Back
Medical Education: Fellow
Category: Abstract Submission
Medical Education 8 - Medical Education: Fellow II
232 - Pediatric End of Life Workshop: A Safe and Novel Place for Fellows to Learn
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 232
Publication Number: 232.332
Publication Number: 232.332
Johannah M. Scheurer, University of Minnesota, Minneapolis, MN, United States; Naomi Goloff, McGill University Faculty of Medicine and Health Sciences, Montreal, PQ, Canada; Kayla Solstad, University of Minnesota, Minneapolis, MN, United States; Sonja J. Meiers, University of Wisconsin-Eau Claire, College of Nursing and Health Sciences, Rochester, MN, United States; Heidi Kamrath, Children's Hospitals and Clinics of Minnesota, St. Paul, MN, United States
- HK
Heidi Kamrath, DO (she/her/hers)
Neonatologist
University of Minnesota Medical School
St. Paul, Minnesota, United States
Presenting Author(s)
Background: The use of simulation is a common teaching-learning strategy within postgraduate medical training for high acuity, low occurrence events such as emergency codes. Our group implemented a workshop for pediatric fellows focused on improving subspecialty fellow competence and self-efficacy in delivering end of life (EOL) care. Session content includes deliberate practice and debriefing surrounding pediatric end of life care skills (PECS), with previous data analysis showing increased participant self-efficacy in PECS.
Objective: Through focus groups, we sought to understand fellows’ reflections and perceptions on workshop participation and how it influenced successive EOL care provided for their patients and families.
Design/Methods: Researchers at a midwest pediatric academic hospital used purposive sampling to recruit prior EOL workshop participants. Participation was voluntary. 12 pediatric fellows from neonatal perinatal medicine, hematology oncology and critical care programs participated across 3 focus groups. Researchers sent an introductory letter via email including the five guiding questions 6 months following participation in the PECS workshop. Facilitators led focus groups during regularly scheduled 90 minute subspecialty monthly educational sessions. Sessions were recorded for accuracy and transcribed for analysis. Each researcher individually read and highlighted transcripts for meaningful statements. Further content analysis was conducted using a modified scissor and sort technique to identify major themes and meaningful implications.
Results: Researchers identified three major themes: Burden, Safe Practice, and Self Efficacy. The themes and supporting quotes are further described in Table 1. In all focus groups, trainees described using specific skills gained from the workshop at the bedside with EOL pediatric patients and families. Real-world practice implications (Table 2) included incorporation of specific practices, improved anticipatory guidance, and increased confidence as a team leader.Conclusion(s): Subspecialty pediatric fellows found the EOL workshop to be a novel and safe space to practice EOL skills and communication, gain performance feedback from trained facilitators, and increase their self-efficacy in EOL care situations. Following workshop participation trainees translated the PECS skills learned through deliberate practice in a simulated environment into clinical practice.
Table 1. End of Life Care Skills Trainee Perceptions: Themes and Supporting Quotations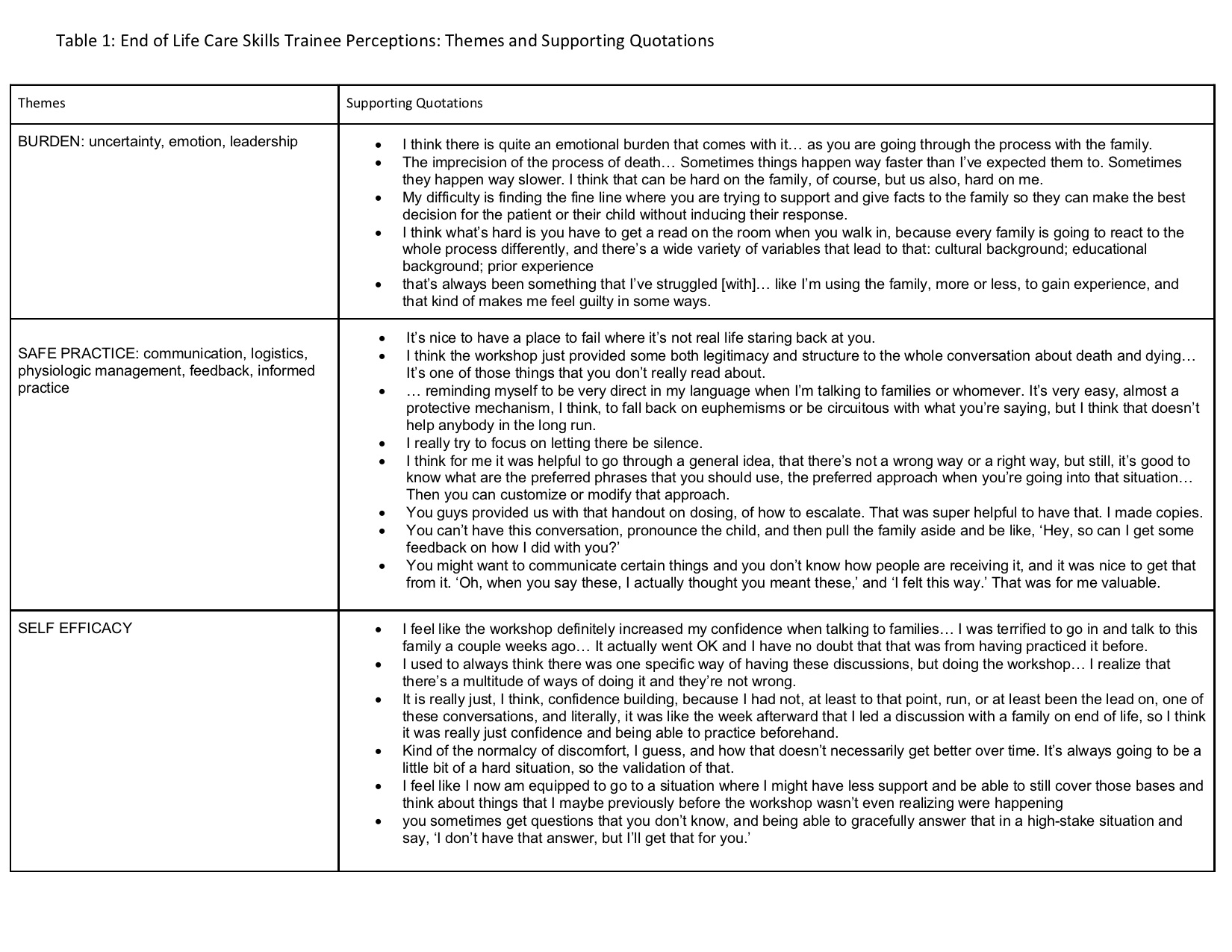
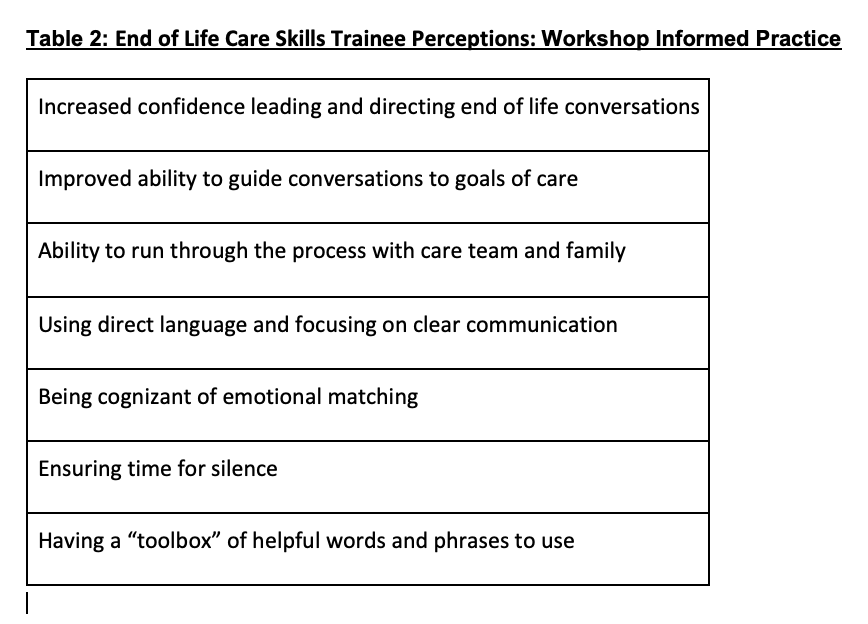
Table 2: End of Life Care Skills Trainee Perceptions: Workshop Informed Practice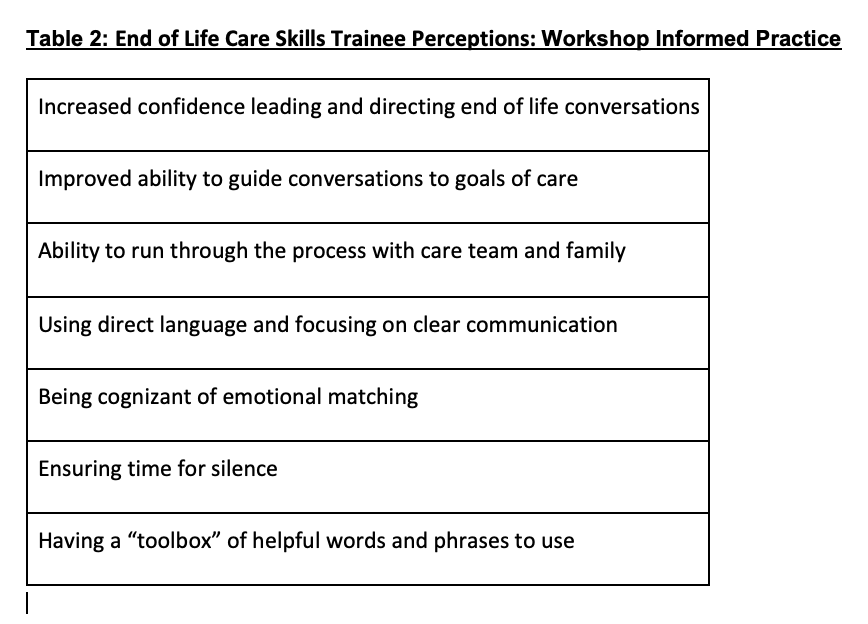
Objective: Through focus groups, we sought to understand fellows’ reflections and perceptions on workshop participation and how it influenced successive EOL care provided for their patients and families.
Design/Methods: Researchers at a midwest pediatric academic hospital used purposive sampling to recruit prior EOL workshop participants. Participation was voluntary. 12 pediatric fellows from neonatal perinatal medicine, hematology oncology and critical care programs participated across 3 focus groups. Researchers sent an introductory letter via email including the five guiding questions 6 months following participation in the PECS workshop. Facilitators led focus groups during regularly scheduled 90 minute subspecialty monthly educational sessions. Sessions were recorded for accuracy and transcribed for analysis. Each researcher individually read and highlighted transcripts for meaningful statements. Further content analysis was conducted using a modified scissor and sort technique to identify major themes and meaningful implications.
Results: Researchers identified three major themes: Burden, Safe Practice, and Self Efficacy. The themes and supporting quotes are further described in Table 1. In all focus groups, trainees described using specific skills gained from the workshop at the bedside with EOL pediatric patients and families. Real-world practice implications (Table 2) included incorporation of specific practices, improved anticipatory guidance, and increased confidence as a team leader.Conclusion(s): Subspecialty pediatric fellows found the EOL workshop to be a novel and safe space to practice EOL skills and communication, gain performance feedback from trained facilitators, and increase their self-efficacy in EOL care situations. Following workshop participation trainees translated the PECS skills learned through deliberate practice in a simulated environment into clinical practice.
Table 1. End of Life Care Skills Trainee Perceptions: Themes and Supporting Quotations
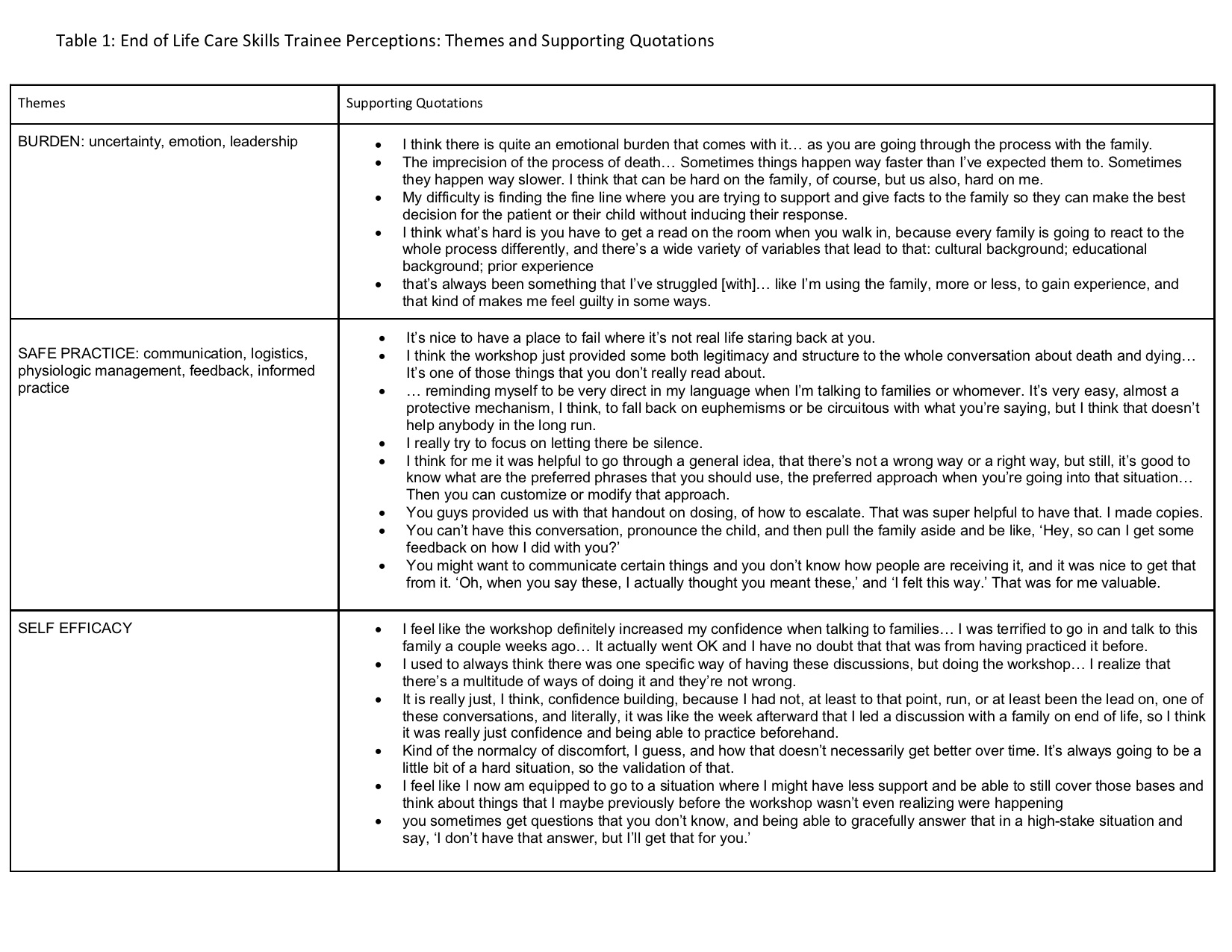
Table 2: End of Life Care Skills Trainee Perceptions: Workshop Informed Practice