Back
Infectious Diseases
Category: Abstract Submission
Infectious Diseases: MIS-C & Kawasaki Disease
536 - Kawasaki Disease (KD) Criteria Fulfillment and Associated Outcomes in Multisystem Inflammatory Syndrome in Children (MIS-C)
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 536
Publication Number: 536.327
Publication Number: 536.327
Lyndsey D. Cole, University of Colorado School of Medicine, Centennial, CO, United States; Marsha S. Anderson, University of Colorado School of Medicine, Aurora, CO, United States; Heather R. Heizer, Children's Hospital Colorado, Aurora, CO, United States; Michelle Hite, Children's Hospital Colorado, Aurora, CO, United States; Christina M. Osborne, University of Colorado School of Medicine, Aurora, CO, United States; Samuel R. Dominguez, Children's Hospital Colorado University of Colorado, Aurora, CO, United States; Pei-Ni Jone, University of Colorado School of Medicine, Aurora, CO, United States

Lyndsey D. Cole, MD
Fellow, Pediatric Infectious Diseases & Rheumatology
University of Colorado School of Medicine
Centennial, Colorado, United States
Presenting Author(s)
Background: Multisystem inflammatory syndrome in children (MIS-C) is a hyperinflammatory illness associated with SARS-CoV-2 infection and has overlapping features with Kawasaki Disease (KD).
Objective: To describe fulfillment of complete and incomplete KD criteria among patients with MIS-C, and to compare features at admission and clinical outcomes among patients with MIS-C who did or did not meet KD criteria.
Design/Methods: Single pediatric hospital retrospective chart review of all patients who met U.S. Centers for Disease Control and Prevention (CDC) MIS-C criteria and received treatment between April 2020 to February 2021.
Results: 79 patients with MIS-C were identified. 55/79 patients (70%) met criteria for KD at admission (n=26) or later in the hospitalization (n=29). Of those, 28/55 (51%) met criteria for complete KD and 27/55 (49%) for incomplete KD. Patients meeting KD criteria at admission presented later (mean day 7 vs 5, P< 0.001) and were more likely to have rash, mucous membrane changes, conjunctivitis, extremity changes, and hypoalbuminemia at admission compared to those who did not (P=0.01, 0.005, < 0.001, 0.008, and < 0.001, respectively). There were no differences in coronary artery lesions (CAL), left ventricular (LV) dysfunction, respiratory failure, or needs for intensive care, vasoactive medications, or second- or third-line MIS-C therapy. Patients who did not meet KD criteria at admission but did later in the hospitalization were more likely to have rash, hypoalbuminemia, and elevated alanine transaminase at admission (P=0.05, 0.007, and < 0.001, respectively), respiratory failure (P=0.02), and had greater need for intensive care, vasoactive medications, and second- and third-line therapy than patients never meeting KD criteria (P < 0.001, < 0.001, 0.001, and 0.005, respectively). There were no differences in CAL or LV dysfunction.Conclusion(s): Most patients with MIS-C met criteria for KD by time of hospital discharge. Fulfillment of KD criteria at admission was not associated with changes in MIS-C patient outcomes, though fulfillment of KD criteria later during hospitalization was associated with greater need for intensive care, vasoactive medications, and second- and third-line MIS-C therapy. KD criteria fulfillment in patients with MIS-C at any timepoints was not associated with increased risk of CAL or LV dysfunction. Further investigation is needed to understand how pathophysiology of MIS-C compares to KD and if presence of KD features can help predict outcomes in MIS-C
Figure 1: Patients with MIS-C Meeting KD Criteria.png)
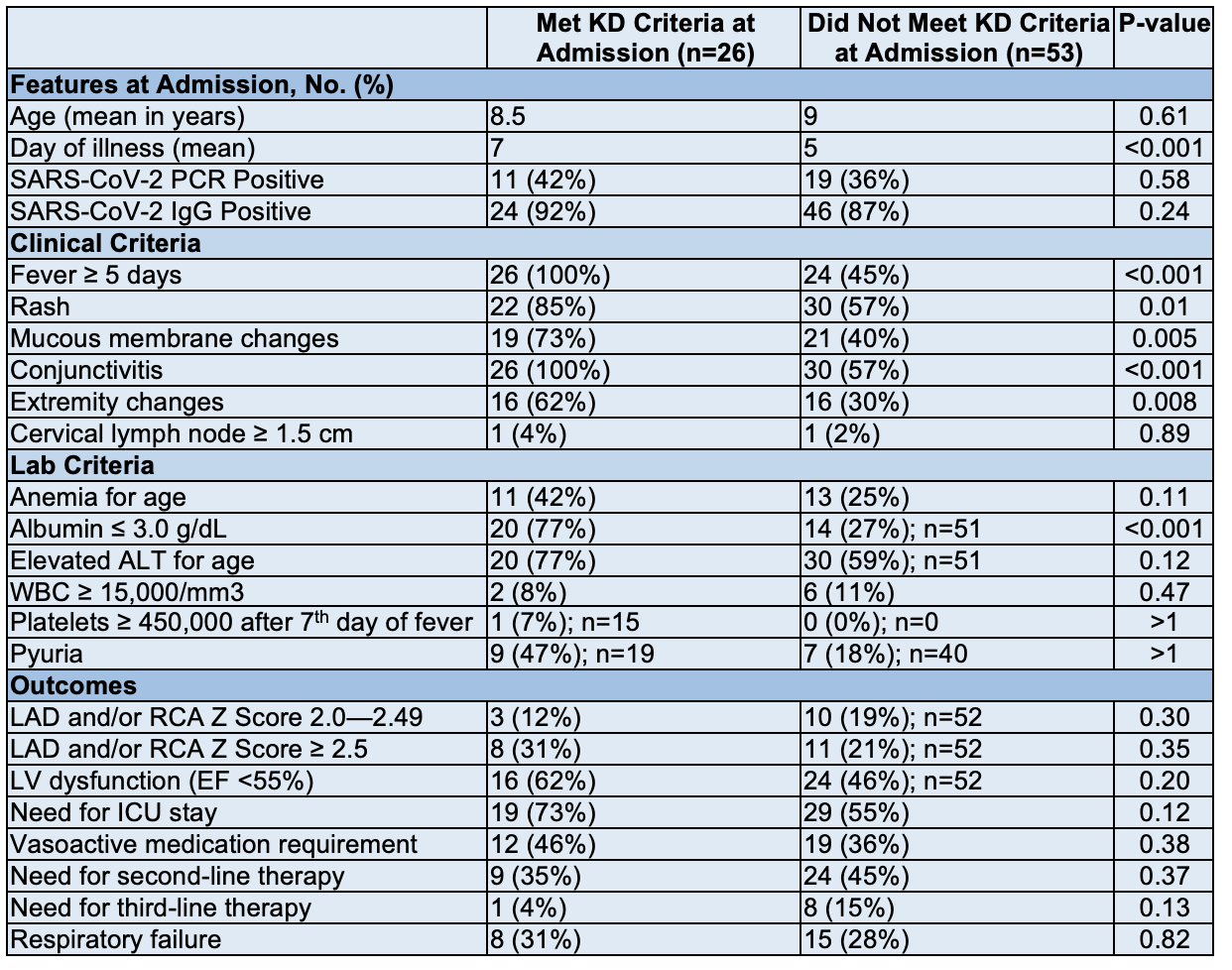
Table 1: Characteristics and Outcomes Among Patients with MIS-C Based on Presence of KD Criteria at Admission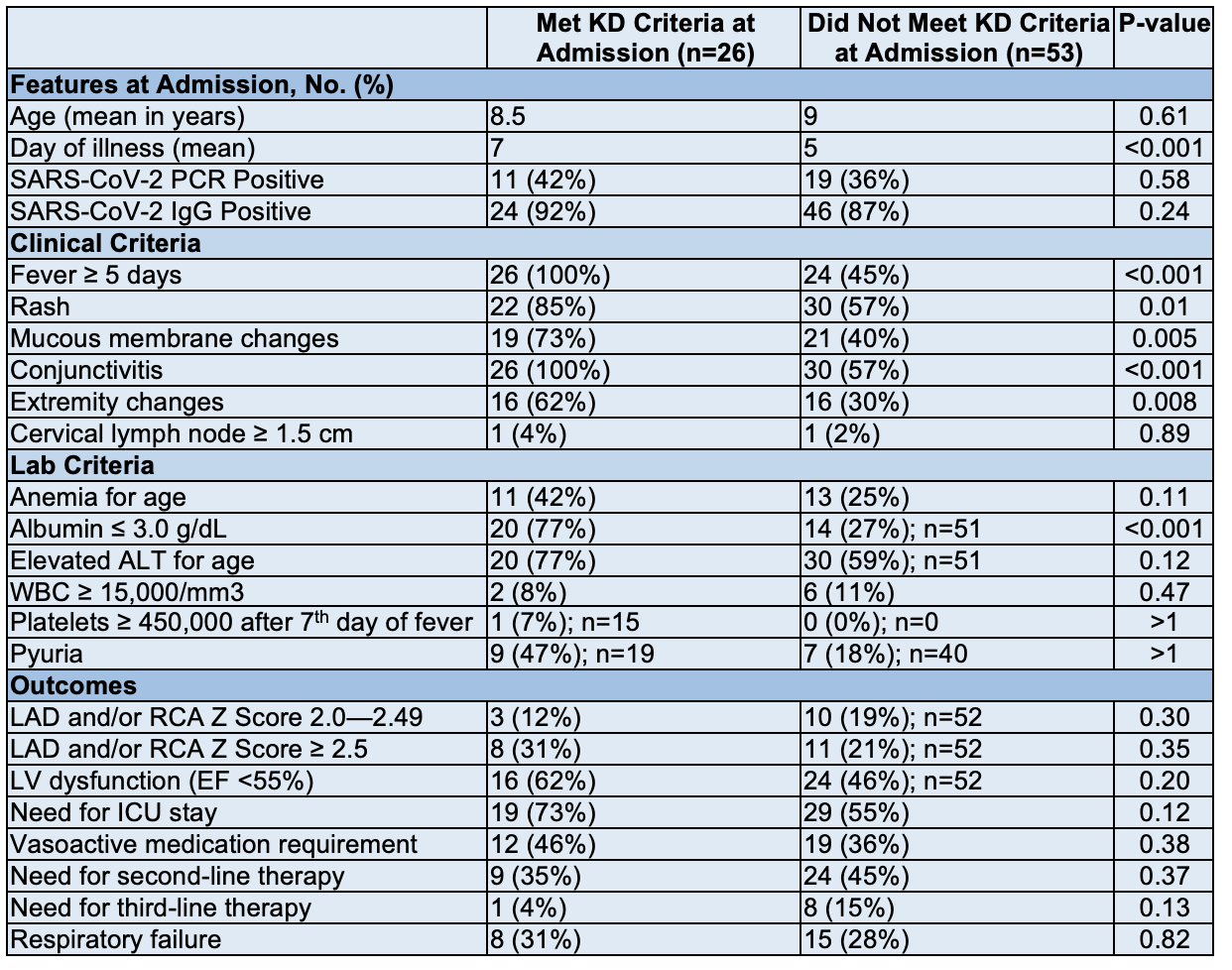
Objective: To describe fulfillment of complete and incomplete KD criteria among patients with MIS-C, and to compare features at admission and clinical outcomes among patients with MIS-C who did or did not meet KD criteria.
Design/Methods: Single pediatric hospital retrospective chart review of all patients who met U.S. Centers for Disease Control and Prevention (CDC) MIS-C criteria and received treatment between April 2020 to February 2021.
Results: 79 patients with MIS-C were identified. 55/79 patients (70%) met criteria for KD at admission (n=26) or later in the hospitalization (n=29). Of those, 28/55 (51%) met criteria for complete KD and 27/55 (49%) for incomplete KD. Patients meeting KD criteria at admission presented later (mean day 7 vs 5, P< 0.001) and were more likely to have rash, mucous membrane changes, conjunctivitis, extremity changes, and hypoalbuminemia at admission compared to those who did not (P=0.01, 0.005, < 0.001, 0.008, and < 0.001, respectively). There were no differences in coronary artery lesions (CAL), left ventricular (LV) dysfunction, respiratory failure, or needs for intensive care, vasoactive medications, or second- or third-line MIS-C therapy. Patients who did not meet KD criteria at admission but did later in the hospitalization were more likely to have rash, hypoalbuminemia, and elevated alanine transaminase at admission (P=0.05, 0.007, and < 0.001, respectively), respiratory failure (P=0.02), and had greater need for intensive care, vasoactive medications, and second- and third-line therapy than patients never meeting KD criteria (P < 0.001, < 0.001, 0.001, and 0.005, respectively). There were no differences in CAL or LV dysfunction.Conclusion(s): Most patients with MIS-C met criteria for KD by time of hospital discharge. Fulfillment of KD criteria at admission was not associated with changes in MIS-C patient outcomes, though fulfillment of KD criteria later during hospitalization was associated with greater need for intensive care, vasoactive medications, and second- and third-line MIS-C therapy. KD criteria fulfillment in patients with MIS-C at any timepoints was not associated with increased risk of CAL or LV dysfunction. Further investigation is needed to understand how pathophysiology of MIS-C compares to KD and if presence of KD features can help predict outcomes in MIS-C
Figure 1: Patients with MIS-C Meeting KD Criteria
.png)
Table 1: Characteristics and Outcomes Among Patients with MIS-C Based on Presence of KD Criteria at Admission