Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VIII
367 - The influence of hospital pediatric inpatient capabilities on an emergency department’s weighted pediatric readiness score
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 367
Publication Number: 367.313
Publication Number: 367.313
Jonathan R. Eisenberg, University of Utah, SALT LAKE CITY, UT, United States; Kristina Brumme, University of Colorado School of Medicine, Lincoln, MA, United States; Rachel Codden, University of Utah, Salt Lake City, UT, United States; Katherine E. Remick, University of Texas at Austin Dell Medical School, Austin, TX, United States; Hilary Hewes, University of Utah School of Medicine, Salt Lake City, UT, United States

Jonathan Eisenberg, MD (he/him/his)
PEM fellow
Dell Children's Medical Center of Central Texas
Austin, Texas, United States
Presenting Author(s)
Background: The majority of ill and injured pediatric patients are initially treated at non-pediatric specialty emergency departments (ED). The 2013 National Pediatric Readiness Project (NPRP) evaluated the presence of essential pediatric-specific elements in an ED, producing a weighted pediatric readiness score (wPRS) to quantify an ED’s pediatric readiness.
Objective: This study seeks to examine the relationships between pediatric inpatient capabilities and the wPRS, including associations with pediatric inpatient unit types.
Design/Methods: This is a retrospective cross-sectional cohort study with secondary analysis of the 2013 NPRP assessment of 5,017 EDs in the US. Resultant wPRS were compared to individual hospital pediatric inpatient capabilities (newborn nursery, neonatal and pediatric intensive care, pediatric ward, and adult ward accepting pediatric patients) and ED structure. A linear regression analysis was performed to determine the relationship between individual pediatric inpatient capabilities including ED structure, cumulative pediatric inpatient capabilities and wPRS.
Results: Of the 4149 responding EDs, 4146 were included in our analysis. The largest sub-group (n=1797) were non-children’s hospitals, without a pediatric ED (PED) but with more than one pediatric inpatient capability (mean WPRS 59.4). Hospitals with a PED and at least one pediatric inpatient capability scored highest (mean WPRS 78.4). In hospitals reporting all inpatient capabilities (nursery, NICU, pediatric ward and PICU) without a PED, the mean score was 67.5. In the unadjusted linear regression, all pediatric inpatient units were additive to final score (P < 0.001) with presence of a PICU having the greatest effect (13.5 pts, P< 0.001).Conclusion(s): Our data demonstrate that hospitals whose infrastructure include a dedicated PED and at least one pediatric inpatient capability are more likely to have an ED with a higher WPRS. The wPRS decreases significantly in the absence of PED space and/or any pediatric inpatient capability. The cumulative effect of multiple pediatric inpatient units in the absence of a PED did not exceed the mean wPRS of EDs in hospitals having at least one pediatric inpatient unit and a separate PED. Engagement of hospital-wide staff to support pediatric readiness in every ED could be an important step to optimize initial stabilization of critically ill and injured children in non-pediatric EDs, especially in rural and remote access sites.
Jonathan Eisenberg MD CVjecv.pdf
Table 1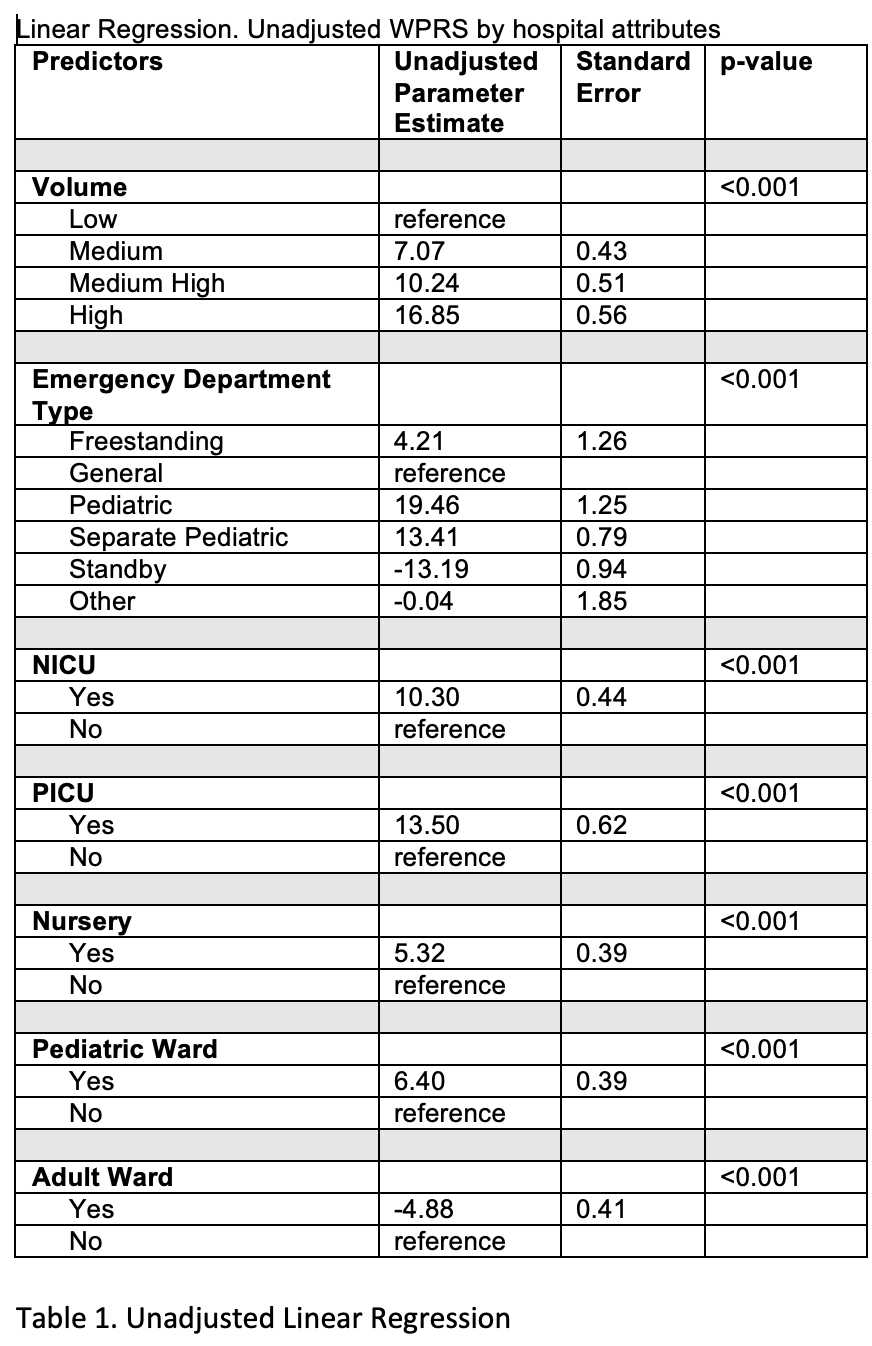 Unadjusted Linear Regression
Unadjusted Linear Regression
Objective: This study seeks to examine the relationships between pediatric inpatient capabilities and the wPRS, including associations with pediatric inpatient unit types.
Design/Methods: This is a retrospective cross-sectional cohort study with secondary analysis of the 2013 NPRP assessment of 5,017 EDs in the US. Resultant wPRS were compared to individual hospital pediatric inpatient capabilities (newborn nursery, neonatal and pediatric intensive care, pediatric ward, and adult ward accepting pediatric patients) and ED structure. A linear regression analysis was performed to determine the relationship between individual pediatric inpatient capabilities including ED structure, cumulative pediatric inpatient capabilities and wPRS.
Results: Of the 4149 responding EDs, 4146 were included in our analysis. The largest sub-group (n=1797) were non-children’s hospitals, without a pediatric ED (PED) but with more than one pediatric inpatient capability (mean WPRS 59.4). Hospitals with a PED and at least one pediatric inpatient capability scored highest (mean WPRS 78.4). In hospitals reporting all inpatient capabilities (nursery, NICU, pediatric ward and PICU) without a PED, the mean score was 67.5. In the unadjusted linear regression, all pediatric inpatient units were additive to final score (P < 0.001) with presence of a PICU having the greatest effect (13.5 pts, P< 0.001).Conclusion(s): Our data demonstrate that hospitals whose infrastructure include a dedicated PED and at least one pediatric inpatient capability are more likely to have an ED with a higher WPRS. The wPRS decreases significantly in the absence of PED space and/or any pediatric inpatient capability. The cumulative effect of multiple pediatric inpatient units in the absence of a PED did not exceed the mean wPRS of EDs in hospitals having at least one pediatric inpatient unit and a separate PED. Engagement of hospital-wide staff to support pediatric readiness in every ED could be an important step to optimize initial stabilization of critically ill and injured children in non-pediatric EDs, especially in rural and remote access sites.
Jonathan Eisenberg MD CVjecv.pdf
Table 1
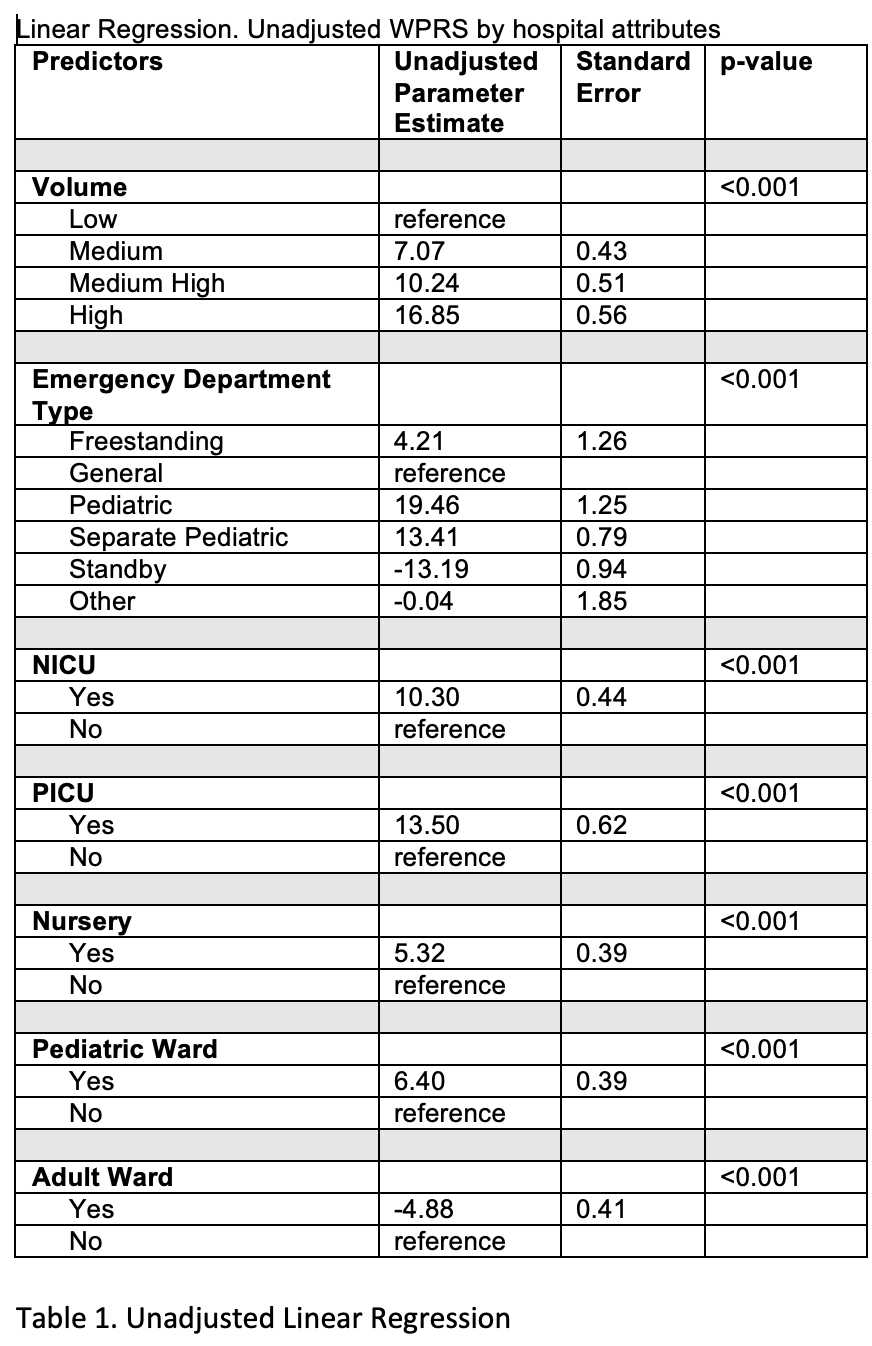 Unadjusted Linear Regression
Unadjusted Linear Regression