Children with Chronic Conditions
Category: Abstract Submission
Children with Chronic Conditions I
138 - Pediatric Hospitalist Evaluation and Management of Unexplained Agitation and/or Irritability in Children with Severe Neurological Impairment (SNI)
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 138
Publication Number: 138.304
Publication Number: 138.304
Jennifer Kaczmarek, Cleveland Clinic Children's, Cleveland, OH, United States; Sabrina K. Tavella-Burka, Cleveland Clinic Children's, Cleveland, OH, United States; Wei Liu, Cleveland Clinic Children's, Cleveland, OH, United States; Julie H. Corder, Cleveland Clinic, Cleveland, OH, United States; Lora Sowunmi, Cleveland Clinic Children's, Cleveland, OH, United States; Hemangini Bhakta, Cleveland Clinic Children's, Cleveland, OH, United States

Jennifer Kaczmarek, MD, MSc.
Pediatric Hospital Medicine Fellow
Cleveland Clinic Children's
Cleveland, Ohio, United States
Presenting Author(s)
Background: Children with SNI often develop symptoms of agitation and/or irritability resulting in admission during which an immediate source is unidentifiable. Variations in practice can contribute to increased hospital resource utilization and length of stay (LOS).
Objective: To describe the evaluation and management of unexplained agitation and/or irritability in children with SNI admitted to a pediatric hospital medicine (PHM) service and to assess the association between reaching a definitive diagnosis and: 1) inpatient resource utilization, 2) hospital LOS and 3) readmission rate.
Design/Methods: This single-center retrospective cohort study included children ≤ 21 years of age with SNI admitted to the PHM service between 2016-2020. Patients were identified using pre-defined ICD-9/10 codes for high-intensity neurologic impairment, and specific diagnosis-related group codes and admit diagnosis descriptions identified those with unexplained agitation and/or irritability. Definitive diagnosis at time of discharge, inpatient resource utilization, hospital LOS and readmission were defined. Each admission was treated independently for analysis.
Results: 64 admissions were included. Demographic and baseline characteristics were not significantly different between groups with and without a definitive diagnosis at time of discharge (Table 1).
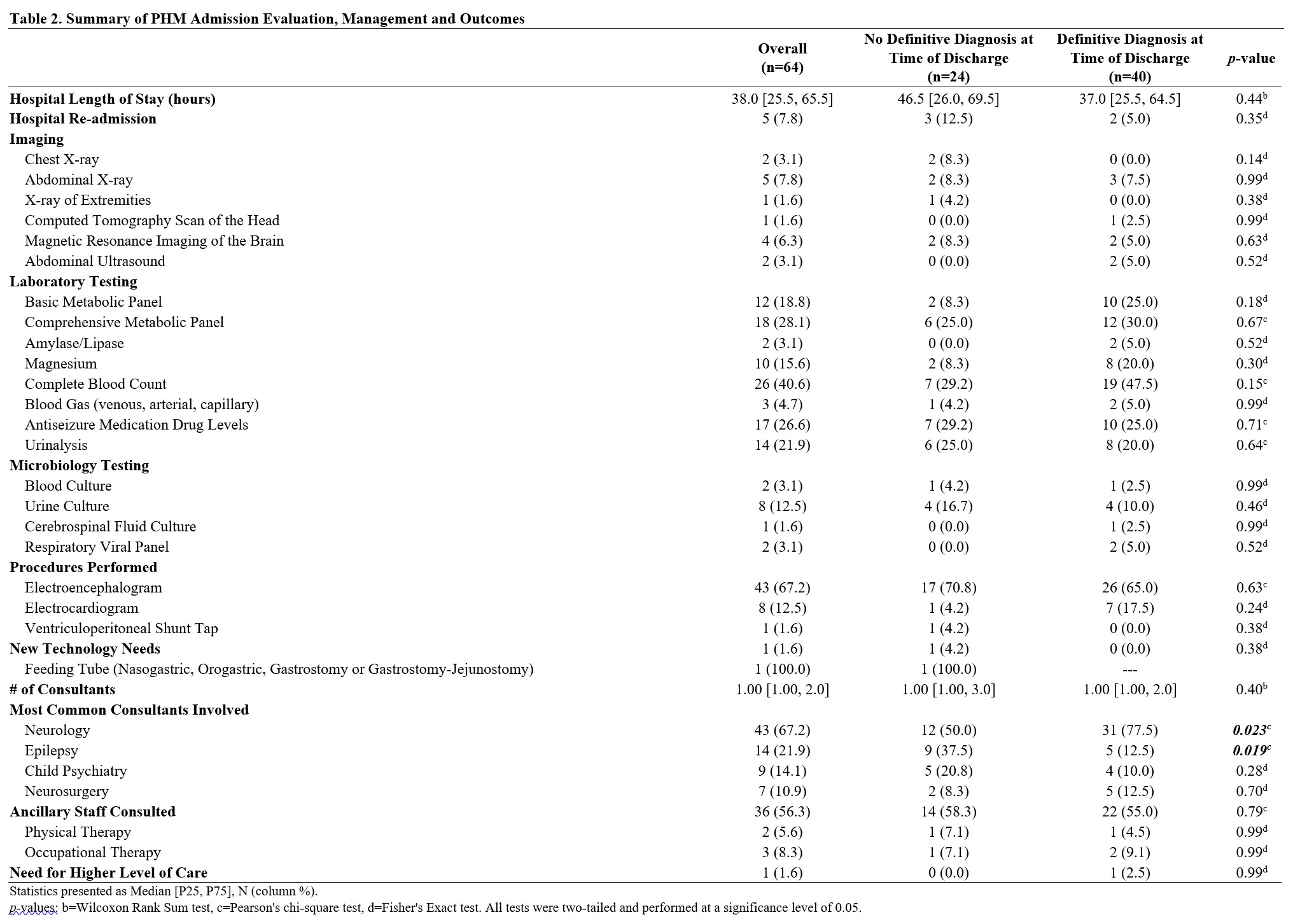
62.5% of admissions achieved a definitive diagnosis, the most common being seizure (70%). Overall inpatient evaluation, management and outcomes are summarized in Tables 2&3.
Admissions with neurology consultants (p=0.02), antiseizure medication usage, either newly initiated (p=0.005) or dosing adjustment (p=0.020), or benzodiazepine usage (p=0.03) were more likely to achieve a definitive diagnosis.
Not achieving a definitive diagnosis was not associated with any significant increase in imaging, microbiology testing, procedures performed, new technology needs or number of consultants/ancillary staff involved during hospitalization. There was no significant difference in hospital LOS or readmission rate between groups.Conclusion(s): Overall hospital LOS and readmission rate was low despite variability in evaluation and management.
Seizure was the most common diagnosis. The higher utilization rate of antiseizure medication and neurology consultation in this group likely represents a targeted and clinically warranted increase in inpatient resource utilization.
Further study is warranted to understand other factors influencing PHM provider variability when evaluating and managing unexplained agitation and/or irritability in children with SNI.
CV_Jennifer Kaczmarek_MD_MScCV_Jennifer Kaczmarek_December 2021.pdf
Table 2. Summary of PHM Admission Evaluation, Management and Outcomes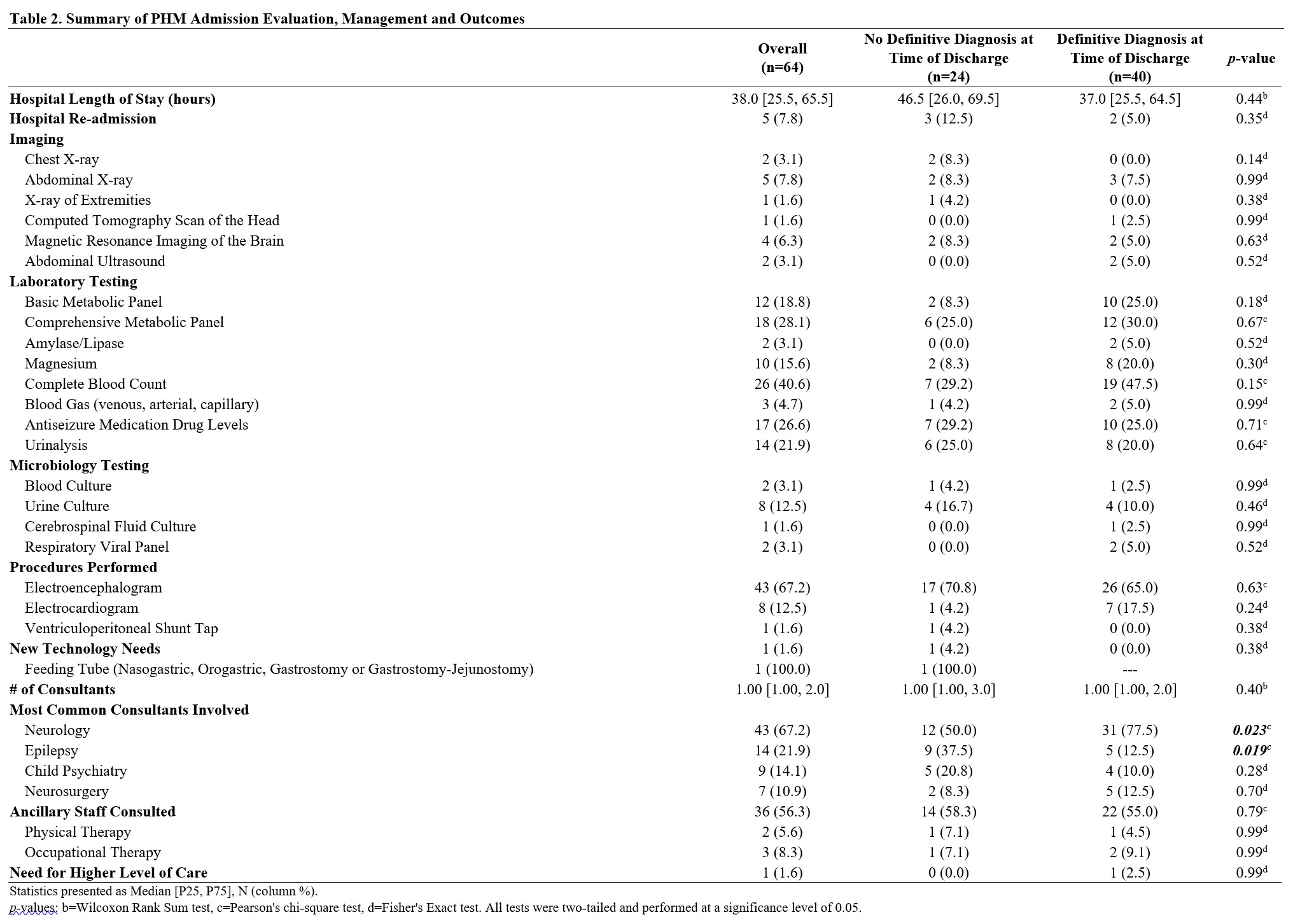
Objective: To describe the evaluation and management of unexplained agitation and/or irritability in children with SNI admitted to a pediatric hospital medicine (PHM) service and to assess the association between reaching a definitive diagnosis and: 1) inpatient resource utilization, 2) hospital LOS and 3) readmission rate.
Design/Methods: This single-center retrospective cohort study included children ≤ 21 years of age with SNI admitted to the PHM service between 2016-2020. Patients were identified using pre-defined ICD-9/10 codes for high-intensity neurologic impairment, and specific diagnosis-related group codes and admit diagnosis descriptions identified those with unexplained agitation and/or irritability. Definitive diagnosis at time of discharge, inpatient resource utilization, hospital LOS and readmission were defined. Each admission was treated independently for analysis.
Results: 64 admissions were included. Demographic and baseline characteristics were not significantly different between groups with and without a definitive diagnosis at time of discharge (Table 1).
62.5% of admissions achieved a definitive diagnosis, the most common being seizure (70%). Overall inpatient evaluation, management and outcomes are summarized in Tables 2&3.
Admissions with neurology consultants (p=0.02), antiseizure medication usage, either newly initiated (p=0.005) or dosing adjustment (p=0.020), or benzodiazepine usage (p=0.03) were more likely to achieve a definitive diagnosis.
Not achieving a definitive diagnosis was not associated with any significant increase in imaging, microbiology testing, procedures performed, new technology needs or number of consultants/ancillary staff involved during hospitalization. There was no significant difference in hospital LOS or readmission rate between groups.Conclusion(s): Overall hospital LOS and readmission rate was low despite variability in evaluation and management.
Seizure was the most common diagnosis. The higher utilization rate of antiseizure medication and neurology consultation in this group likely represents a targeted and clinically warranted increase in inpatient resource utilization.
Further study is warranted to understand other factors influencing PHM provider variability when evaluating and managing unexplained agitation and/or irritability in children with SNI.
CV_Jennifer Kaczmarek_MD_MScCV_Jennifer Kaczmarek_December 2021.pdf
Table 2. Summary of PHM Admission Evaluation, Management and Outcomes