Neonatal Neurology: Clinical
Category: Abstract Submission
Neurology 5: Neonatal Neurology Term Clinical
483 - Predictive value of the Thompson score for short-term adverse outcomes in neonatal encephalopathy patients who underwent therapeutic hypothermia
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 483
Publication Number: 483.343
Publication Number: 483.343
Jun Shibasaki, Kanagawa Childrens' Medical Center, Yokohama, Kanagawa, Japan; Hirosato Aoki, Kanagawa Children's Medical Center, Yokohama, Kanagawa, Japan; Kennosuke Tsuda, Nagoya City University, Nagoya, Aichi, Japan; Akihito Takeuchi, National Hospital Organization Okayama Medical Center, Okayama, Okayama, Japan; Yuichiro Sugiyama, Japanese Red Cross Aichi Medical Center Nagoya Daiichi Hospital, Nagoya, Aichi, Japan; Osuke Iwata, Nagoya City University, Nagoya, Aichi, Japan

Jun Shibasaki, MD
staff doctor
Kanagawa Childrens' Medical Center
Yokohama, Kanagawa, Japan
Presenting Author(s)
Background:
The rate of mortality and severe disabilities in moderate to severe neonatal encephalopathy following perinatal asphyxia is still high. Thus, withdrawal of life-sustaining treatment is considered in infants with neonatal encephalopathy expected to have very severe neurological sequelae with special health care needs. This decision is accordingly made based on a reliable prediction of poor outcomes. Parents often ask independent feeding and breathing. However, there are few reports on predictive measures of difficulty in feeding or spontaneous breathing.
Objective:
To explore the predictive value of the Thompson score during the first 4 days of life for estimating death and long-term respiratory or feeding impairment in neonatal encephalopathy.
Design/Methods:
This observational study evaluated neonatal encephalopathy infants born at ≥36 weeks of gestation and registered in a multicenter cohort of cooled infants in Japan from 2012 to 2016. The Thompson score was evaluated at 0–24, 24–48, 48–72, and 72–90 h of age. Adverse outcomes included death, survival with respiratory impairment (requiring tracheostomy or long-term intubation), or survival with feeding impairment (requiring gavage feeding) at discharge.
Results:
Of the 632 infants, 21 (3.3%) died, 59 (9.3%) survived with respiratory impairment, and 113 (17.9%) survived with feeding impairment (Table 1). All infants with respiratory impairment also had feeding impairment. The Thompson score throughout the first 4 days accurately predicted death or respiratory impairment, with areas under the curve of 0.918–0.947 and 0.869–0.913 for death or feeding impairment, respectively. The 72–90 h Thompson score showed the highest accuracy. A cutoff of ≥15 had a sensitivity of 0.85 and specificity of 0.92 for death or respiratory impairment, while a cutoff of ≥14 had a sensitivity of 0.71 and a specificity of 0.92 for death or feeding impairment (Table 2). Among the 98 patients with a Thompson score of ≥15 at 72–90 h, 9% (9/98) died, 43% (42/98) survived without tracheostomy or intubation, 48% (47/98) survived with tracheostomy or long-term intubation, and 67% (66/98) required gavage feeding (Figure 1).
Conclusion(s):
A high Thompson score during the first 4 days of life, especially at 72–90 h could thus be useful for estimating the need for prolonged life support. Owing to the rare withdrawal of life-sustaining treatment in Japan, some infants with persistent severe encephalopathy at 72-90 hours of age could regain spontaneous breathing, be extubated, and survive without tracheostomy. Meanwhile, approximately 50% of them survived with feeding impairment.
Table 1. Patient characteristics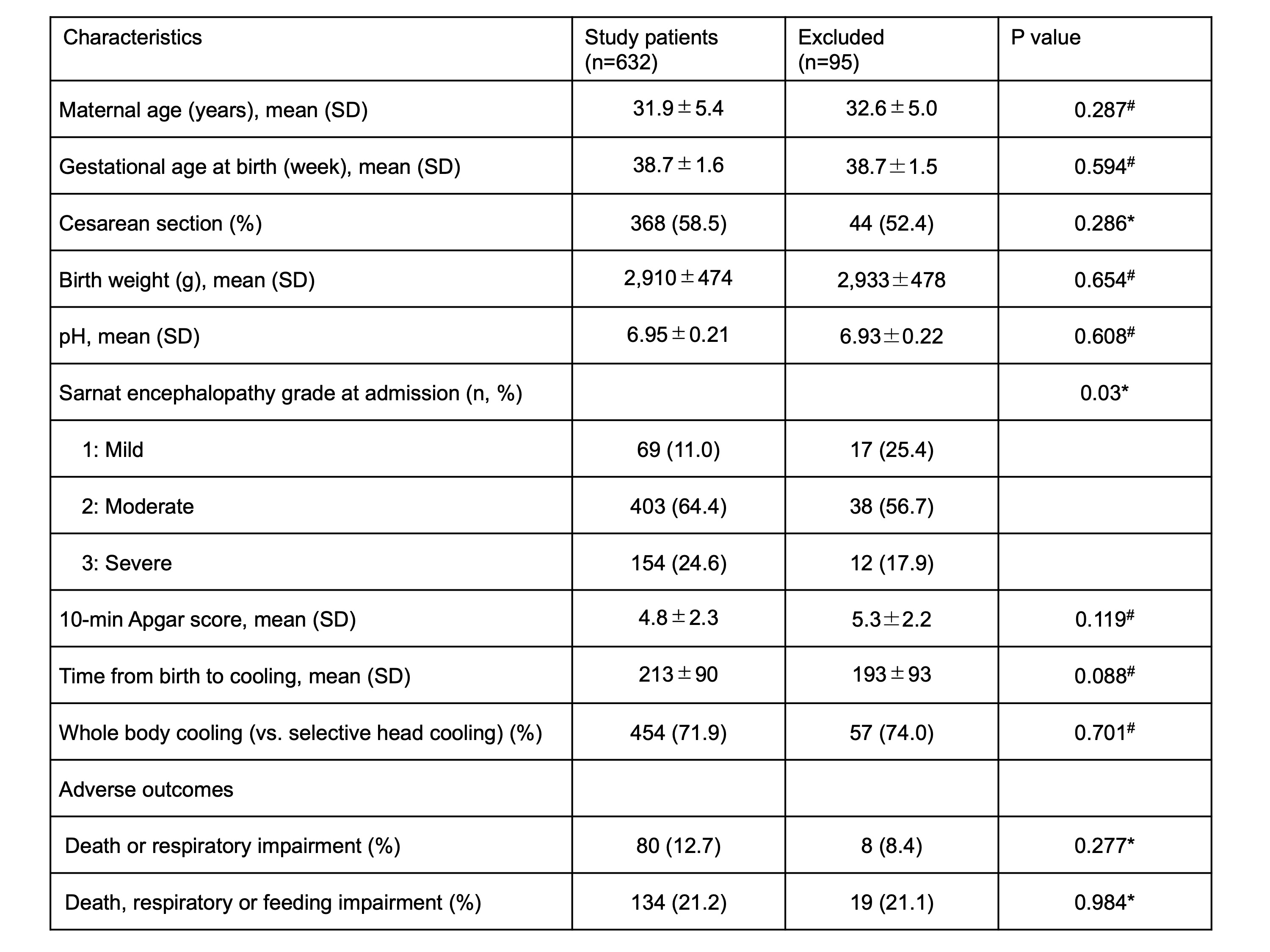 *Quantitative variables are analyzed using the Mann-Whitney U test, while qualitative variables are analyzed using the Chi-square test.
*Quantitative variables are analyzed using the Mann-Whitney U test, while qualitative variables are analyzed using the Chi-square test.
#The T-test is used for this quantitative variable.
Table 2. Prognostic utility of the Thompson score for adverse outcomes stratified by assessment period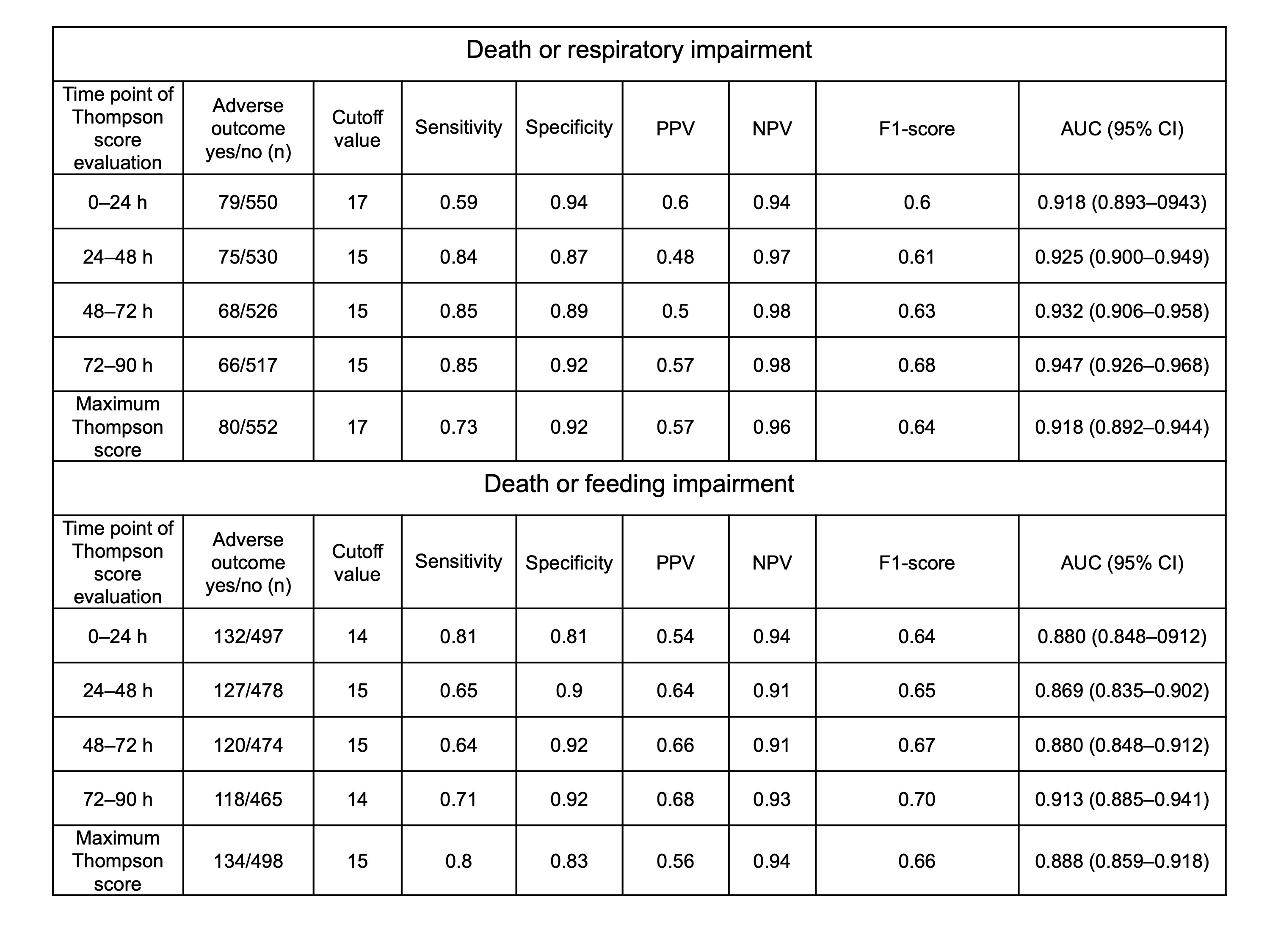 AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value
AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value
The rate of mortality and severe disabilities in moderate to severe neonatal encephalopathy following perinatal asphyxia is still high. Thus, withdrawal of life-sustaining treatment is considered in infants with neonatal encephalopathy expected to have very severe neurological sequelae with special health care needs. This decision is accordingly made based on a reliable prediction of poor outcomes. Parents often ask independent feeding and breathing. However, there are few reports on predictive measures of difficulty in feeding or spontaneous breathing.
Objective:
To explore the predictive value of the Thompson score during the first 4 days of life for estimating death and long-term respiratory or feeding impairment in neonatal encephalopathy.
Design/Methods:
This observational study evaluated neonatal encephalopathy infants born at ≥36 weeks of gestation and registered in a multicenter cohort of cooled infants in Japan from 2012 to 2016. The Thompson score was evaluated at 0–24, 24–48, 48–72, and 72–90 h of age. Adverse outcomes included death, survival with respiratory impairment (requiring tracheostomy or long-term intubation), or survival with feeding impairment (requiring gavage feeding) at discharge.
Results:
Of the 632 infants, 21 (3.3%) died, 59 (9.3%) survived with respiratory impairment, and 113 (17.9%) survived with feeding impairment (Table 1). All infants with respiratory impairment also had feeding impairment. The Thompson score throughout the first 4 days accurately predicted death or respiratory impairment, with areas under the curve of 0.918–0.947 and 0.869–0.913 for death or feeding impairment, respectively. The 72–90 h Thompson score showed the highest accuracy. A cutoff of ≥15 had a sensitivity of 0.85 and specificity of 0.92 for death or respiratory impairment, while a cutoff of ≥14 had a sensitivity of 0.71 and a specificity of 0.92 for death or feeding impairment (Table 2). Among the 98 patients with a Thompson score of ≥15 at 72–90 h, 9% (9/98) died, 43% (42/98) survived without tracheostomy or intubation, 48% (47/98) survived with tracheostomy or long-term intubation, and 67% (66/98) required gavage feeding (Figure 1).
Conclusion(s):
A high Thompson score during the first 4 days of life, especially at 72–90 h could thus be useful for estimating the need for prolonged life support. Owing to the rare withdrawal of life-sustaining treatment in Japan, some infants with persistent severe encephalopathy at 72-90 hours of age could regain spontaneous breathing, be extubated, and survive without tracheostomy. Meanwhile, approximately 50% of them survived with feeding impairment.
Table 1. Patient characteristics
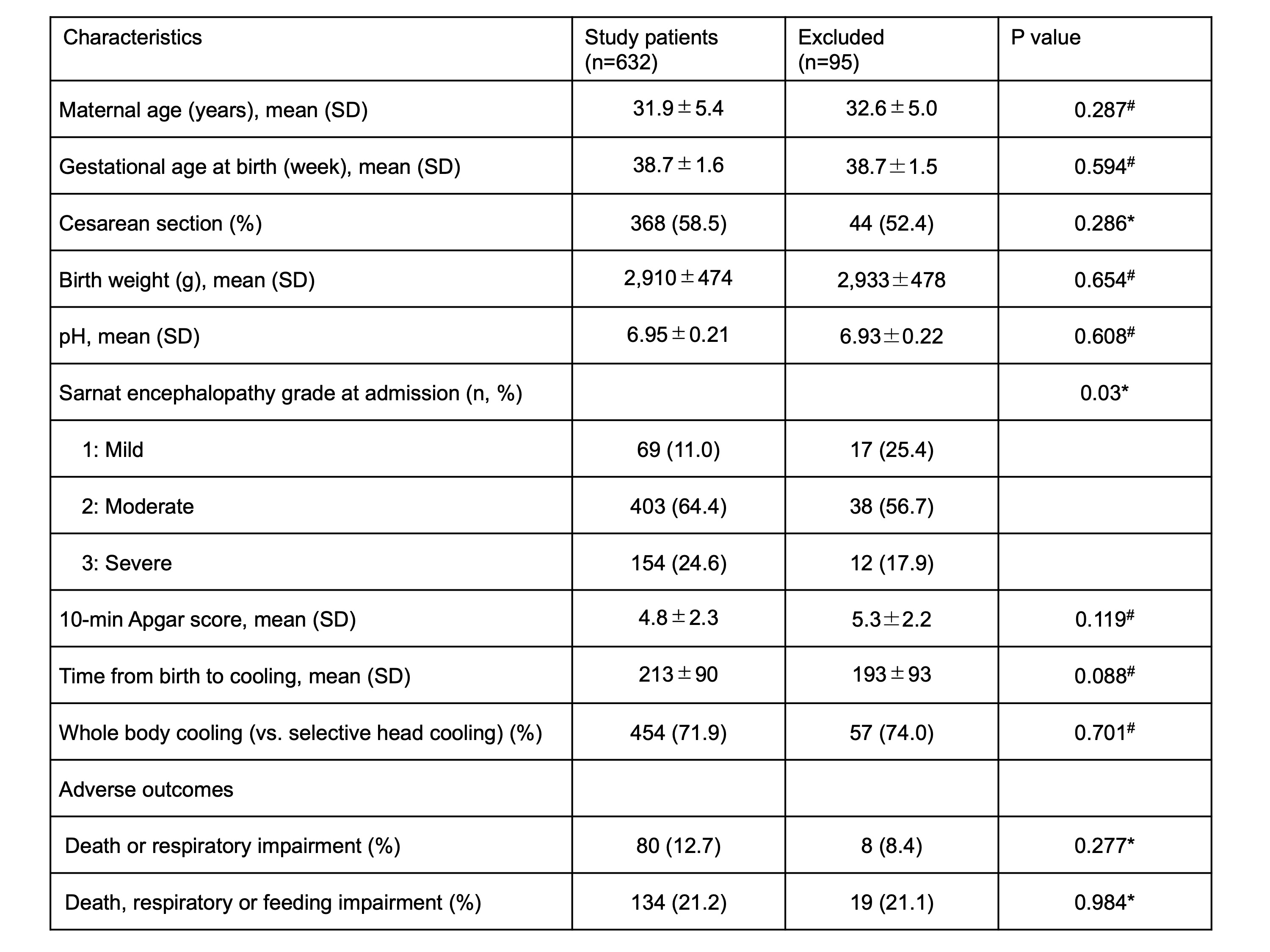 *Quantitative variables are analyzed using the Mann-Whitney U test, while qualitative variables are analyzed using the Chi-square test.
*Quantitative variables are analyzed using the Mann-Whitney U test, while qualitative variables are analyzed using the Chi-square test. #The T-test is used for this quantitative variable.
Table 2. Prognostic utility of the Thompson score for adverse outcomes stratified by assessment period
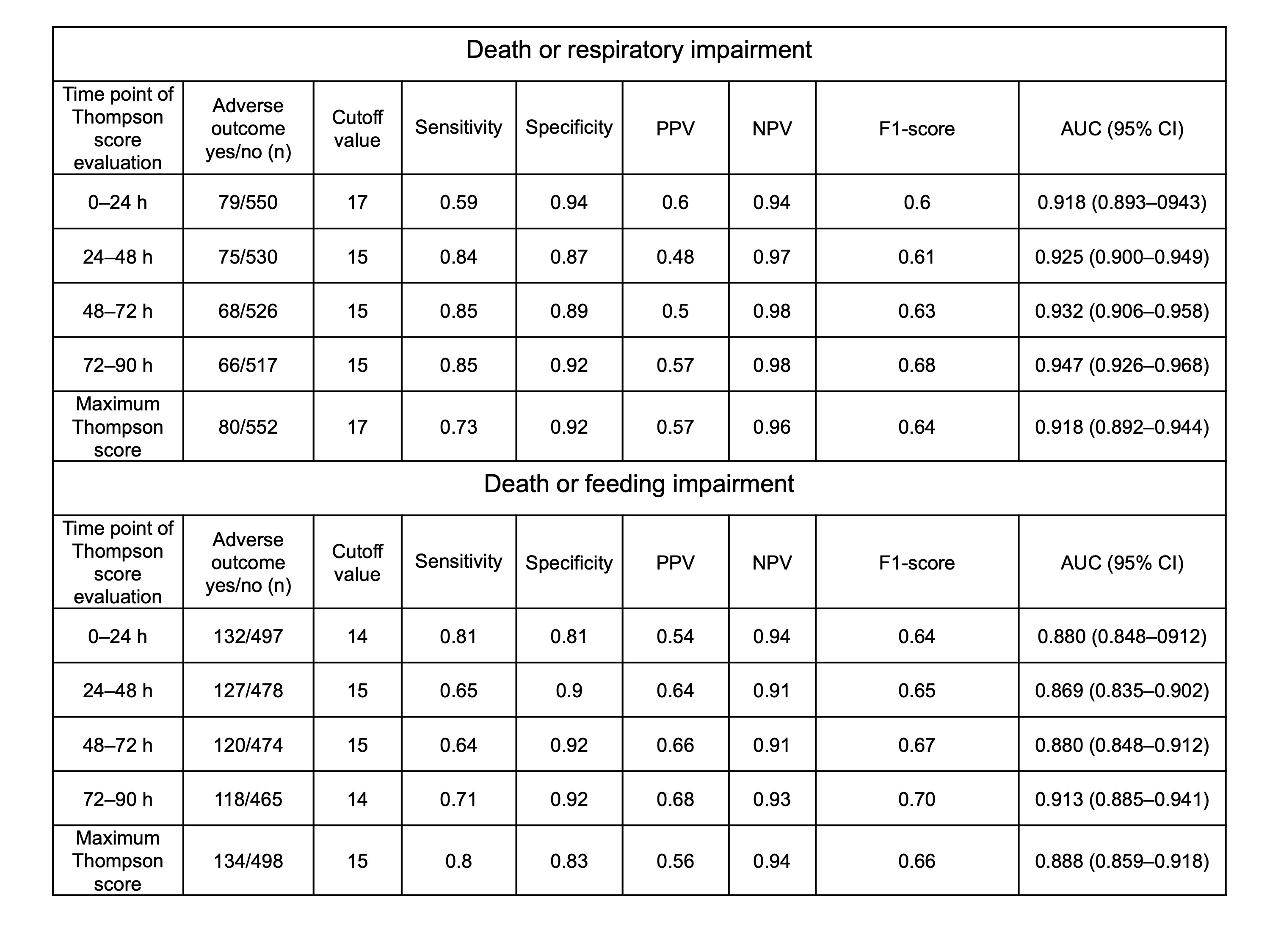 AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value
AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive value