Back
Critical Care
Category: Abstract Submission
Critical Care III
110 - Efficacy of an Early Mobilization Protocol in a Pediatric ICU
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 110
Publication Number: 110.307
Publication Number: 110.307
Roman Gusdorf, Vanderbilt University School of Medicine, Nashville, TN, United States; Shilin Zhao, Vanderbilt University School of Medicine, Nashville, TN, United States; Stacey R. Williams, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Katherine Hedden, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Camille Heider, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Jennifer Pearson, Monroe Carell Jr Children's hospital at Vanderbilt, Nashville, TN, United States; Kristina A. Betters, Vanderbilt Univeristy, Nashville, TN, United States
Roman Gusdorf, BS
Medical Student
Vanderbilt University School of Medicine
Nashville, Tennessee, United States
Presenting Author(s)
Background: Early mobility (EM) is recommended for intensive care unit (ICU) patients to ameliorate the negative consequences of an ICU stay. Pediatric ICUs (PICUs) have been slow to adopt EM programs given several barriers, and as such many patients may have missed treatment opportunities.
Objective: We sought to evaluate the efficacy of a PICU EM protocol and examine the rehabilitation needs encountered in a heterogenous PICU population.
Design/Methods: This is a single-center, retrospective cohort study of PICU patients treated in an academic free-standing children’s hospital. In May 2018, a physical therapy (PT) and occupational therapy (OT) driven EM protocol, for all patients with an ICU length of stay of 72 hours or more, was implemented in both a 24-bed medical-surgical ICU and 18-bed cardiac ICU. Demographic data and rehabilitation evaluations, treatments, and outcomes were retrospectively collected on PICU patients who had a length of stay at least 72 hours prior to the protocol (November 2017 – April 2018) and after the protocol was implemented (June 2018 – April 2019). Descriptive statistics were reported with median and interquartile range. Wilcox rank sum and chi-squared tests were used to compare continuous and categorical data between two groups. A p-value of less than 0.05 was predefined as significant.
Results: Age, sex, mechanical ventilation requirement, exposure to sedative infusions, incidence of delirium, and disposition did not differ between the pre and post-EM groups. Ninety-four percent of patients in the post-EM cohort were evaluated by PT and OT, while only 51% were evaluated in the pre-EM cohort (p < 0.001). The median and interquartile ranges (IQR) of number of PT/OT sessions during ICU stay increased from 3.50 (2.0, 7.0) in the pre-protocol group to 4.0 (2.0, 9.0) in the post-protocol group (p=0.043).Conclusion(s): Implementation of an EM protocol resulted in a significant increase in the number of patients evaluated and treated by PT/OT during their ICU stay. Additionally, the number of PT/OT sessions in the PICU increased after implementation of the protocol. A formal EM protocol may be useful in increasing the amount of PICU patients evaluated and treated by PT and OT in a timely manner.
Cohorts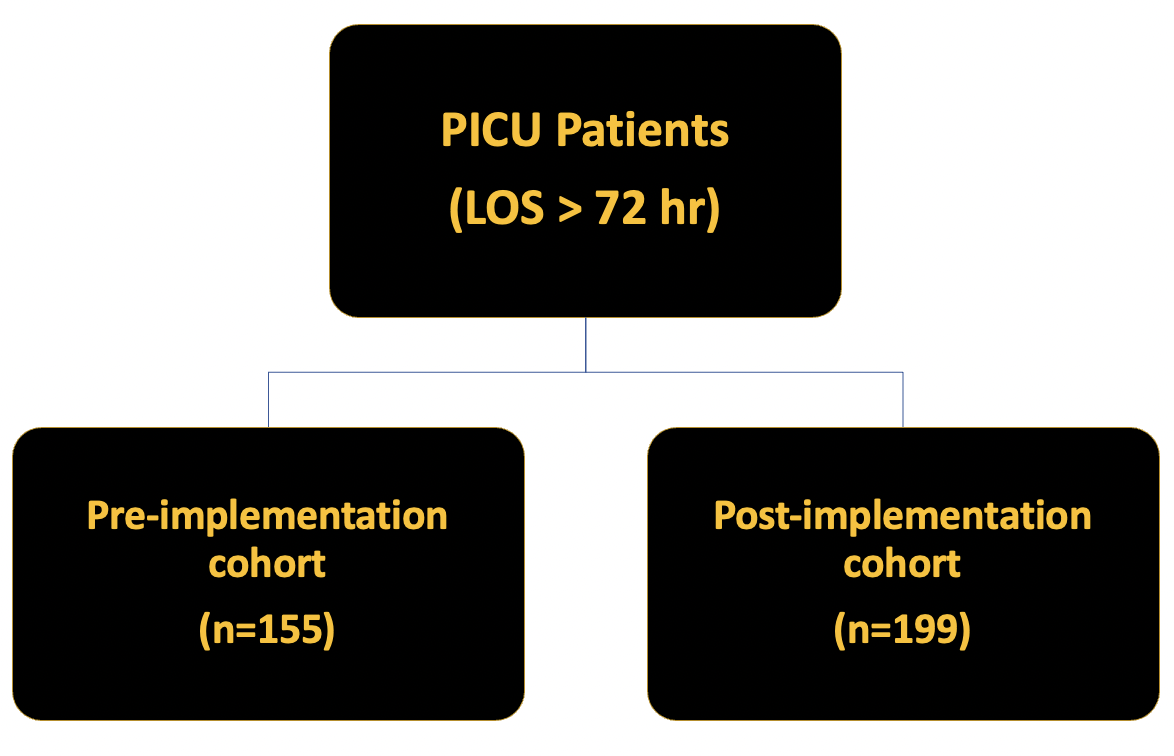 Demographics of patients in each cohort
Demographics of patients in each cohort
Demographics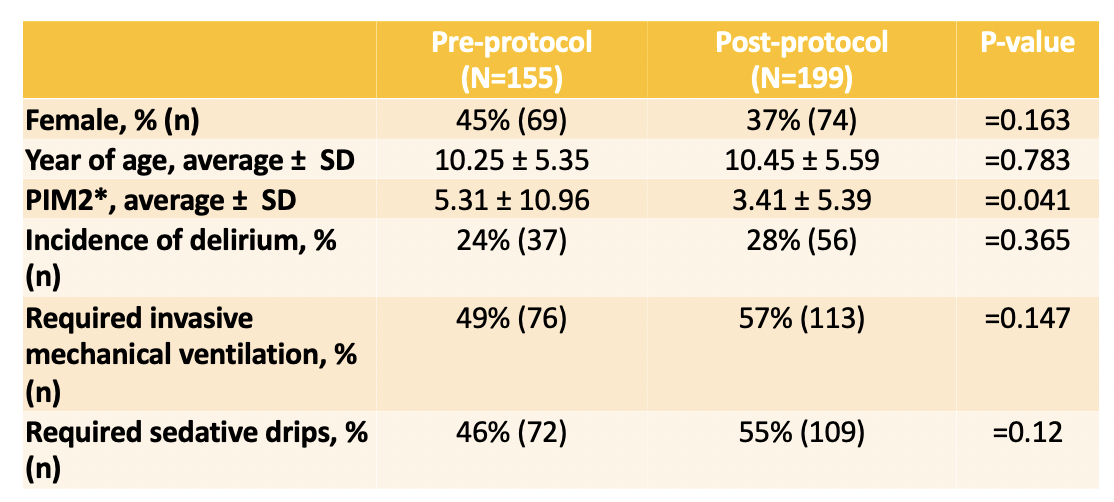 Demographic and clinical factors of patients in each cohort
Demographic and clinical factors of patients in each cohort
Objective: We sought to evaluate the efficacy of a PICU EM protocol and examine the rehabilitation needs encountered in a heterogenous PICU population.
Design/Methods: This is a single-center, retrospective cohort study of PICU patients treated in an academic free-standing children’s hospital. In May 2018, a physical therapy (PT) and occupational therapy (OT) driven EM protocol, for all patients with an ICU length of stay of 72 hours or more, was implemented in both a 24-bed medical-surgical ICU and 18-bed cardiac ICU. Demographic data and rehabilitation evaluations, treatments, and outcomes were retrospectively collected on PICU patients who had a length of stay at least 72 hours prior to the protocol (November 2017 – April 2018) and after the protocol was implemented (June 2018 – April 2019). Descriptive statistics were reported with median and interquartile range. Wilcox rank sum and chi-squared tests were used to compare continuous and categorical data between two groups. A p-value of less than 0.05 was predefined as significant.
Results: Age, sex, mechanical ventilation requirement, exposure to sedative infusions, incidence of delirium, and disposition did not differ between the pre and post-EM groups. Ninety-four percent of patients in the post-EM cohort were evaluated by PT and OT, while only 51% were evaluated in the pre-EM cohort (p < 0.001). The median and interquartile ranges (IQR) of number of PT/OT sessions during ICU stay increased from 3.50 (2.0, 7.0) in the pre-protocol group to 4.0 (2.0, 9.0) in the post-protocol group (p=0.043).Conclusion(s): Implementation of an EM protocol resulted in a significant increase in the number of patients evaluated and treated by PT/OT during their ICU stay. Additionally, the number of PT/OT sessions in the PICU increased after implementation of the protocol. A formal EM protocol may be useful in increasing the amount of PICU patients evaluated and treated by PT and OT in a timely manner.
Cohorts
 Demographics of patients in each cohort
Demographics of patients in each cohortDemographics
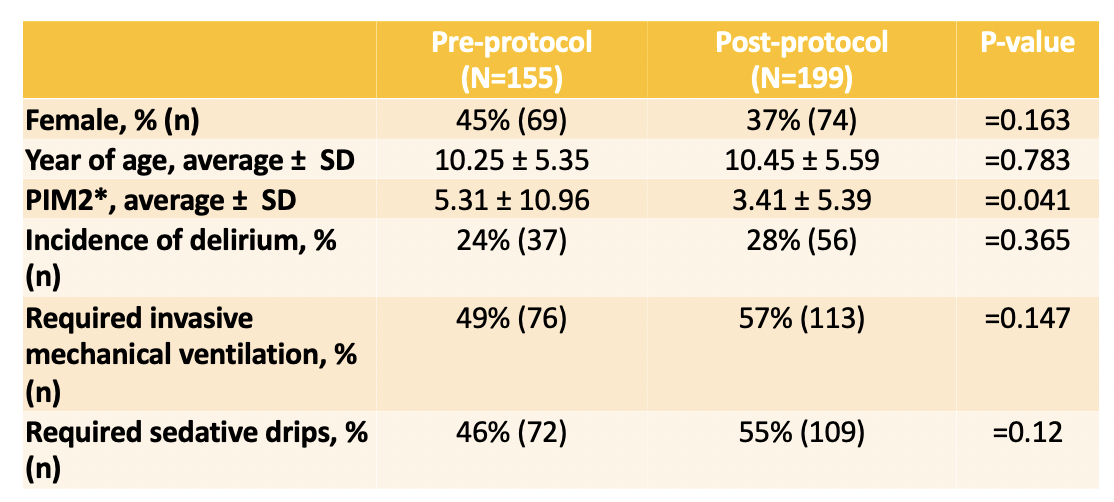 Demographic and clinical factors of patients in each cohort
Demographic and clinical factors of patients in each cohort