Children with Chronic Conditions
Category: Abstract Submission
Children with Chronic Conditions II
146 - Interfacility Transfers Among Children with Complex Chronic Conditions: Associations Between Patient-Level and Hospital-Level Factors on Transfer Outcomes
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 146
Publication Number: 146.305
Publication Number: 146.305
Diya M. Uthappa, Duke University School of Medicine, Durham, NC, United States; Tressa Ellett, Duke University School of Medicine, Durham, NC, United States; Tichelle Porch, Duke University School of Medicine, Durham, NC, United States; Aruna Rikhi, Duke Clinical Research Institute, Durham, NC, United States; Victoria Parente, Duke University School of Medicine, Durham, NC, United States; David Ming, Duke University School of Medicine, Durham, NC, United States; Michelle White, Duke University School of Medicine, Durham, NC, United States

Diya M. Uthappa
Medical Student
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: For children with complex chronic conditions (CCCs) interfacility transfer increases the risk of adverse events. Understanding predictors of transfer outcomes in patients with CCCs can provide insight into how to facilitate safe transfers.
Objective: Determine patient- and referring hospital-level predictors of transfer outcomes among children with one or more CCC transferred to a large academic medical center.
Design/Methods: Retrospective chart review revealed 2600 pediatric inpatient admissions from 2017-2019 with at least one CCC defined by ICD-10 codes. Charts were excluded if patient age >21yrs, direct admission to ICU or surgical service, born during the hospitalization or admitted via any route other than transfer from a referring hospital’s ED or inpatient ward. Patient-level factors abstracted were race/ethnicity, payor status, and zip code median income. Hospital-level factors included provider type initiating transfer and whether the referring hospital admits pediatric patients. Transfer outcomes were rapid response within 24 hours of admission, Pediatric Early Warning Score at admission, and hours to arrival. Regression analyses adjusted for age were used to determine the association between patient- or hospital-level predictors and transfer outcomes.
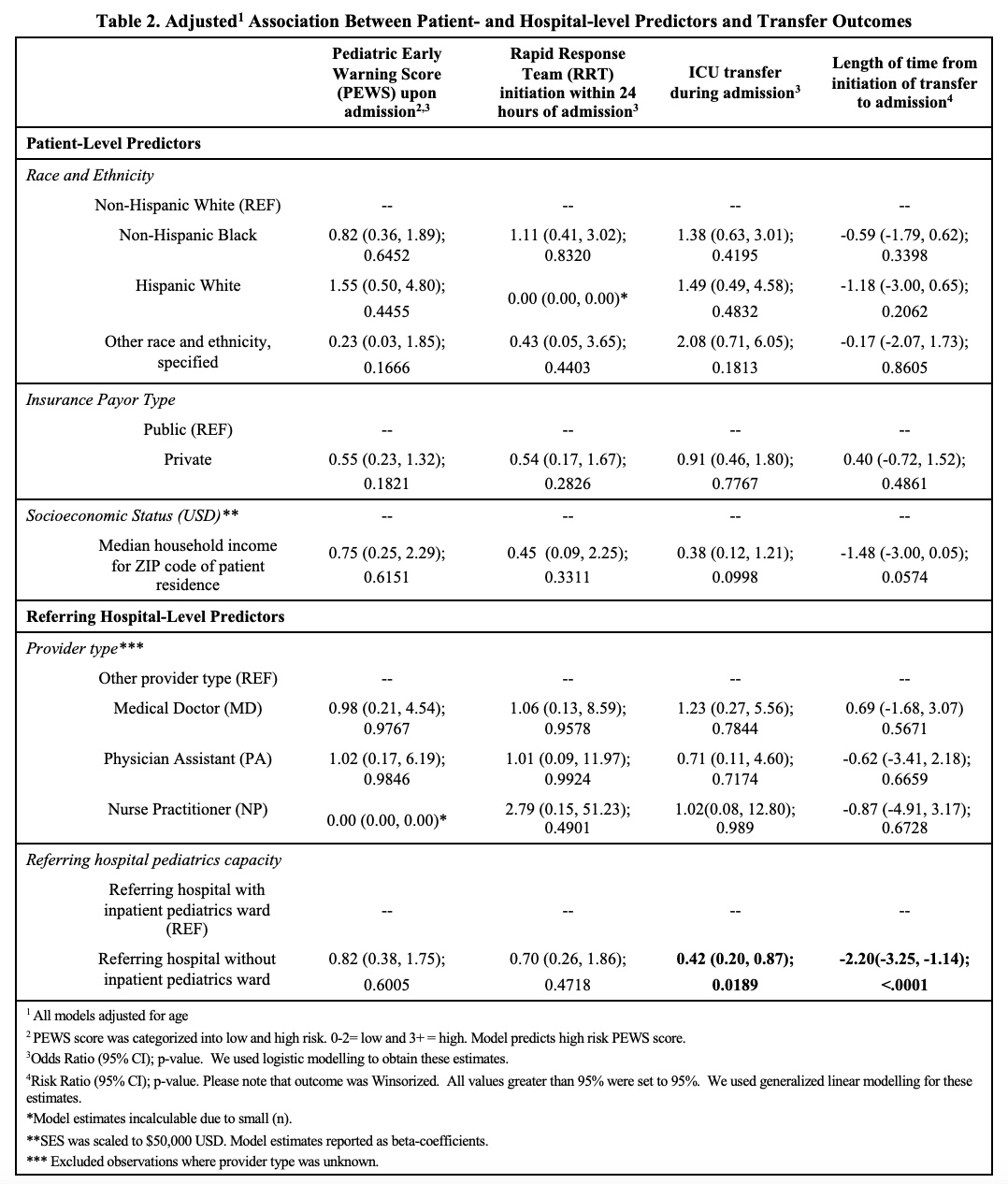
Results: 389 admissions met inclusion criteria. Approximately 34% were non-Hispanic white, 45% non-Hispanic Black, and 11% Hispanic white. More than half had public insurance (64%) and zip code-level median household income was $48,113. There were no significant associations between patient-level predictors and transfer outcomes. Hospital-level adjusted analyses indicated that transfers from hospitals without an inpatient pediatrics ward had lower odds of ICU admission during hospitalization [OR: 0.42, 95%CI:(0.20-0.87)] and shorter transfer times [RR: -2.20, 95%CI:(-3.25,-1.14)] versus transfers from hospitals with inpatient pediatrics wards. There were no significant associations between provider type initiating the transfer and transfer outcomes.Conclusion(s): For pediatric patients with one or more CCC, patient-level predictors were not associated with clinical outcomes, indicating potentially equitable outcomes among a diverse patient population. For hospital-level predictors, transfers from hospitals without an inpatient pediatric ward were less likely to require ICU admission and had shorter interfacility transfer times compared to those from hospitals with inpatient pediatrics wards likely due to a lower clinical threshold for transfer for hospitals without inpatient pediatrics wards.
Diya Uthappa CVDiya Uthappa CV 22.01.04 PAS.pdf
Table 2. Adjusted Association Between Patient- and Hospital- Level Predictors and Transfer Outcomes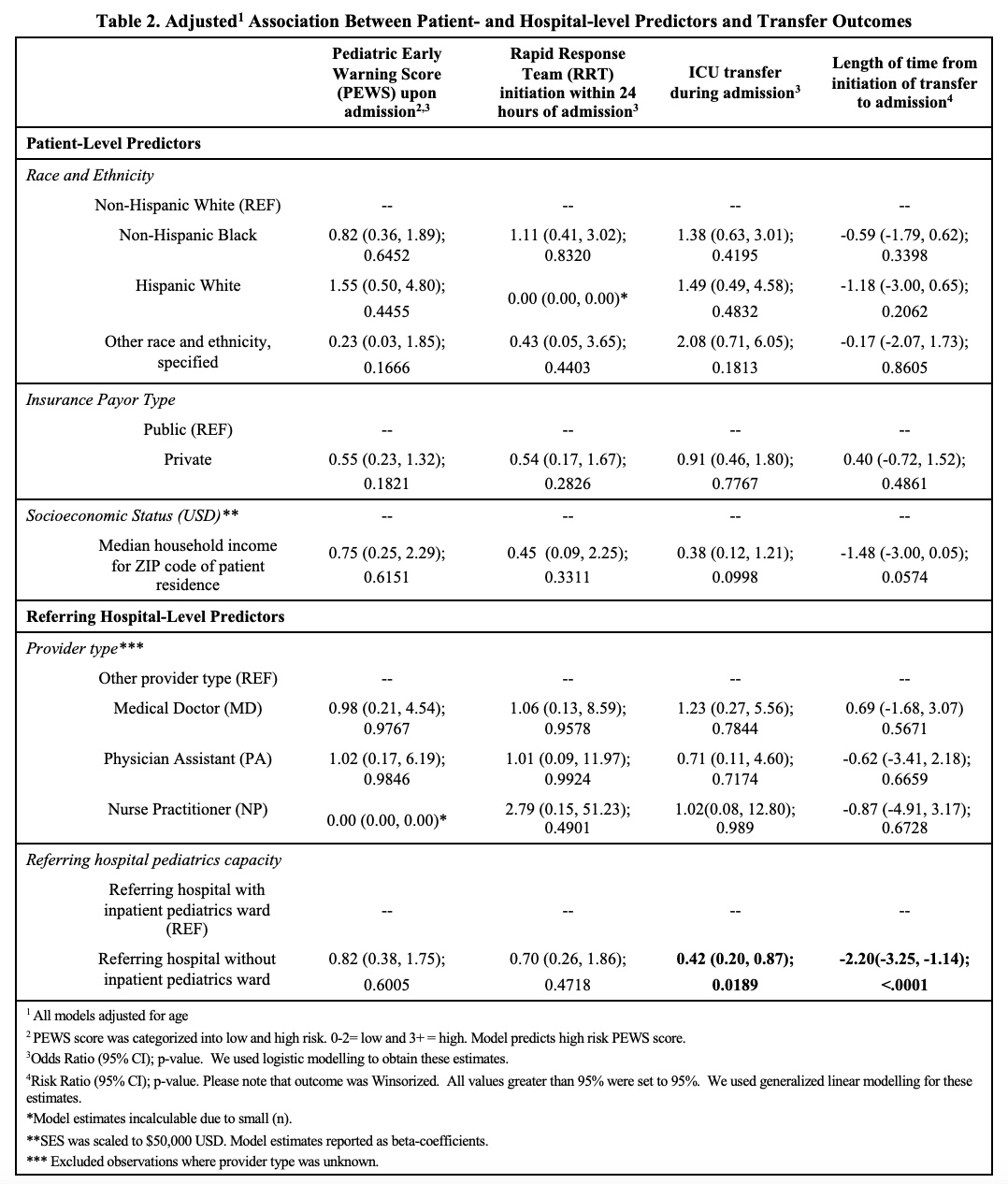
Objective: Determine patient- and referring hospital-level predictors of transfer outcomes among children with one or more CCC transferred to a large academic medical center.
Design/Methods: Retrospective chart review revealed 2600 pediatric inpatient admissions from 2017-2019 with at least one CCC defined by ICD-10 codes. Charts were excluded if patient age >21yrs, direct admission to ICU or surgical service, born during the hospitalization or admitted via any route other than transfer from a referring hospital’s ED or inpatient ward. Patient-level factors abstracted were race/ethnicity, payor status, and zip code median income. Hospital-level factors included provider type initiating transfer and whether the referring hospital admits pediatric patients. Transfer outcomes were rapid response within 24 hours of admission, Pediatric Early Warning Score at admission, and hours to arrival. Regression analyses adjusted for age were used to determine the association between patient- or hospital-level predictors and transfer outcomes.
Results: 389 admissions met inclusion criteria. Approximately 34% were non-Hispanic white, 45% non-Hispanic Black, and 11% Hispanic white. More than half had public insurance (64%) and zip code-level median household income was $48,113. There were no significant associations between patient-level predictors and transfer outcomes. Hospital-level adjusted analyses indicated that transfers from hospitals without an inpatient pediatrics ward had lower odds of ICU admission during hospitalization [OR: 0.42, 95%CI:(0.20-0.87)] and shorter transfer times [RR: -2.20, 95%CI:(-3.25,-1.14)] versus transfers from hospitals with inpatient pediatrics wards. There were no significant associations between provider type initiating the transfer and transfer outcomes.Conclusion(s): For pediatric patients with one or more CCC, patient-level predictors were not associated with clinical outcomes, indicating potentially equitable outcomes among a diverse patient population. For hospital-level predictors, transfers from hospitals without an inpatient pediatric ward were less likely to require ICU admission and had shorter interfacility transfer times compared to those from hospitals with inpatient pediatrics wards likely due to a lower clinical threshold for transfer for hospitals without inpatient pediatrics wards.
Diya Uthappa CVDiya Uthappa CV 22.01.04 PAS.pdf
Table 2. Adjusted Association Between Patient- and Hospital- Level Predictors and Transfer Outcomes