Health Services Research
Category: Abstract Submission
Health Services Research I
194 - Hispanic Children Face Larger Disparities in Medicaid Patient Experience than Hispanic Adults
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 194
Sara Toomey, Boston Children's Hospital, Boston, MA, United States; Marc Elliott, RAND Corporation, Santa Monica, CA, United States; Alan M. Zaslavsky, Harvard Medical School, Milton, MA, United States; Shanshan Liu, Boston Children's Hospital, Boston, MA, United States; Sarah Y. Lee, State University of New York Downstate Medical Center College of Medicine, Palisades Park, NJ, United States; Asher K. Baden, Boston Children's Hospital, Boston, MA, United States; Sara W. Buscher, Boston Children's Hospital, Boston, MA, United States; Mark Schuster, Kaiser Permanente Bernard J. Tyson School of Medicine, Pasadena, CA, United States

Sara Toomey, MD, MPhil, MPH, MSc (she/her/hers)
Chief Safety and Quality Officer, SVP
Boston Children's Hospital
Cambridge, Massachusetts, United States
Presenting Author(s)
Background: Racial/ethnic and socioeconomic disparities in patient experience may be associated with disparities in other health outcomes. Hispanic patients typically report worse experiences than do other patients, but it is unclear whether these differences occur for pediatric as well as adult patients and how much the size of these differences varies across health plans.
Objective: To compare racial/ethnic patterns in patient experience for adult care and pediatric care as reported by adult caregivers.
Design/Methods: We analyzed data from the Consumer Assessment of Healthcare Providers and Systems Health Plan Survey from the AHRQ CAHPS database representing all U.S. census regions and divisions from 2015 to 2018. Using cross-sectional data from 495 Medicaid health plans, we compared pediatric and adult care by race/ethnicity, case-mix adjusting for sex, age, overall health, and education. We analyzed two series of linear regression models. The first measures total disparities by comparing each racial/ethnic group to the rest of the population. The second adds plan identifiers as fixed effects to assess within-plan disparities. Between-plan differences are then calculated by subtracting within-plan disparities from total disparities.
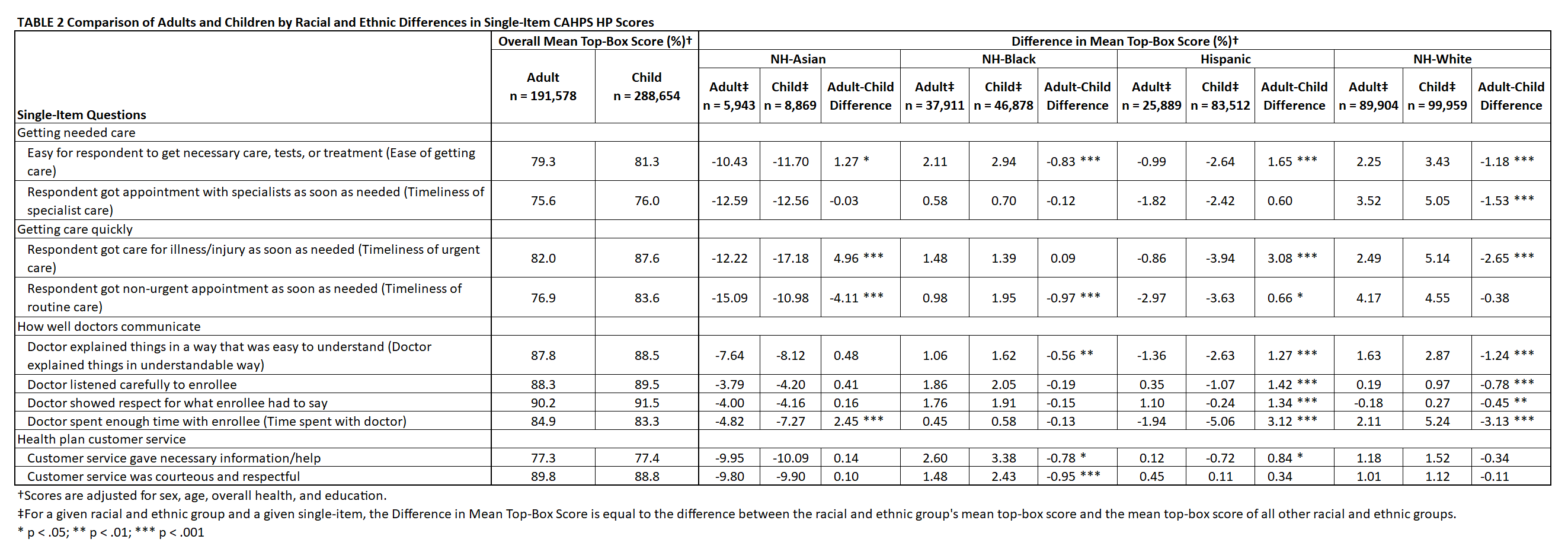
Results: 480,232 completed surveys (191,578 adults, 288,654 children) were included (Table 1). Both Hispanic children (29% of child Medicaid respondents) and adults (14% of all Medicaid respondents) had worse experiences (0-100 scale with differences of 5, 3, 1 considered “large,” “medium,” “small”) than non-Hispanic counterparts for ease of getting care (-2.6 for children vs. -1.0 for adults), timeliness of specialist care (-2.4 vs. -1.8), timeliness of urgent care (-3.9 vs. -0.9), timeliness of routine care (-3.6 vs. -3.0), doctor explained things in understandable way (-2.6 vs -1.4), and time spent with doctor (-5.1 vs. -1.9; Table 2). For all four provider-communication items, racial and ethnic differences were greater for Hispanic children than for adults (p < 0.001). For both children and adults, disparities for Hispanic patients reflected within-plan more than between-plan disparities (Table 3).Conclusion(s): Mean patient experience scores of plans with many Hispanic enrollees do not differ substantially from mean scores of plans with little Hispanic enrollment. However, Hispanic adults and especially Hispanic children have worse experiences with care than other enrollees within those plans. Efforts, including assessment of culturally and linguistically appropriate services, are needed to address inequities in pediatric care within Medicaid plans.
Table 1 CAHPS HP 2015-2018: Sample Characteristics by Race and Ethnicity for Adults and Children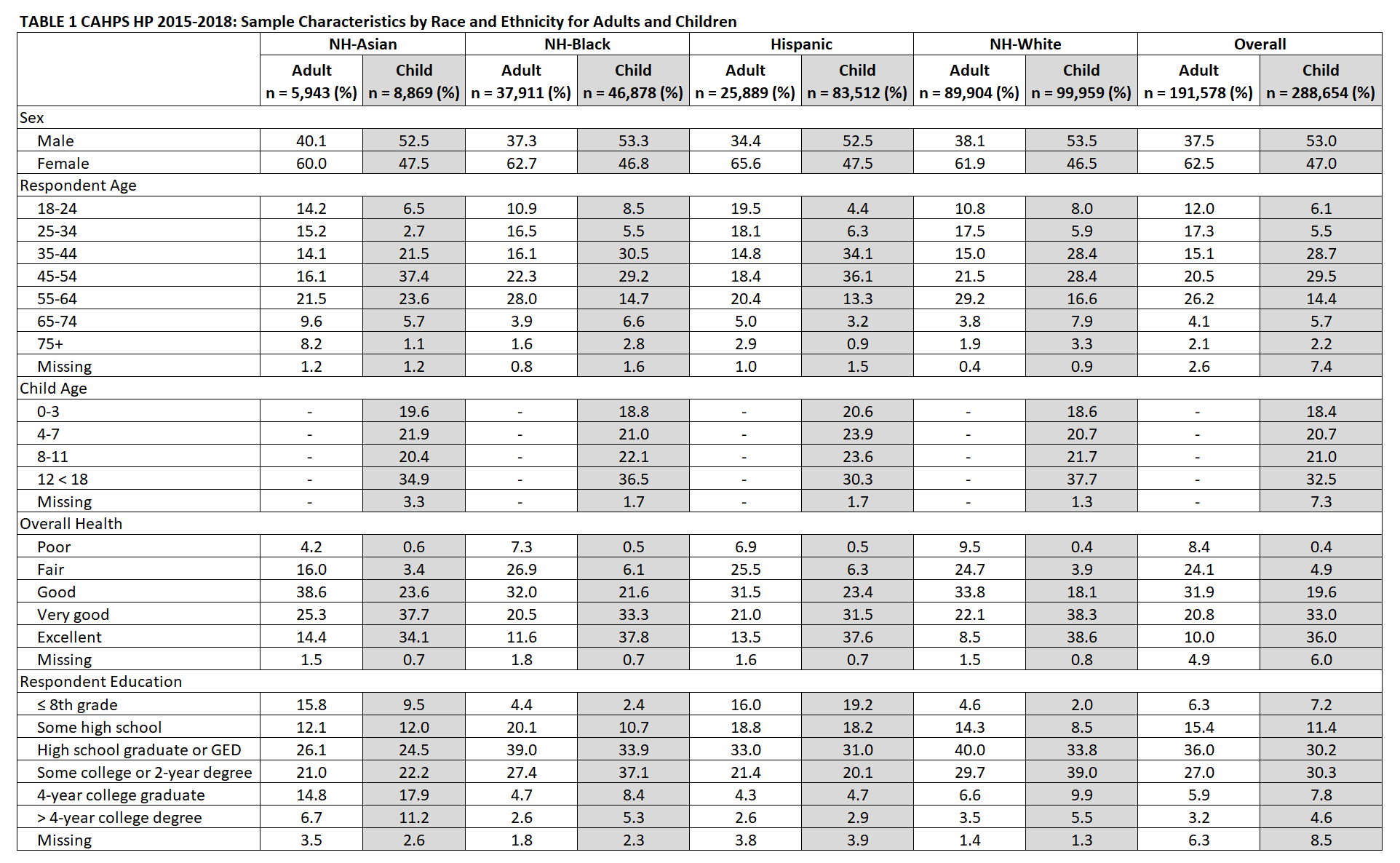
Table 2 Comparison of Adults and Children by Racial and Ethnic Differences in Single-Item CAHPS HP Scores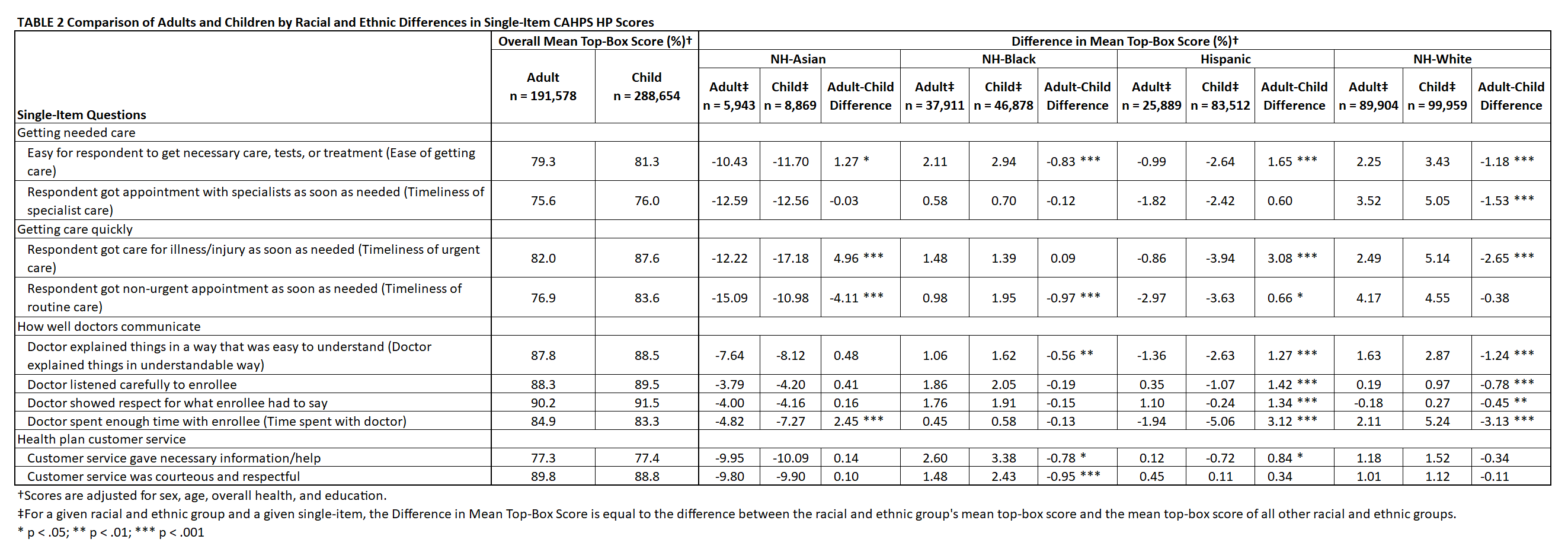
Objective: To compare racial/ethnic patterns in patient experience for adult care and pediatric care as reported by adult caregivers.
Design/Methods: We analyzed data from the Consumer Assessment of Healthcare Providers and Systems Health Plan Survey from the AHRQ CAHPS database representing all U.S. census regions and divisions from 2015 to 2018. Using cross-sectional data from 495 Medicaid health plans, we compared pediatric and adult care by race/ethnicity, case-mix adjusting for sex, age, overall health, and education. We analyzed two series of linear regression models. The first measures total disparities by comparing each racial/ethnic group to the rest of the population. The second adds plan identifiers as fixed effects to assess within-plan disparities. Between-plan differences are then calculated by subtracting within-plan disparities from total disparities.
Results: 480,232 completed surveys (191,578 adults, 288,654 children) were included (Table 1). Both Hispanic children (29% of child Medicaid respondents) and adults (14% of all Medicaid respondents) had worse experiences (0-100 scale with differences of 5, 3, 1 considered “large,” “medium,” “small”) than non-Hispanic counterparts for ease of getting care (-2.6 for children vs. -1.0 for adults), timeliness of specialist care (-2.4 vs. -1.8), timeliness of urgent care (-3.9 vs. -0.9), timeliness of routine care (-3.6 vs. -3.0), doctor explained things in understandable way (-2.6 vs -1.4), and time spent with doctor (-5.1 vs. -1.9; Table 2). For all four provider-communication items, racial and ethnic differences were greater for Hispanic children than for adults (p < 0.001). For both children and adults, disparities for Hispanic patients reflected within-plan more than between-plan disparities (Table 3).Conclusion(s): Mean patient experience scores of plans with many Hispanic enrollees do not differ substantially from mean scores of plans with little Hispanic enrollment. However, Hispanic adults and especially Hispanic children have worse experiences with care than other enrollees within those plans. Efforts, including assessment of culturally and linguistically appropriate services, are needed to address inequities in pediatric care within Medicaid plans.
Table 1 CAHPS HP 2015-2018: Sample Characteristics by Race and Ethnicity for Adults and Children
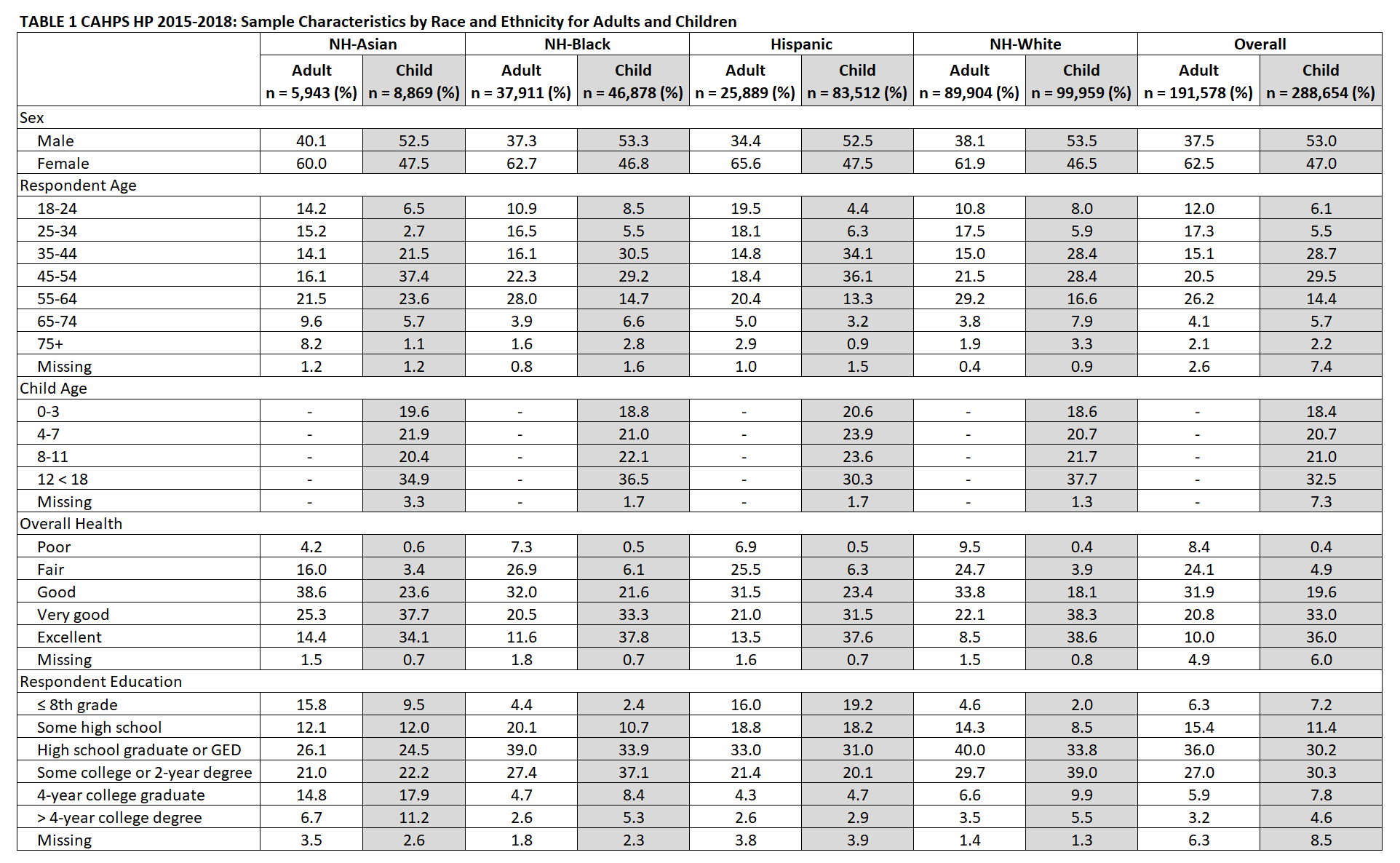
Table 2 Comparison of Adults and Children by Racial and Ethnic Differences in Single-Item CAHPS HP Scores