Cardiology
Category: Abstract Submission
Cardiology II
93 - Impact of Congenital Heart Disease on the Outcomes of Very Low Birth Weight Infants
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 93
Publication Number: 93.303
Publication Number: 93.303
Xuxin Chen, Stanford University School of Medicine, Sunnyvale, CA, United States; David M. Kwiatkowski, Stanford University School of Medicine, Palo Alto, CA, United States; Shazia Bhombal, Stanford university, Palo Alto, CA, United States; Valerie Y. Chock, Stanford University School of Medicine, Sunnyvale, CA, United States

Xuxin Chen, MD, MS
Fellow
Stanford University School of Medicine
Stanford University School of Medicine
Sunnyvale, California, United States
Presenting Author(s)
Background: The incidence of very low birth weight infants < 1500 g with congenital heart disease (CHD-VLBWs) has been increasing. Preterm infants with CHD have increased rates of death or severe morbidity compared to term infants with CHD. However, it is unclear if these poor outcomes are primarily a result of prematurity itself, or the extent to which the added burden of a congenital heart defect contributes to these poor outcomes.
Objective: This study aimed to investigate the significance of CHD on morbidity and mortality of VLBW infants.
Design/Methods: This matched case-control study included VLBW infants born at a single institution between 2001-2015. The primary outcome was mortality. Secondary outcomes included necrotizing enterocolitis, bronchopulmonary dysplasia (BPD), sepsis, retinopathy of prematurity, and intraventricular hemorrhage. These outcomes were assessed by comparing CHD-VLBWs with control VLBW infants matched by GA within a week, birth weight within 500 g, sex, and birth date within a year using conditional logistic regression. Multivariable logistic regression analyzed differences in outcomes in the CHD-VLBW group between two birth periods (2001-2008 and 2009-2015) to account for changes in practice.
Results: In a cohort of 44 CHD infants matched with 88 controls, the mean (SD) GA was 30.4 (2.8) weeks and mean (SD) birth weight was 1179 (317) g. Among the CHD group, 36% had cyanotic disease with a mean (SD) postmenstrual age at surgery of 33.3 (4.0) weeks. The CHD group had more ventilation days [SD] compared to controls (29.0 [35.4] vs. 6.5 [12.4]; p < 0.001). The mortality rate was 25% in infants with CHD and 1% in controls. The CHD-VLBWs had increased BPD; (OR 7.70, 95% CI: 1.96-30.29), sepsis (OR 10.59, 95% CI: 2.99-37.57), and death (p < 0.0001) compared to the control VLBWs (Table 1). When adjusted for pre-operative ventilator use, the CHD-VLBWs still had significantly higher odds of BPD (OR 6.97, 95% CI: 1.73-28.04). CHD-VLBWs also had significantly higher odds of both presumed and culture-positive sepsis as well as late onset sepsis than their matched controls (Table 1). There were no significant differences in outcomes between the two birth periods (Table 2).Conclusion(s): CHD-VLBWs showed higher odds of BPD, sepsis, and mortality than VLBW infants without CHD. Future research should focus on the increased mortality and specific complications encountered by VLBW infants with CHD and implement targeted strategies to address these risks.
Xuxin Chen CV for APA Award SubmissionChenX_CV_082021.pdf
Table 2: Birth period (2001-2008 vs. 2009-2015) and outcomes of interest in the CHD-VLBW group*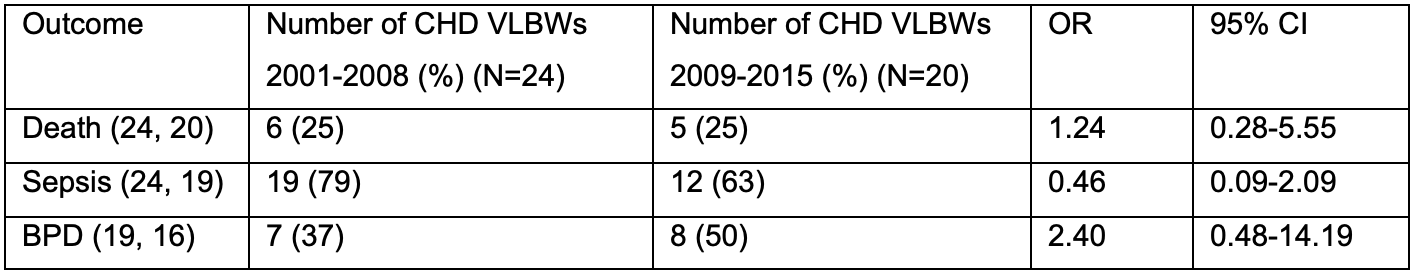 *The available n for each group is listed after the outcome as (2001-2008, 2009-2015)
*The available n for each group is listed after the outcome as (2001-2008, 2009-2015)
Objective: This study aimed to investigate the significance of CHD on morbidity and mortality of VLBW infants.
Design/Methods: This matched case-control study included VLBW infants born at a single institution between 2001-2015. The primary outcome was mortality. Secondary outcomes included necrotizing enterocolitis, bronchopulmonary dysplasia (BPD), sepsis, retinopathy of prematurity, and intraventricular hemorrhage. These outcomes were assessed by comparing CHD-VLBWs with control VLBW infants matched by GA within a week, birth weight within 500 g, sex, and birth date within a year using conditional logistic regression. Multivariable logistic regression analyzed differences in outcomes in the CHD-VLBW group between two birth periods (2001-2008 and 2009-2015) to account for changes in practice.
Results: In a cohort of 44 CHD infants matched with 88 controls, the mean (SD) GA was 30.4 (2.8) weeks and mean (SD) birth weight was 1179 (317) g. Among the CHD group, 36% had cyanotic disease with a mean (SD) postmenstrual age at surgery of 33.3 (4.0) weeks. The CHD group had more ventilation days [SD] compared to controls (29.0 [35.4] vs. 6.5 [12.4]; p < 0.001). The mortality rate was 25% in infants with CHD and 1% in controls. The CHD-VLBWs had increased BPD; (OR 7.70, 95% CI: 1.96-30.29), sepsis (OR 10.59, 95% CI: 2.99-37.57), and death (p < 0.0001) compared to the control VLBWs (Table 1). When adjusted for pre-operative ventilator use, the CHD-VLBWs still had significantly higher odds of BPD (OR 6.97, 95% CI: 1.73-28.04). CHD-VLBWs also had significantly higher odds of both presumed and culture-positive sepsis as well as late onset sepsis than their matched controls (Table 1). There were no significant differences in outcomes between the two birth periods (Table 2).Conclusion(s): CHD-VLBWs showed higher odds of BPD, sepsis, and mortality than VLBW infants without CHD. Future research should focus on the increased mortality and specific complications encountered by VLBW infants with CHD and implement targeted strategies to address these risks.
Xuxin Chen CV for APA Award SubmissionChenX_CV_082021.pdf
Table 2: Birth period (2001-2008 vs. 2009-2015) and outcomes of interest in the CHD-VLBW group*
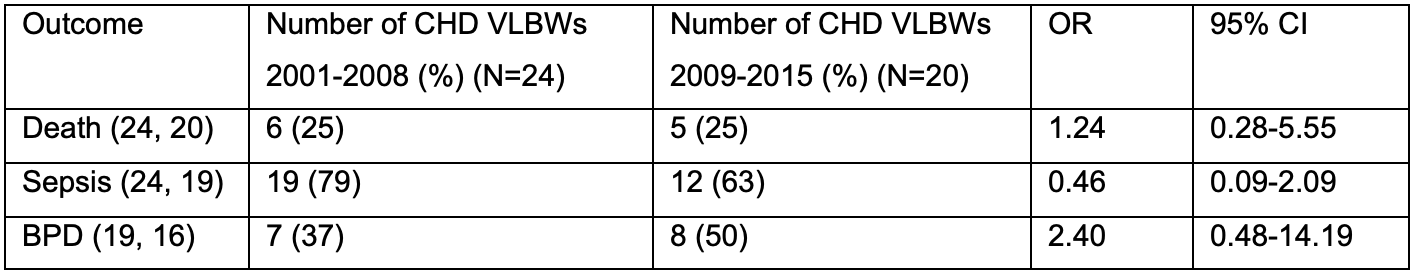 *The available n for each group is listed after the outcome as (2001-2008, 2009-2015)
*The available n for each group is listed after the outcome as (2001-2008, 2009-2015)