Back
Hospital Medicine: Hospital Medicine Quality Improvement
Category: Abstract Submission
Hospital Medicine: QI
336 - Rates of ICU transfers after implementation of an I-PASS handoff document for direct admissions
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 336
Publication Number: 336.323
Publication Number: 336.323
Jayme L. Wilder, Boston Children's Hospital, Boston, MA, United States; Alexandra Aldarondo, Boston Children's Hospital, Boston, MA, United States; Beth Harper, Boston Children's Hospital, Boston, MA, United States; Elizabeth Pingree, Harvard Medical School and Boston Children's Hospital, Boston, MA, United States; David A. Johnson, Boston Children's Hospital, Norwood, MA, United States; Christopher P. Landrigan, Boston Children's Hospital, Harvard Medial School, Boston, MA, United States; Jonathan Mansbach, Boston Children's Hospital, Boston, MA, United States; Amanda Growdon, Harvard Medical School, Boston, MA, United States

Jayme Wilder, MD (she/her/hers)
Hospitalist
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Handoff failures are a leading cause of harmful medical errors. As COVID-19 emerged, our pediatric hospital medicine (PHM) service anticipated an influx of direct admissions from community hospitals closing their pediatric wards. We created an I-PASS handoff document to standardized communications during direct admissions.
Objective: Our primary aim was to reduce the number of patients transferred to the ICU within 48 hours of a direct admission to a PHM service from 1 in 36 to 1 in 60 over 18 months. A secondary aim was to increase the use of the standardized direct admission handoff document in the electronic medical record (EMR).
Design/Methods: With input from multiple stakeholders at a quaternary children’s hospital, we created, for the first time, a standardized direct admission handoff document in I-PASS format. Using the Institute for Healthcare Improvement’s Model for Improvement framework, we conducted several Plan-Do-Study-Act cycles starting in April 2020, focused on adapting the handoff document for ease of use and identification of potential safety issues, education and reminders for hospitalists, and optimization of the process for including the document in the EMR. We collected data monthly. All direct admissions to the PHM service were identified and manually reviewed to determine if an ICU transfer occurred and if the handoff document was used.
Results: Following implementation, 78% of direct admissions had a standardized handoff document in the EMR compared to 0% prior to the intervention (Fig. 1) . There was a reduction in ICU transfers within 48 hours from a baseline of 1 in every 36 direct admissions to a PHM service to < 1 in 60. There have been 56 additional direct admissions since the last ICU transfer with data collection ongoing (Fig. 2). Additionally, days between ICU transfers within 48 hours of direct admission has increased from a median of 104 days before the intervention, to a median of 228 days after the intervention (Fig. 3). Nurses, trainees, and consultants anecdotally report that the availability of the handoff document has been associated with an improvement in interdisciplinary communication. Conclusion(s): Implementation of a standardized direct admission handoff document in I-PASS format was associated with a reduction in ICU transfers within 48 hours of admission, an increase in days since the last rapid ICU transfer, and anecdotal improvements in communication among providers. Based on the success of this document, other services within our hospital are now developing similar handoff tools.
Figure 1. Percent of direct admissions with I-PASS handoff document in the EMR..png) Run chart depicting percent of direct admissions with I-PASS handoff document present in the EMR per month since implementation. Dashed line represents the median.
Run chart depicting percent of direct admissions with I-PASS handoff document present in the EMR per month since implementation. Dashed line represents the median.
G-chart: Number of direct admissions between ICU transfers within 48 hours.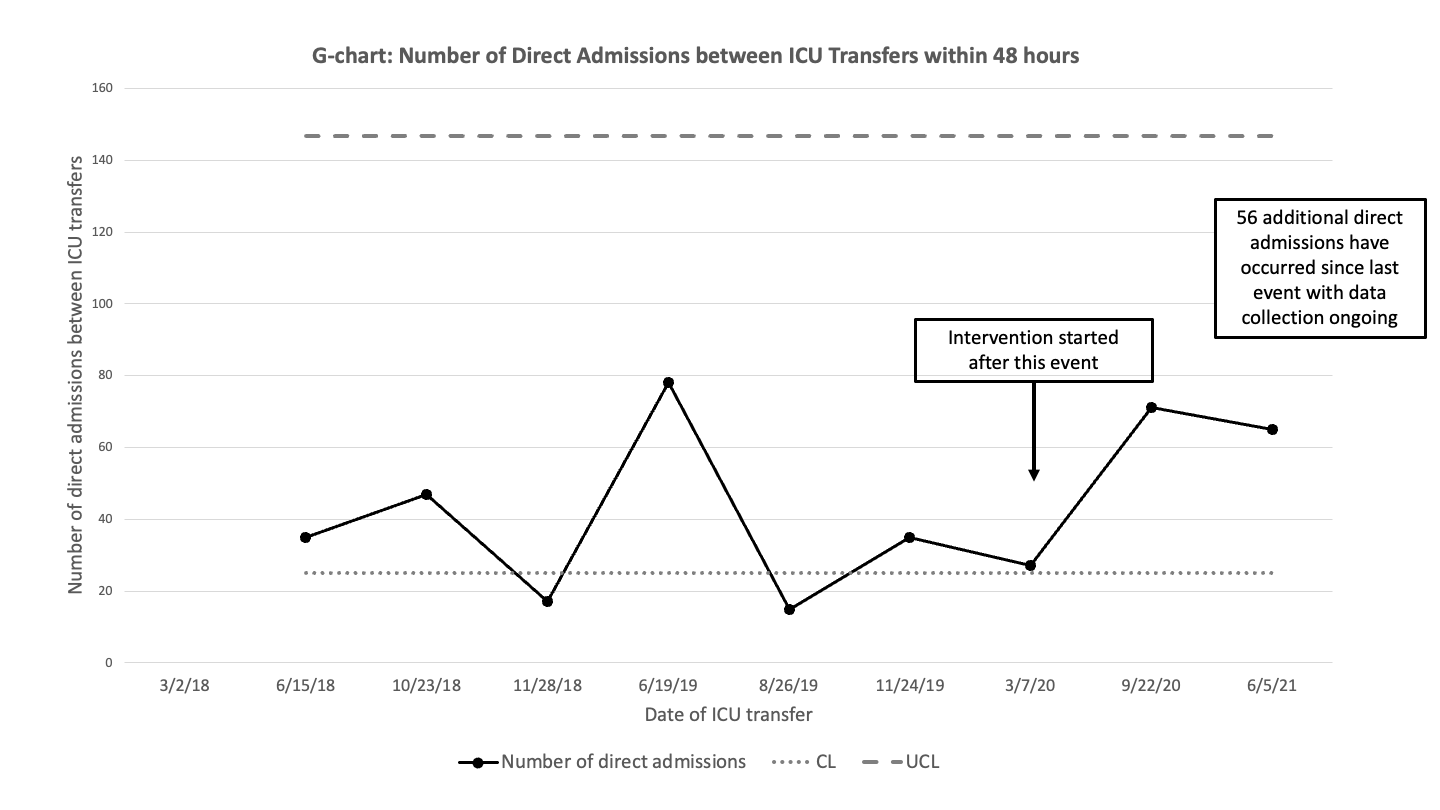 G-chart showing the number of direct admissions to the PHM service that were not transferred to ICU between direct admissions to the PHM service that were transferred to the ICU within 48 hours of admission. The upper control limit (dashed line) and center line (dotted line) are shown for the baseline.
G-chart showing the number of direct admissions to the PHM service that were not transferred to ICU between direct admissions to the PHM service that were transferred to the ICU within 48 hours of admission. The upper control limit (dashed line) and center line (dotted line) are shown for the baseline.
Objective: Our primary aim was to reduce the number of patients transferred to the ICU within 48 hours of a direct admission to a PHM service from 1 in 36 to 1 in 60 over 18 months. A secondary aim was to increase the use of the standardized direct admission handoff document in the electronic medical record (EMR).
Design/Methods: With input from multiple stakeholders at a quaternary children’s hospital, we created, for the first time, a standardized direct admission handoff document in I-PASS format. Using the Institute for Healthcare Improvement’s Model for Improvement framework, we conducted several Plan-Do-Study-Act cycles starting in April 2020, focused on adapting the handoff document for ease of use and identification of potential safety issues, education and reminders for hospitalists, and optimization of the process for including the document in the EMR. We collected data monthly. All direct admissions to the PHM service were identified and manually reviewed to determine if an ICU transfer occurred and if the handoff document was used.
Results: Following implementation, 78% of direct admissions had a standardized handoff document in the EMR compared to 0% prior to the intervention (Fig. 1) . There was a reduction in ICU transfers within 48 hours from a baseline of 1 in every 36 direct admissions to a PHM service to < 1 in 60. There have been 56 additional direct admissions since the last ICU transfer with data collection ongoing (Fig. 2). Additionally, days between ICU transfers within 48 hours of direct admission has increased from a median of 104 days before the intervention, to a median of 228 days after the intervention (Fig. 3). Nurses, trainees, and consultants anecdotally report that the availability of the handoff document has been associated with an improvement in interdisciplinary communication. Conclusion(s): Implementation of a standardized direct admission handoff document in I-PASS format was associated with a reduction in ICU transfers within 48 hours of admission, an increase in days since the last rapid ICU transfer, and anecdotal improvements in communication among providers. Based on the success of this document, other services within our hospital are now developing similar handoff tools.
Figure 1. Percent of direct admissions with I-PASS handoff document in the EMR.
.png) Run chart depicting percent of direct admissions with I-PASS handoff document present in the EMR per month since implementation. Dashed line represents the median.
Run chart depicting percent of direct admissions with I-PASS handoff document present in the EMR per month since implementation. Dashed line represents the median.G-chart: Number of direct admissions between ICU transfers within 48 hours.
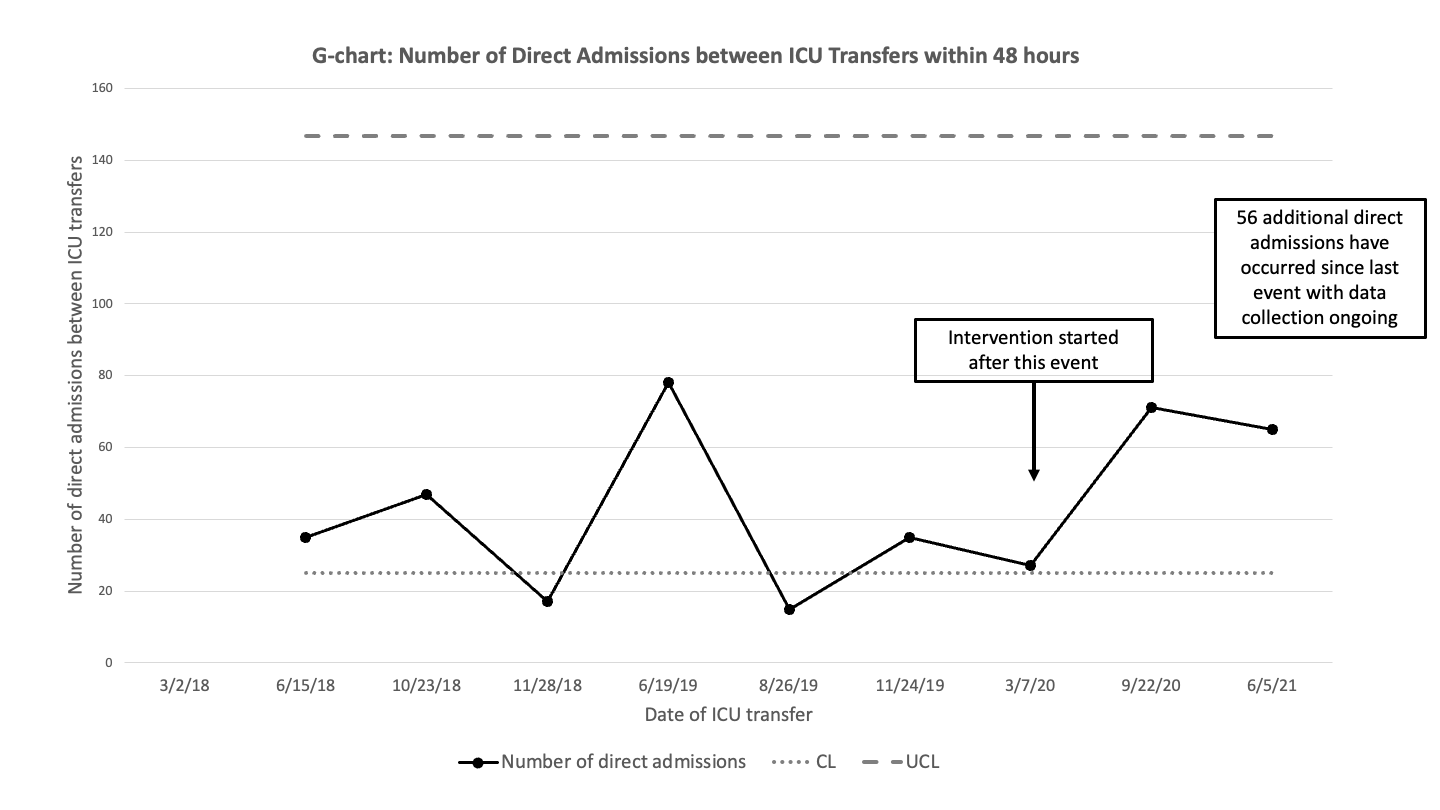 G-chart showing the number of direct admissions to the PHM service that were not transferred to ICU between direct admissions to the PHM service that were transferred to the ICU within 48 hours of admission. The upper control limit (dashed line) and center line (dotted line) are shown for the baseline.
G-chart showing the number of direct admissions to the PHM service that were not transferred to ICU between direct admissions to the PHM service that were transferred to the ICU within 48 hours of admission. The upper control limit (dashed line) and center line (dotted line) are shown for the baseline.