Hospital Medicine: Hospital Medicine Quality Improvement
Category: Abstract Submission
Hospital Medicine: QI
337 - Safely Doing Less: Shifting MRIs to the Outpatient Arena
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 337
Publication Number: 337.323
Publication Number: 337.323
Courtney Port, Inova Children's Hospital, Falls Church, VA, United States; Brooke Shuster, Inova Children's Hospital, Falls Church, VA, United States; Barbara E. Switzer, Inova Children's Hospital, Shreveport, LA, United States

Brooke Shuster, MD
Pediatric Hospitalist and Physician Advisor
Inova Children's Hospital
Falls Church, Virginia, United States
Presenting Author(s)
Background: Epilepsy is a chronic and common condition. The typical workup for patients admitted for seizures may include an electroencephalogram (EEG), brain magnetic resonance imaging (MRI) and neurology consult. Yet, only about 2% of neuroimaging reveals a clinically significant finding that would change the acute management of the patient. At our local children’s hospital, the percentage of patients with seizures receiving inpatient brain MRIs increased from just under 50% in 2018 to over 70% in 2020. Similarly, the cost per case for the diagnosis-related group (DRG) for seizures steadily increased and nearly doubled from 2018 to 2020.
Objective: Reduce the cost per case for seizure DRGs 100 and 101 by safely shifting 10% of brain MRIs to outpatient procedures by January 2022.
Design/Methods: Provider practice was analyzed for variation in diagnostic evaluation of patients presenting with unprovoked seizures. Stakeholders were gathered to create a value improvement project team. A detailed process map for obtaining an outpatient brain MRI on a pediatric patient was created. Bottlenecks and other opportunities for improvement were identified. A guideline was developed for brain MRI utilization (figure 1) and a new process was created that includes automation using the local electronic medical record (EMR) for ordering, providing patient instructions, and scheduling the outpatient brain MRI (figure 2). The Model for Improvement was utilized with PDSA cycles testing these changes for meaningful improvement in desired measures.
Results: Variation in brain MRI ordering practices among neurologists ranged from 300 to 550 per 1,000 patients. When analyzing ordering practices by neurologists over time, the percentage of patients receiving an inpatient brain MRI decreased from a median of 42% to 29% in 6 months. The financial department estimates a savings of $3000 per case by shifting the MRI to the outpatient setting. The average time from discharge to obtaining MRI was 31 days with none of these requiring urgent intervention or re-admission to the hospital.Conclusion(s): This project was successful in safely decreasing inpatient brain MRI procedures for patients hospitalized with seizures and seizure-like episodes by nearly 1/3rd. As the next step in this value improvement project, EEG ordering practices will be standardized to streamline the process to obtain a timely outpatient EEG.
Figure 1: Brain MRI ordering guidelines for pediatric patients presenting after a seizure or seizure-like episode.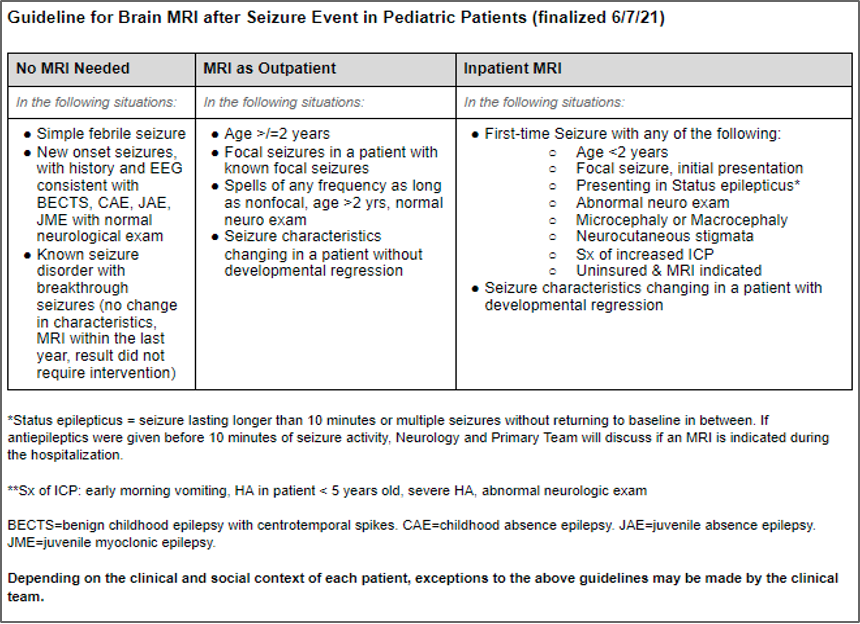 Figure 1: Brain MRI ordering guidelines for pediatric patients presenting after a seizure or seizure-like episode.
Figure 1: Brain MRI ordering guidelines for pediatric patients presenting after a seizure or seizure-like episode.
Work Flow Process Map Work flow process map
Work flow process map
Objective: Reduce the cost per case for seizure DRGs 100 and 101 by safely shifting 10% of brain MRIs to outpatient procedures by January 2022.
Design/Methods: Provider practice was analyzed for variation in diagnostic evaluation of patients presenting with unprovoked seizures. Stakeholders were gathered to create a value improvement project team. A detailed process map for obtaining an outpatient brain MRI on a pediatric patient was created. Bottlenecks and other opportunities for improvement were identified. A guideline was developed for brain MRI utilization (figure 1) and a new process was created that includes automation using the local electronic medical record (EMR) for ordering, providing patient instructions, and scheduling the outpatient brain MRI (figure 2). The Model for Improvement was utilized with PDSA cycles testing these changes for meaningful improvement in desired measures.
Results: Variation in brain MRI ordering practices among neurologists ranged from 300 to 550 per 1,000 patients. When analyzing ordering practices by neurologists over time, the percentage of patients receiving an inpatient brain MRI decreased from a median of 42% to 29% in 6 months. The financial department estimates a savings of $3000 per case by shifting the MRI to the outpatient setting. The average time from discharge to obtaining MRI was 31 days with none of these requiring urgent intervention or re-admission to the hospital.Conclusion(s): This project was successful in safely decreasing inpatient brain MRI procedures for patients hospitalized with seizures and seizure-like episodes by nearly 1/3rd. As the next step in this value improvement project, EEG ordering practices will be standardized to streamline the process to obtain a timely outpatient EEG.
Figure 1: Brain MRI ordering guidelines for pediatric patients presenting after a seizure or seizure-like episode.
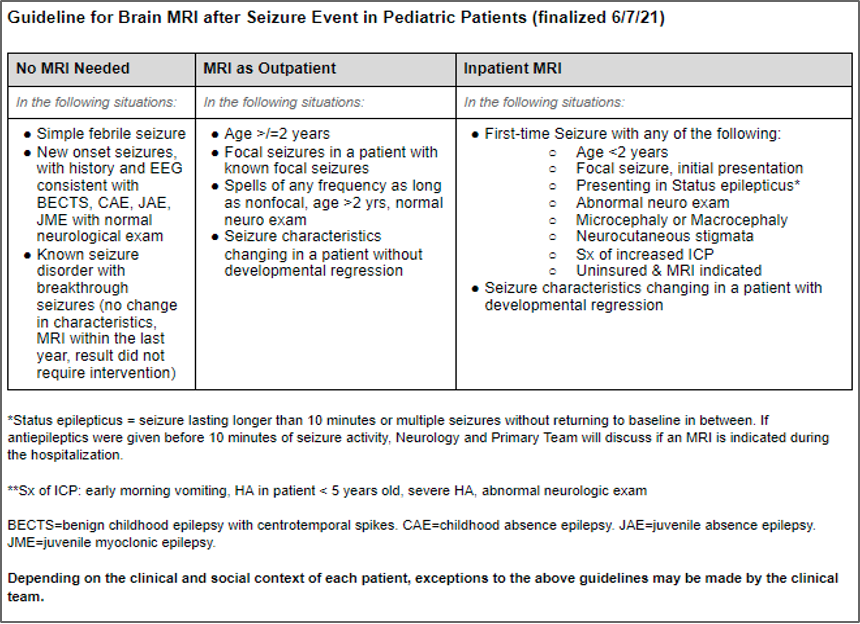 Figure 1: Brain MRI ordering guidelines for pediatric patients presenting after a seizure or seizure-like episode.
Figure 1: Brain MRI ordering guidelines for pediatric patients presenting after a seizure or seizure-like episode.Work Flow Process Map
 Work flow process map
Work flow process map