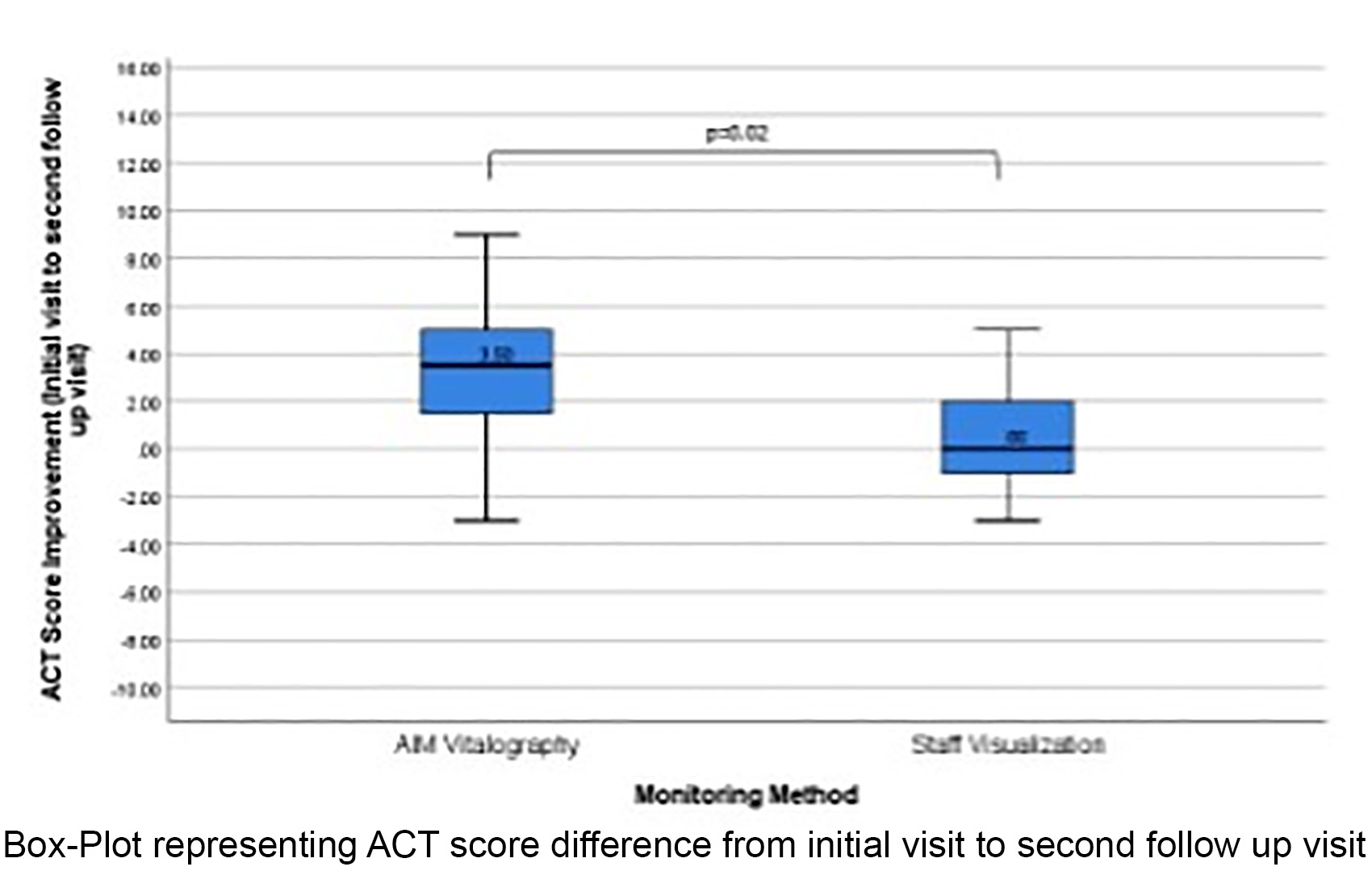 ACT Score Improvement in Objective Verification group from Initial visit to second follow up visit compare to Subjective Verification group.
ACT Score Improvement in Objective Verification group from Initial visit to second follow up visit compare to Subjective Verification group.
The ACT has been designated as a core measure for research of asthma by the NIH. Difference of 3 points in ACT score suggests change in asthma control.
Objective: To find an appreciable difference in asthma control of patients taught inhaler technique subjectively compared to patients with objective verification using Aerosol Inhalation Monitor (AIM) Vitalograph.
Design/Methods: A retrospective chart review of patients with a current diagnosis of asthma was performed before and after the implementation of AIM Vitalograph between July 2015 to September 2017. Before September 2016, all patients were taught the inhaler technique subjectively. Asthma control was assessed using the standardized Asthma Control Test (ACT) for the corresponding age groups as a standard of care. ACT scores of each eligible patient were collected at the initial visit (baseline visit) and two more visits after that within 12 months of follow-up. Mean differences from baseline visit to the first (∆ACT1) and second follow-up visit (∆ACT2) were compared between two groups.
Results: A total of 31 and 35 eligible patient’s charts were reviewed for objective and subjective verification groups, respectively. No significant difference was observed in baseline characteristics. The median ACT score improvement (∆ACT1) for objective verification was 2.5 and 0.0 for the subjective verification group with a statistically trending p-value of 0.08. The median ACT score improvement (∆ACT2) for objective verification was 3.5, and 0.0 for the subjective verification group with a statistically significant p-value of 0.02.Conclusion(s): Our results provide proof of concept that objective verification of inhaler technique in asthmatics may help to improve control as indicated by the ACT score. Prospective studies with adequate power are required to confirm these findings.
ACT Score Improvement
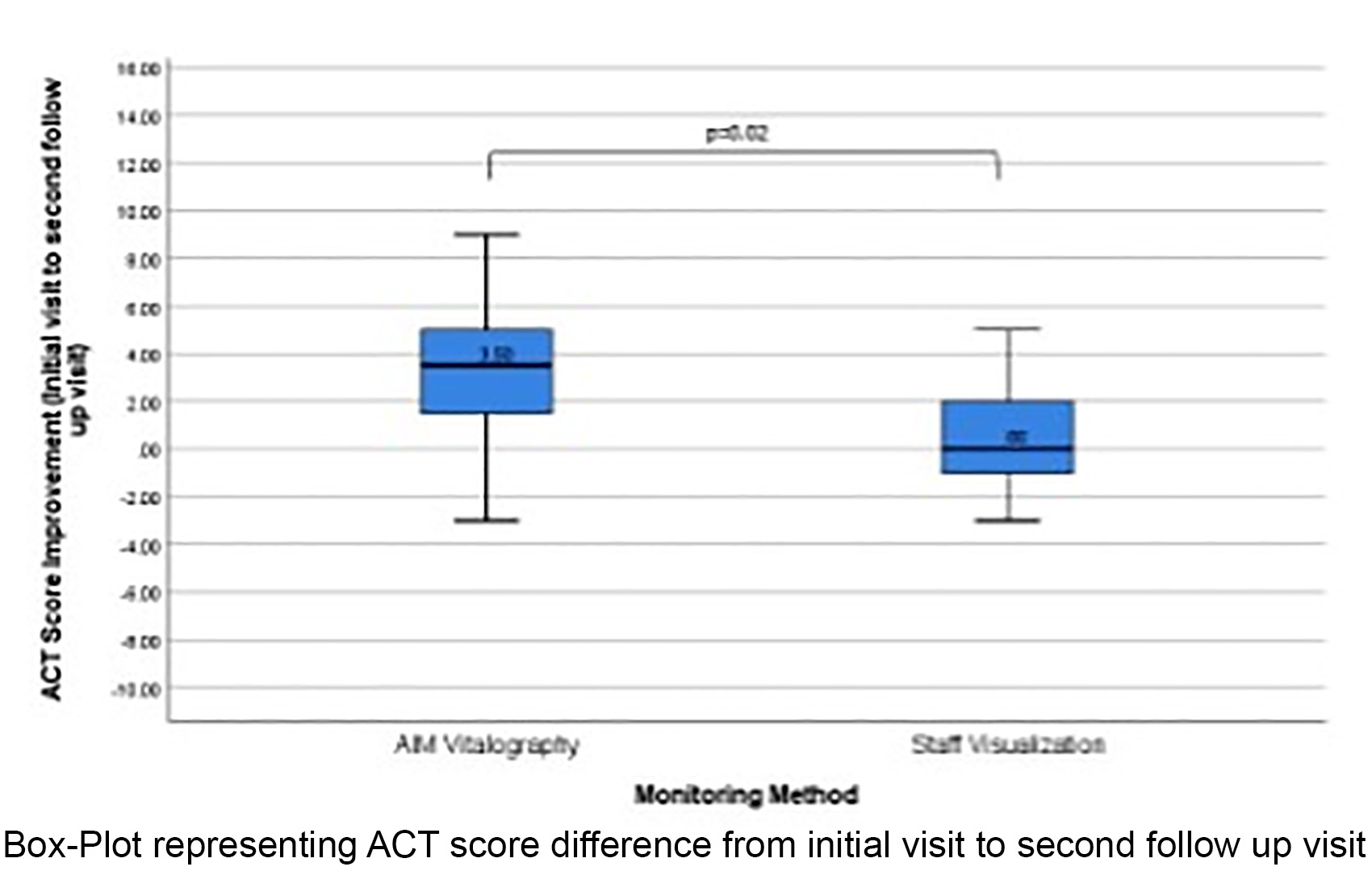 ACT Score Improvement in Objective Verification group from Initial visit to second follow up visit compare to Subjective Verification group.
ACT Score Improvement in Objective Verification group from Initial visit to second follow up visit compare to Subjective Verification group.