Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Education/Research/QI Potpourri
320 - The Effect of a Brief Medical Huddle Prior to Rounds on the Patient and Family Experience with Inpatient Physician Communication
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 320
Publication Number: 320.322
Publication Number: 320.322
Rachel R. Osborn, Yale University School of Medicine, New Haven, CT, United States; Henna S. Boolchandani, Yale-New Haven Children's Hospital, New Haven, CT, United States; Aaron Bennett, Yale New Haven Children’s Hospital, Philadelphia, PA, United States; Rebecca Beagan, Yale School of Medicine, New Haven, CT, United States; Nirali Butala, Yale New Haven, New Haven, CT, United States; Jessica Malcolm, Yale-New Haven Children's Hospital, New Haven, CT, United States; Heather Collette, Yale School of Medicine, New Haven, CT, United States

Rachel R. Osborn, MD
Assistant Professor Pediatrics
Yale University School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background: Initial studies of Patient and Family Centered Rounds (PFCR) in pediatrics used increasing parental interest in participating as the primary indicator of success and did not include comparative data. There are mixed results of family satisfaction with the process when compared to standard rounding. To date, there is limited data examining hybrid models of rounding and communication, in which some medical information is shared amongst the interdisciplinary team prior to initiating the formal rounding process.
Objective: To assess the effect of the addition of a standardized interdisciplinary medical huddle prior to the formal family-centered rounding encounter on patient and family satisfaction with communication and experience on rounds.
Design/Methods: We utilized a quasi-experimental interrupted time series to compare family experience with rounding before and after the introduction of an interdisciplinary medical huddle preceding the PFCR encounter. Family experience was assessed utilizing a five question Likert scale survey administered by a study team member after rounds. The primary outcome measure was proportion of “top box” responses which was compared between the pre-intervention period (Feb-Jun 2017) and post intervention periods (Mar-Jul 2021). The medical huddle consisted of a brief review of overnight events and data, along with an assessment organized by problem list. Communication coaching and contingency planning were both addressed by team leaders. Both pre and post intervention periods relied on a communication checklist to guide the rounding encounter within the room (Figure 1).
Results: Proportion of top box responses in both pre and post intervention periods is shown in Table 1. Following the introduction of the medical huddle, significant improvements were noted in answers to: “the doctors used language I could understand” (27/50 in 2017 compared with 40/54 in 2021) (p=0.03), “The doctors addressed my concerns and questions” (29/50 in 2017 compared with 43/53 in 2021) (p=0.02) and “I felt comfortable raising questions or concerns” (23/50 in 2017 compared with 42/54 in 2021) (p=0.008). Overall top box response in aggregate was 56% in the pre-intervention period compared with 76% in the post-intervention period (pConclusion(s): Utilizing a pre-rounds medical huddle in real time significantly improved family experience on rounds in the general inpatient setting. The focus of developing a shared understanding for all team members, as well as communication planning, likely contributed to these results.
Figure 1: Standard Script for PFCR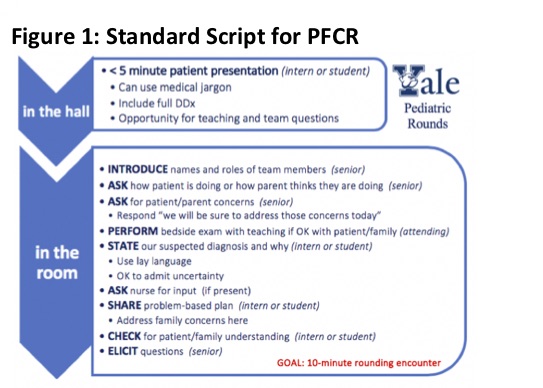 This card guided physician team communication with family. "In the room" had nearly identical wording in the pre and post intervention periods, excepting a substitution of "state our suspected diagnosis and why" in place of "present the history and assessment."
This card guided physician team communication with family. "In the room" had nearly identical wording in the pre and post intervention periods, excepting a substitution of "state our suspected diagnosis and why" in place of "present the history and assessment."
Table 1: Percent of Top Box Reponse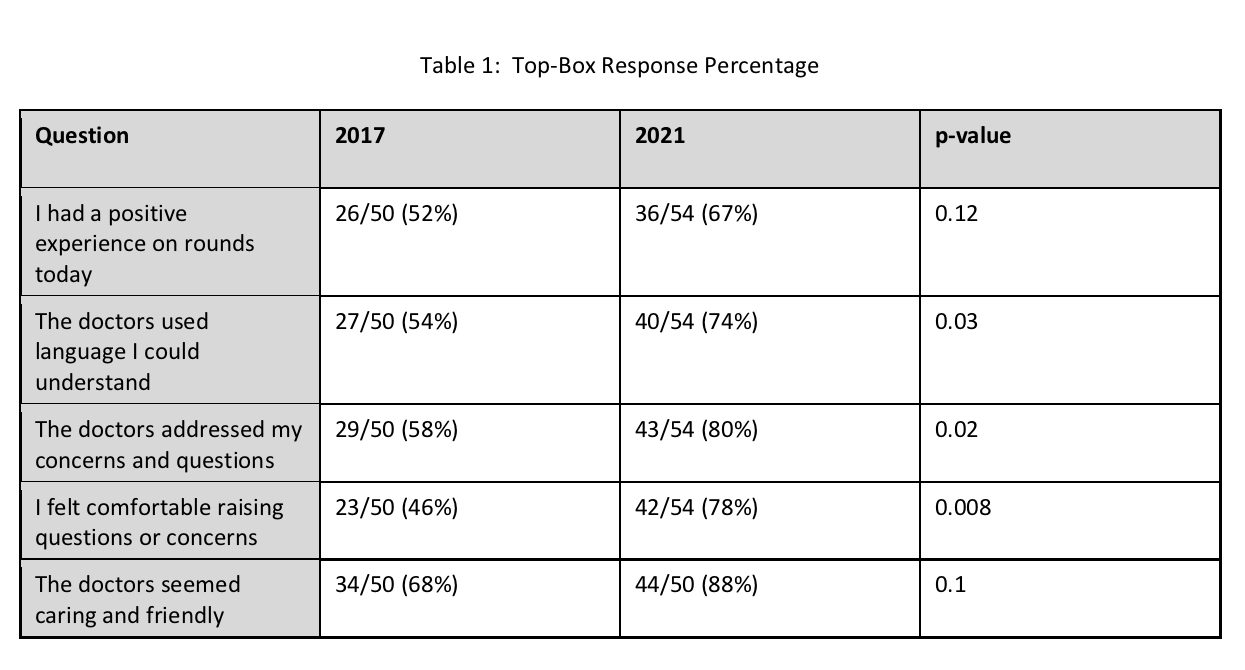 Proportion of responses in the "strongly agree" category acrosss all 5 Likert questions is shown here
Proportion of responses in the "strongly agree" category acrosss all 5 Likert questions is shown here
Objective: To assess the effect of the addition of a standardized interdisciplinary medical huddle prior to the formal family-centered rounding encounter on patient and family satisfaction with communication and experience on rounds.
Design/Methods: We utilized a quasi-experimental interrupted time series to compare family experience with rounding before and after the introduction of an interdisciplinary medical huddle preceding the PFCR encounter. Family experience was assessed utilizing a five question Likert scale survey administered by a study team member after rounds. The primary outcome measure was proportion of “top box” responses which was compared between the pre-intervention period (Feb-Jun 2017) and post intervention periods (Mar-Jul 2021). The medical huddle consisted of a brief review of overnight events and data, along with an assessment organized by problem list. Communication coaching and contingency planning were both addressed by team leaders. Both pre and post intervention periods relied on a communication checklist to guide the rounding encounter within the room (Figure 1).
Results: Proportion of top box responses in both pre and post intervention periods is shown in Table 1. Following the introduction of the medical huddle, significant improvements were noted in answers to: “the doctors used language I could understand” (27/50 in 2017 compared with 40/54 in 2021) (p=0.03), “The doctors addressed my concerns and questions” (29/50 in 2017 compared with 43/53 in 2021) (p=0.02) and “I felt comfortable raising questions or concerns” (23/50 in 2017 compared with 42/54 in 2021) (p=0.008). Overall top box response in aggregate was 56% in the pre-intervention period compared with 76% in the post-intervention period (pConclusion(s): Utilizing a pre-rounds medical huddle in real time significantly improved family experience on rounds in the general inpatient setting. The focus of developing a shared understanding for all team members, as well as communication planning, likely contributed to these results.
Figure 1: Standard Script for PFCR
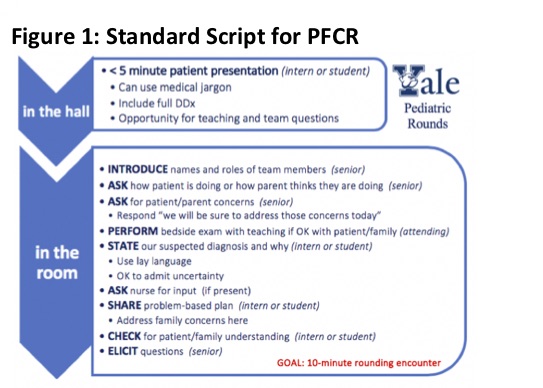 This card guided physician team communication with family. "In the room" had nearly identical wording in the pre and post intervention periods, excepting a substitution of "state our suspected diagnosis and why" in place of "present the history and assessment."
This card guided physician team communication with family. "In the room" had nearly identical wording in the pre and post intervention periods, excepting a substitution of "state our suspected diagnosis and why" in place of "present the history and assessment."Table 1: Percent of Top Box Reponse
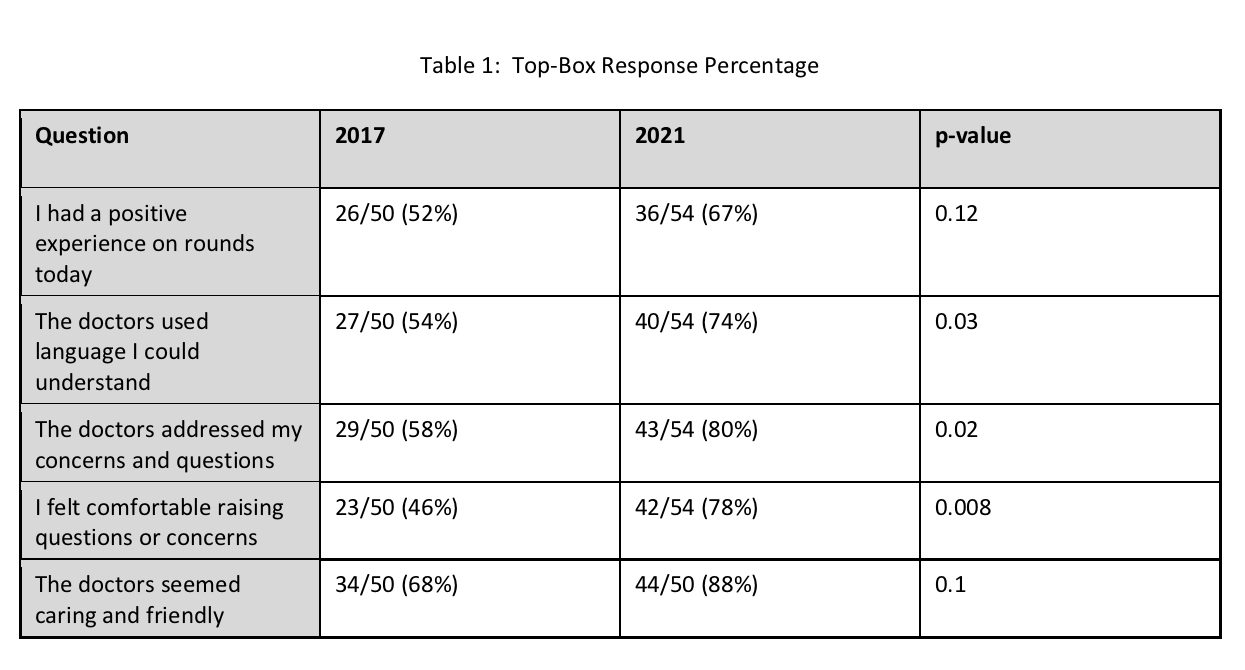 Proportion of responses in the "strongly agree" category acrosss all 5 Likert questions is shown here
Proportion of responses in the "strongly agree" category acrosss all 5 Likert questions is shown here