Hypertension
Category: Abstract Submission
Hypertension I
83 - Hypertension Subspecialty Provider Accuracy in Diagnosing Obesity in Youth Referred for Hypertensive Disorders: a SUPERHERO Interim Analysis
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 83
Publication Number: 83.324
Publication Number: 83.324
Andrew M. South, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston Salem, NC, United States; Victoria Giammattei, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Caroline B. Lucas, Wake Forest School of Medicine of Wake Forest Baptist Medical Center, Winston-Salem, NC, United States; Jack Weaver, Levine Children's Hospital, Charlotte, NC, United States

Andrew Michael South, MD, MS (he/him/his)
Associate Professor
Wake Forest School of Medicine of Wake Forest Baptist Medical Center
Winston Salem, North Carolina, United States
Presenting Author(s)
Background: Obesity is a well-known risk factor for youth-onset hypertension, but the degree to which hypertension subspecialty providers diagnose obesity accurately is unclear.
Objective: Determine whether providers accurately diagnose obesity by ICD-10 code documentation compared to body mass index (BMI)-based obesity classification at the initial clinic visit.
Design/Methods: Interim analysis of Phase 1.1 baseline data from The Study of the Epidemiology of Pediatric Hypertension (SUPERHERO) Registry, a multicenter retrospective cohort of youth referred to subspecialty care for hypertensive disorders. Data were available from two centers and were collected via electronic health record queries using a common data model. Inclusion criteria were initial visit to a subspecialty clinic for ICD-10 code-identified hypertensive disorders from 1/1/2016 to 6/30/2021 and age < 19 years. Exclusion criteria were kidney failure on dialysis, kidney transplantation, or pregnancy by ICD-10 code and, for this analysis, missing BMI values and age < 2 years. We examined obesity prevalence across the study period with Cochran-Armitage trend test. We compared obesity by ICD-10 code-based provider diagnosis (ICD-obesity) with presence of actual obesity (BMI-obesity) defined as BMI ≥95th %ile for age/sex per CDC criteria. We calculated McNemar’s test for agreement, kappa coefficients, sensitivity, specificity, and positive and negative predictive values.
Results: Of 2447 participants, median age was 14.4 years [IQR 11.5, 16.4], 37% were female, 29% were Black or African American, 49% were White or Caucasian, and 18% were Hispanic or Latino. Across the study period, BMI-obesity and ICD-obesity prevalence increased over time from 56 to 66% and 35 to 42%, respectively (p=0.009; Figure 1). ICD-obesity had moderate agreement with BMI-obesity overall and per year, with a missed obesity diagnosis occurring in 20–25% (all McNemar’s test p< 0.001, kappa 0.55–0.6); there was no trend over time (p=0.8). Overall, ICD-obesity had 98% specificity and positive predictive value to predict BMI-obesity, but only 63% sensitivity and 65% negative predictive value (Table 1).Conclusion(s): In a large multicenter cohort of youth referred for hypertensive disorders, obesity increased in prevalence over time but was frequently undiagnosed. Ongoing analyses are investigating why we observed these patterns and the consequences of missed diagnoses, including estimating rates of referrals to Nutrition and Metabolic Clinics.
Figure 1: Agreement between Provider Obesity Diagnosis by ICD-10 Code and BMI-Based Obesity Prevalence by Year of Initial Clinic Visit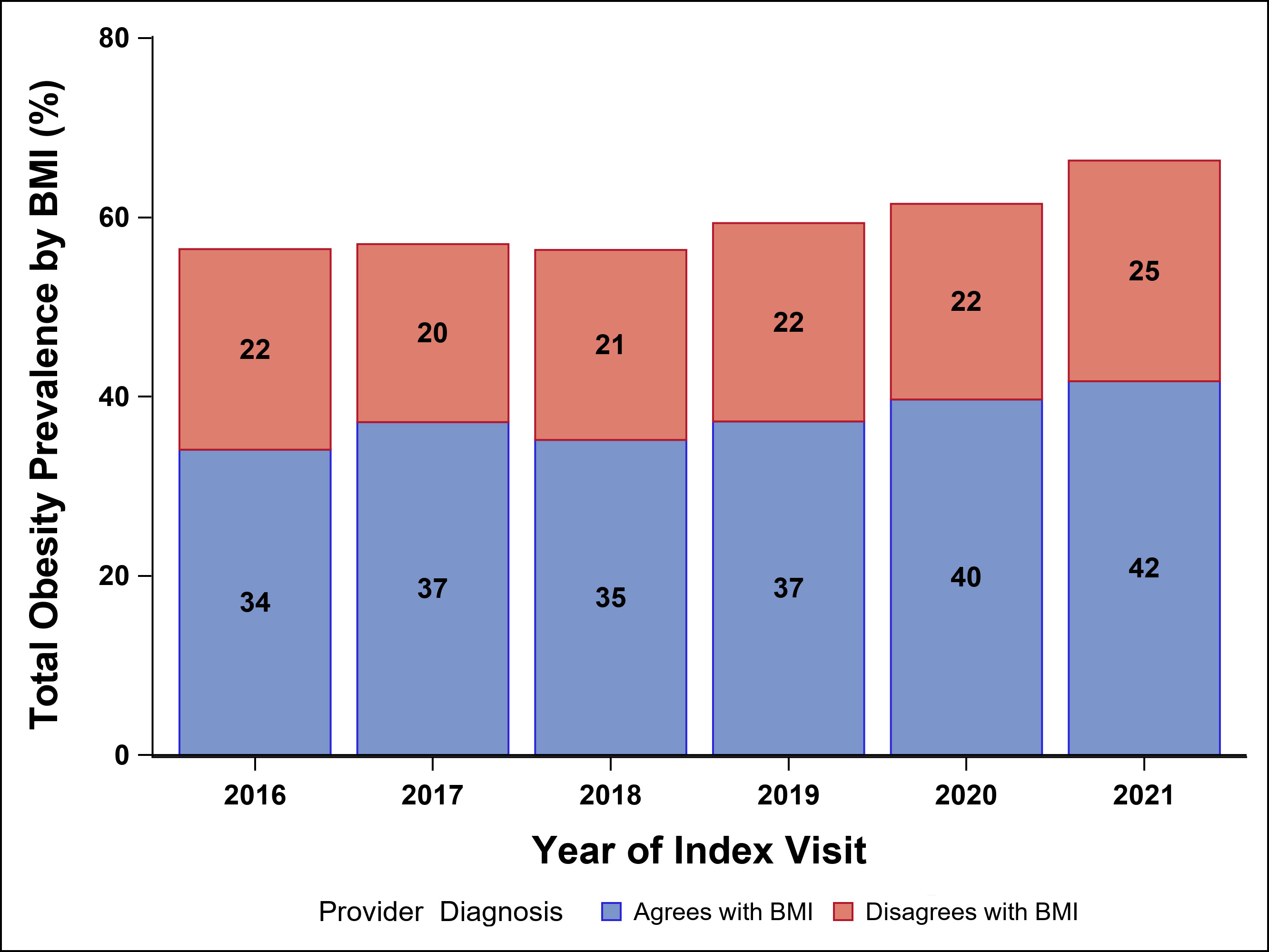 Total BMI-based obesity prevalence is shown on the Y-axis with agreement between ICD-10 code and BMI shown in blue and disagreement shown in red. Individual proportions of total prevalence per year are provided within the bars.
Total BMI-based obesity prevalence is shown on the Y-axis with agreement between ICD-10 code and BMI shown in blue and disagreement shown in red. Individual proportions of total prevalence per year are provided within the bars.
Table 1: Agreement between Provider Diagnosis ICD-10 Code-Based Obesity and BMI-Defined Obesity for the Entire Study Period with Predictive Statistics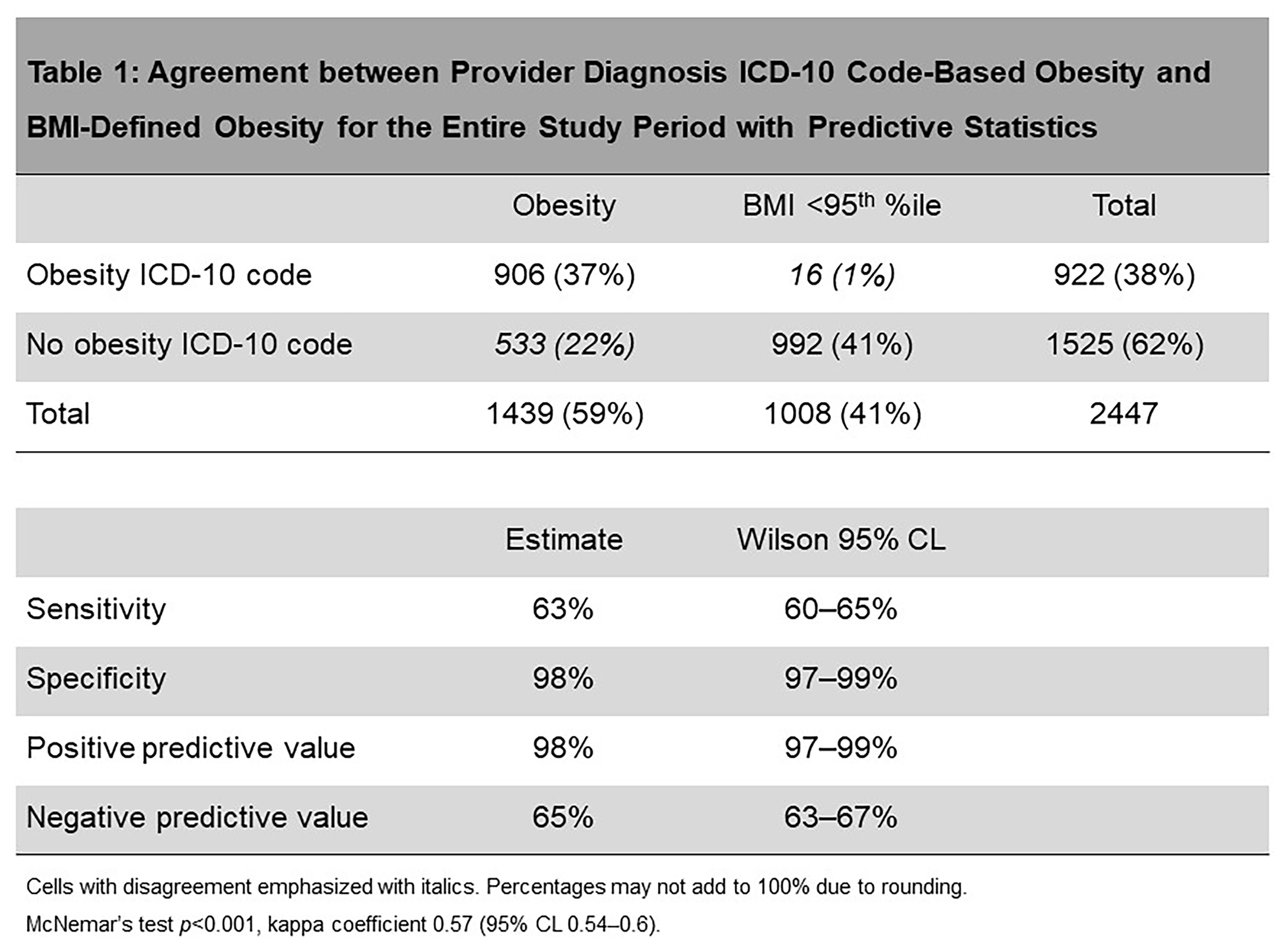 Cells with disagreement emphasized with italics. Percentages may not add to 100% due to rounding.
Cells with disagreement emphasized with italics. Percentages may not add to 100% due to rounding.
McNemar’s test p < 0.001, kappa coefficient 0.57 (95% CL 0.54–0.6).
Objective: Determine whether providers accurately diagnose obesity by ICD-10 code documentation compared to body mass index (BMI)-based obesity classification at the initial clinic visit.
Design/Methods: Interim analysis of Phase 1.1 baseline data from The Study of the Epidemiology of Pediatric Hypertension (SUPERHERO) Registry, a multicenter retrospective cohort of youth referred to subspecialty care for hypertensive disorders. Data were available from two centers and were collected via electronic health record queries using a common data model. Inclusion criteria were initial visit to a subspecialty clinic for ICD-10 code-identified hypertensive disorders from 1/1/2016 to 6/30/2021 and age < 19 years. Exclusion criteria were kidney failure on dialysis, kidney transplantation, or pregnancy by ICD-10 code and, for this analysis, missing BMI values and age < 2 years. We examined obesity prevalence across the study period with Cochran-Armitage trend test. We compared obesity by ICD-10 code-based provider diagnosis (ICD-obesity) with presence of actual obesity (BMI-obesity) defined as BMI ≥95th %ile for age/sex per CDC criteria. We calculated McNemar’s test for agreement, kappa coefficients, sensitivity, specificity, and positive and negative predictive values.
Results: Of 2447 participants, median age was 14.4 years [IQR 11.5, 16.4], 37% were female, 29% were Black or African American, 49% were White or Caucasian, and 18% were Hispanic or Latino. Across the study period, BMI-obesity and ICD-obesity prevalence increased over time from 56 to 66% and 35 to 42%, respectively (p=0.009; Figure 1). ICD-obesity had moderate agreement with BMI-obesity overall and per year, with a missed obesity diagnosis occurring in 20–25% (all McNemar’s test p< 0.001, kappa 0.55–0.6); there was no trend over time (p=0.8). Overall, ICD-obesity had 98% specificity and positive predictive value to predict BMI-obesity, but only 63% sensitivity and 65% negative predictive value (Table 1).Conclusion(s): In a large multicenter cohort of youth referred for hypertensive disorders, obesity increased in prevalence over time but was frequently undiagnosed. Ongoing analyses are investigating why we observed these patterns and the consequences of missed diagnoses, including estimating rates of referrals to Nutrition and Metabolic Clinics.
Figure 1: Agreement between Provider Obesity Diagnosis by ICD-10 Code and BMI-Based Obesity Prevalence by Year of Initial Clinic Visit
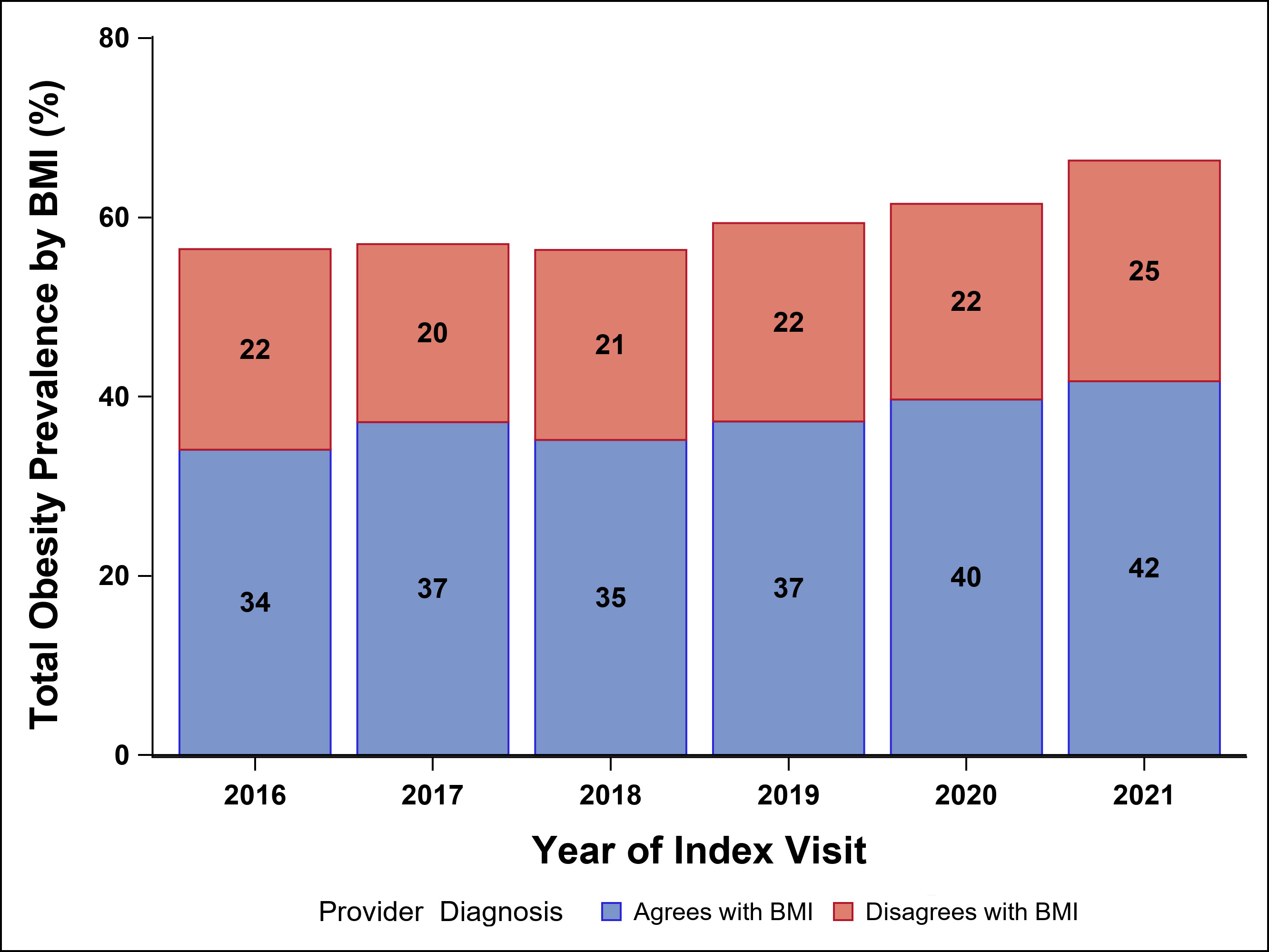 Total BMI-based obesity prevalence is shown on the Y-axis with agreement between ICD-10 code and BMI shown in blue and disagreement shown in red. Individual proportions of total prevalence per year are provided within the bars.
Total BMI-based obesity prevalence is shown on the Y-axis with agreement between ICD-10 code and BMI shown in blue and disagreement shown in red. Individual proportions of total prevalence per year are provided within the bars.Table 1: Agreement between Provider Diagnosis ICD-10 Code-Based Obesity and BMI-Defined Obesity for the Entire Study Period with Predictive Statistics
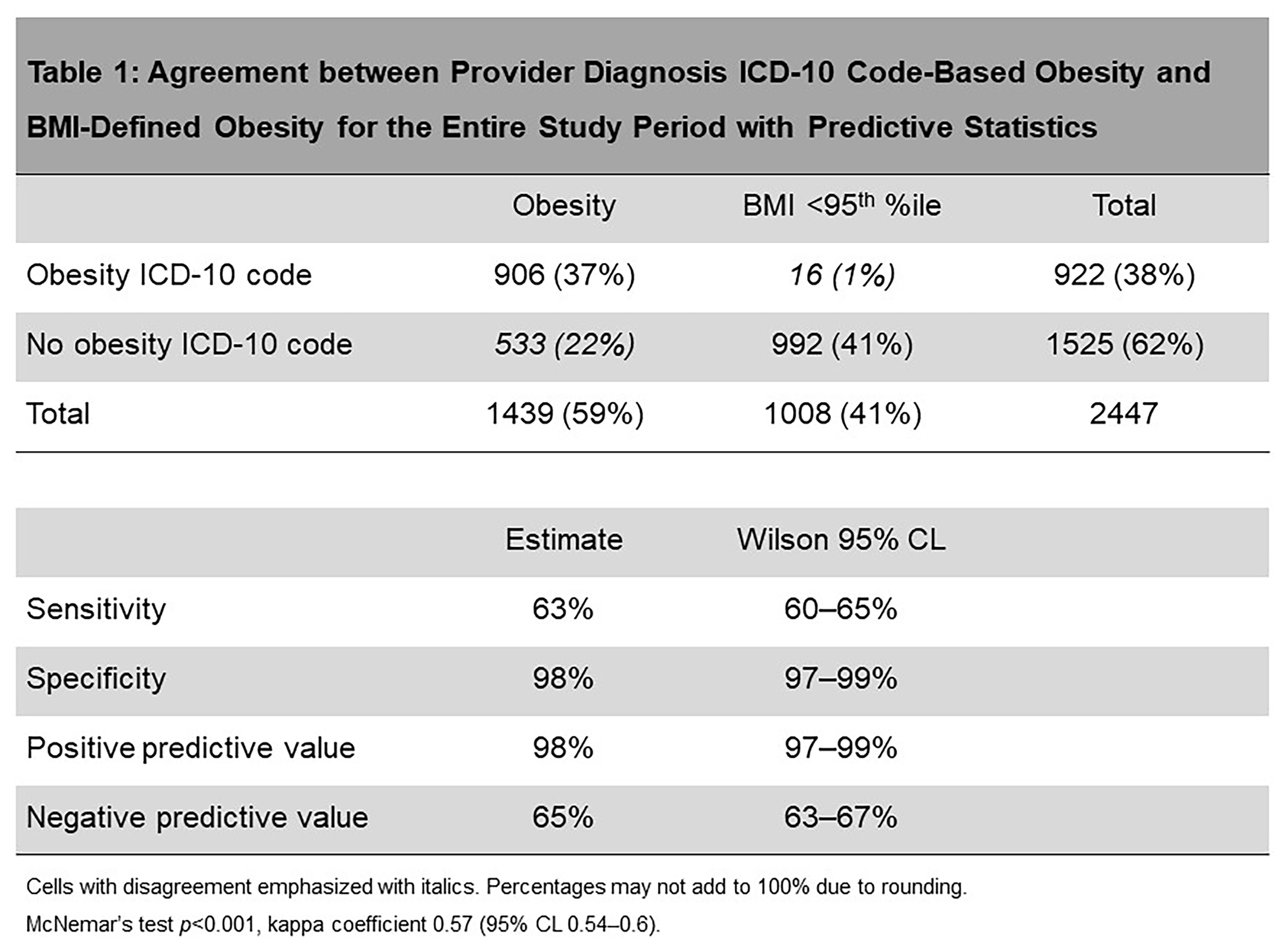 Cells with disagreement emphasized with italics. Percentages may not add to 100% due to rounding.
Cells with disagreement emphasized with italics. Percentages may not add to 100% due to rounding.McNemar’s test p < 0.001, kappa coefficient 0.57 (95% CL 0.54–0.6).
