Clinical Bioethics
Category: Abstract Submission
Clinical Bioethics
615 - The Role of Resource Utilization in the Ethical Debate of Offering Neonatal Resuscitation During the 22nd Week of Gestation
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 615
Publication Number: 615.306
Publication Number: 615.306
Allison Schuh, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Samantha Millikan, University of Chicago Medical Center, Chicago, IL, United States; Cameron N. Boyd, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Cassandra C. Daisy, The University of Chicago Pritzker School of Medicine, Chicago, IL, United States; Aunum Akhter, University of Michigan Medical School, Ann Arbor, MI, United States; Naomi T. Laventhal, University of Michigan Medical School, Ann Arbor, MI, United States; Danielle LoRe, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Kathleen G. Brennan, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Catherine M. Groden, Indiana University School of Medicine, Indianapolis, IN, United States; Jasmine Soo, Indiana University School of Medicine, Indianapolis, IN, United States; Shelley Hoffman, Indiana University School of Medicine, Indianapolis, IN, United States; Brownsyne Tucker Edmonds, Indiana University School of Medicine, Department Of Ob/Gyn, Indianapolis, IN, United States; Tiffany Tonismae, Johns Hopkins All Children's Hospital, Tampa, FL, United States; Sanela Andelija, HCA Healthcare/USF Morsani College of Medicine GME Programs, Brandon Regional Hospital, Brandon, FL, United States; Richard Kampanatkosol, Advocate Children's Hospital - Oak Lawn, Oak Lawn, IL, United States; Maggie M. Vogel, Advocate Children's Hospital - Oak Lawn, Oak Lawn, IL, United States; Christine Carlos, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States; Dalia M. Feltman, NorthShore University HealthSystem Evanston Hospital, Burr Ridge, IL, United States; Bree Andrews, University of Chicago Division of the Biological Sciences The Pritzker School of Medicine, Chicago, IL, United States
- AS
Allison Schuh, MD
Neonatal/Perinatal Medicine Fellow
Comer Children's Hospital at University of Chicago Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Variation in attitudes and practices of offering resuscitation to infants born at the margin of viability between 22-24 weeks’ gestational age (GA) has been extensively described. While resuscitation near the upper end of this GA range is now widely offered, recent ethical debate is centered on whether to offer active resuscitation (AR) in the 22nd week. One facet of this debate is the relative cost of providing care to those born at 22 weeks’ GA.
Objective: To evaluate practice change over time for mothers and their infants inborn at 22, 23, and 24 weeks’ GA with respect to NICU resource utilization and infant outcomes at 15 study centers over two epochs.
Design/Methods: This is a retrospective cohort study comprised of mothers and their infants delivered between 22 0/7 and 24 6/7 weeks’ GA at tertiary care centers which are part of the INDEED (Investigating Neonatal Decisions for Extremely Early Deliveries) study group; the cohort will ultimately include data from 15 centers over a 10 year period, divided into two epochs. NICU length of stay (LOS) was utilized as a proxy measure for cost of care. Chi-square and ANOVA were used to compare perinatal interventions and LOS.
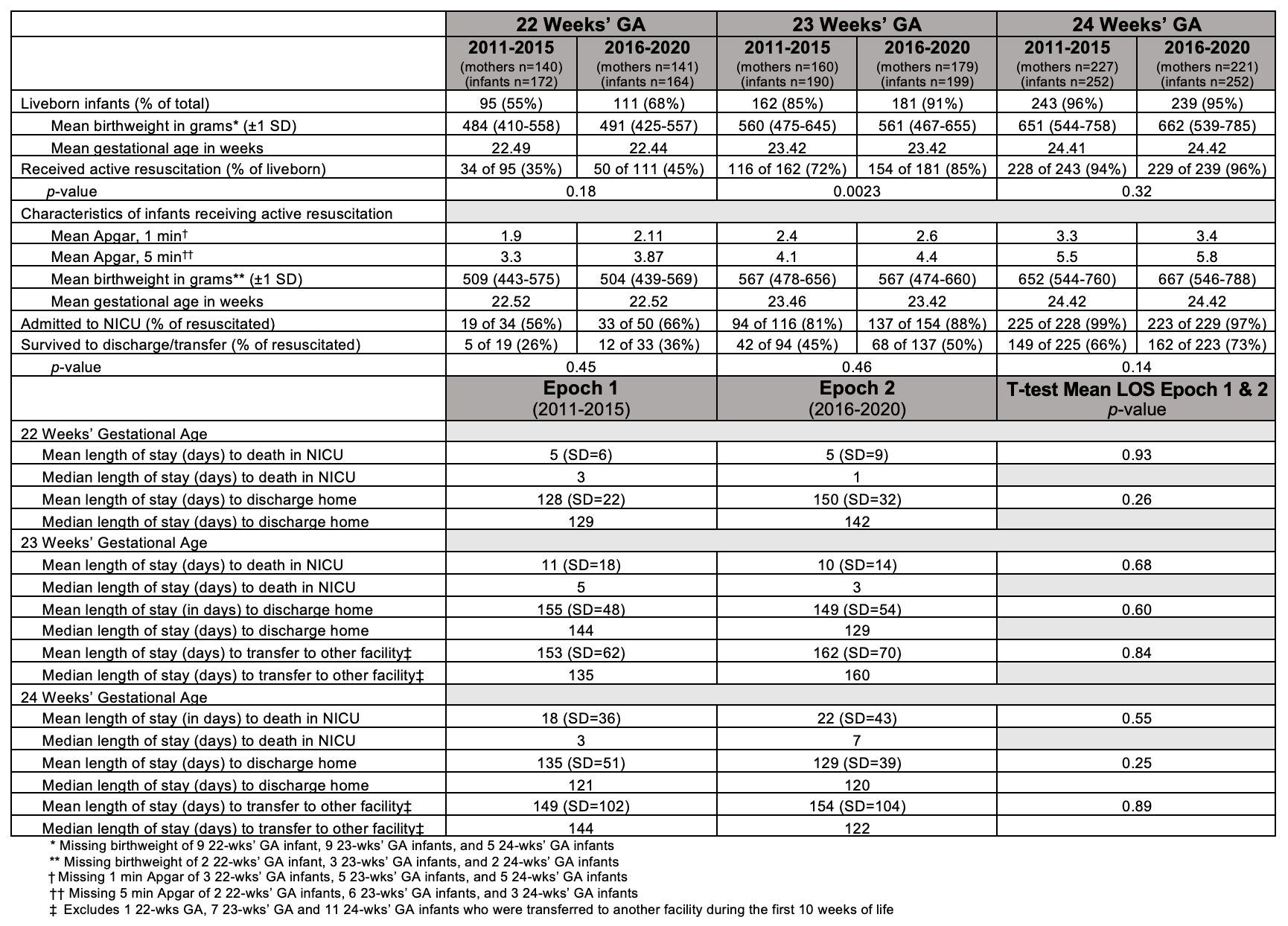
Results: Epoch 1 and 2 cohorts included 7 centers with 527 and 541 mothers, and 614 and 615 infants, respectively. Antenatal corticosteroid use increased at 22 and 23 weeks’ GA between epochs (11 vs 26% and 58 vs 82%, respectively). The rate of AR at 22 and 23 weeks’ GA also increased (35 vs 45% and 72 vs 85%, respectively). There was a trend toward increased survival among all GA groups between epochs (Table 1 and 2). Figures 1 and 2 report LOS to disposition of death in the NICU, NICU discharge, or transfer to a long-term care facility in Epochs 1 and 2. The mean LOS of all non-surviving 22, 23 & 24 week infants was 15 vs 14 days and the mean LOS of all surviving 22, 23 & 24 week infants was 141 vs 139 days in Epoch 1 and 2, respectively. LOS did not differ statistically between GA cohorts for those who died in the NICU or those who were discharged from the NICU within or between Epoch 1 and 2. In Epoch 2, the total mean LOS was significantly less for 22 week infants than for 23 and 24 week infants, reflective of the short NICU LOS at this GA for non-survivors.Conclusion(s): We identified an increase in AR at 22 and 23 weeks' GA, with a trend toward increased survival, over the last decade. Importantly, this AR increase was not accompanied by an increase in LOS to discharge or death, suggesting that disproportionate NICU resource utilization is not a justice-based argument to persuade against offering AR at the margin of viability.
Table 1: Population Characteristics and Antenatal Interventions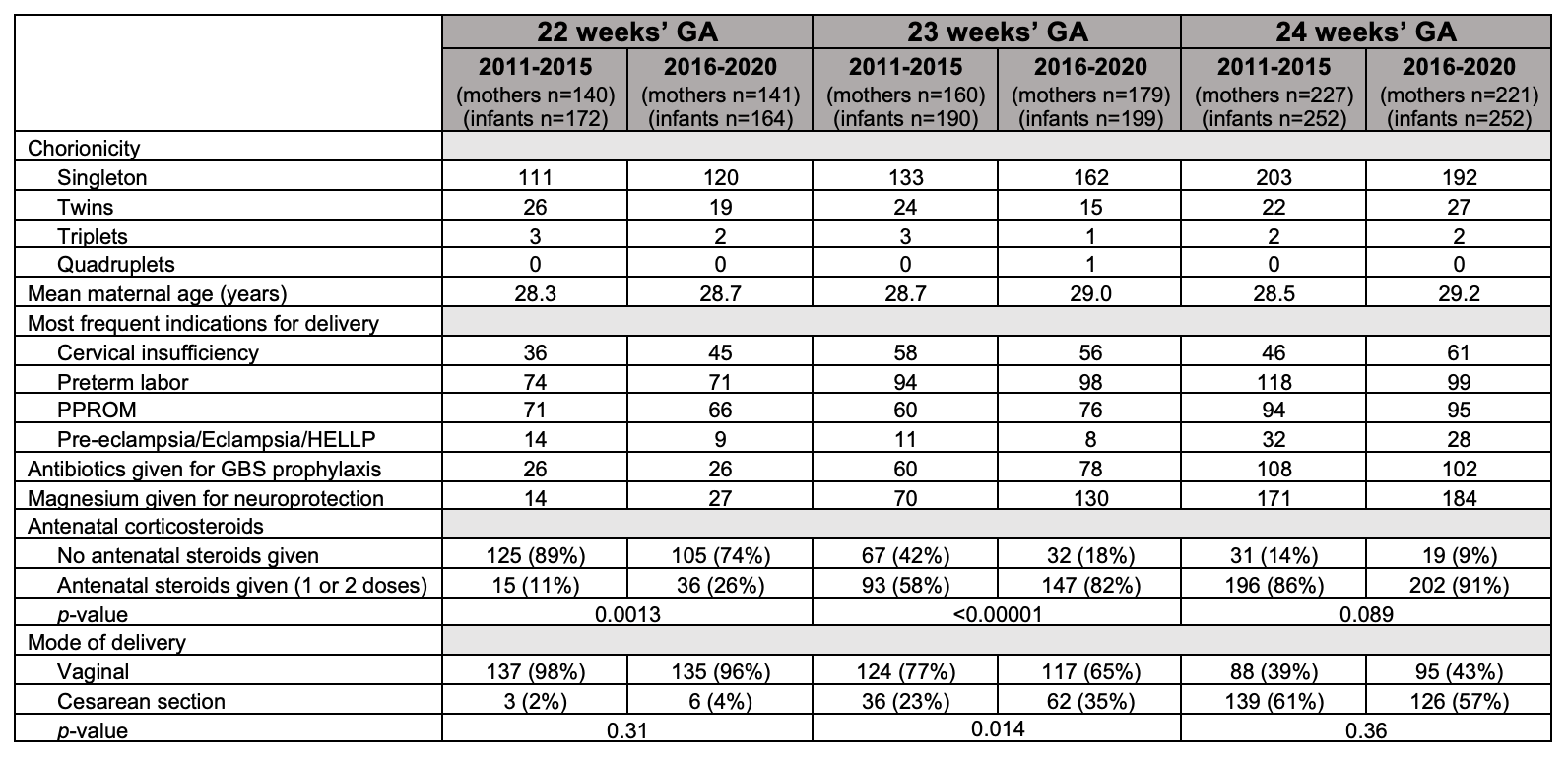
Table 2: Infant Outcomes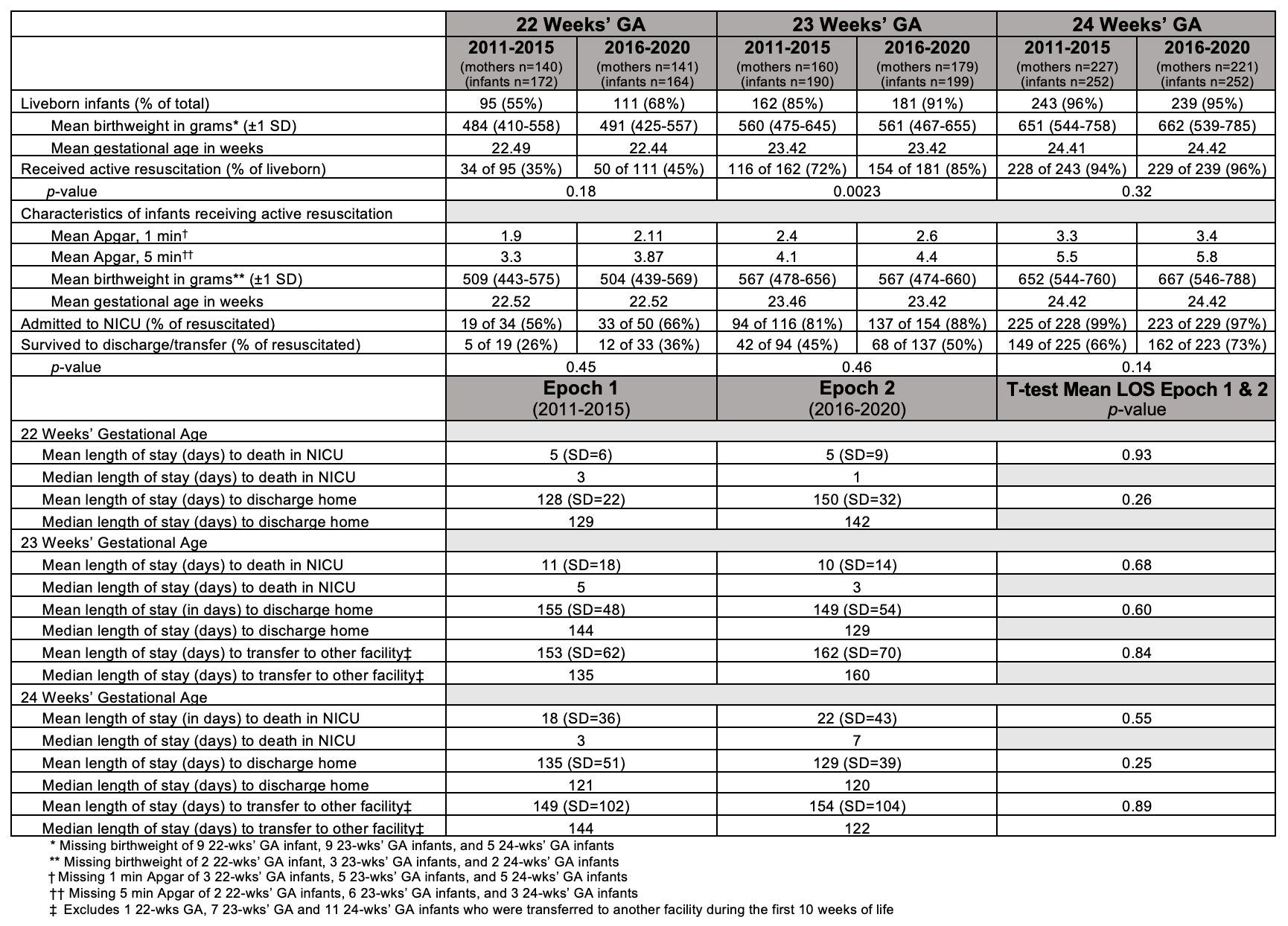
Objective: To evaluate practice change over time for mothers and their infants inborn at 22, 23, and 24 weeks’ GA with respect to NICU resource utilization and infant outcomes at 15 study centers over two epochs.
Design/Methods: This is a retrospective cohort study comprised of mothers and their infants delivered between 22 0/7 and 24 6/7 weeks’ GA at tertiary care centers which are part of the INDEED (Investigating Neonatal Decisions for Extremely Early Deliveries) study group; the cohort will ultimately include data from 15 centers over a 10 year period, divided into two epochs. NICU length of stay (LOS) was utilized as a proxy measure for cost of care. Chi-square and ANOVA were used to compare perinatal interventions and LOS.
Results: Epoch 1 and 2 cohorts included 7 centers with 527 and 541 mothers, and 614 and 615 infants, respectively. Antenatal corticosteroid use increased at 22 and 23 weeks’ GA between epochs (11 vs 26% and 58 vs 82%, respectively). The rate of AR at 22 and 23 weeks’ GA also increased (35 vs 45% and 72 vs 85%, respectively). There was a trend toward increased survival among all GA groups between epochs (Table 1 and 2). Figures 1 and 2 report LOS to disposition of death in the NICU, NICU discharge, or transfer to a long-term care facility in Epochs 1 and 2. The mean LOS of all non-surviving 22, 23 & 24 week infants was 15 vs 14 days and the mean LOS of all surviving 22, 23 & 24 week infants was 141 vs 139 days in Epoch 1 and 2, respectively. LOS did not differ statistically between GA cohorts for those who died in the NICU or those who were discharged from the NICU within or between Epoch 1 and 2. In Epoch 2, the total mean LOS was significantly less for 22 week infants than for 23 and 24 week infants, reflective of the short NICU LOS at this GA for non-survivors.Conclusion(s): We identified an increase in AR at 22 and 23 weeks' GA, with a trend toward increased survival, over the last decade. Importantly, this AR increase was not accompanied by an increase in LOS to discharge or death, suggesting that disproportionate NICU resource utilization is not a justice-based argument to persuade against offering AR at the margin of viability.
Table 1: Population Characteristics and Antenatal Interventions
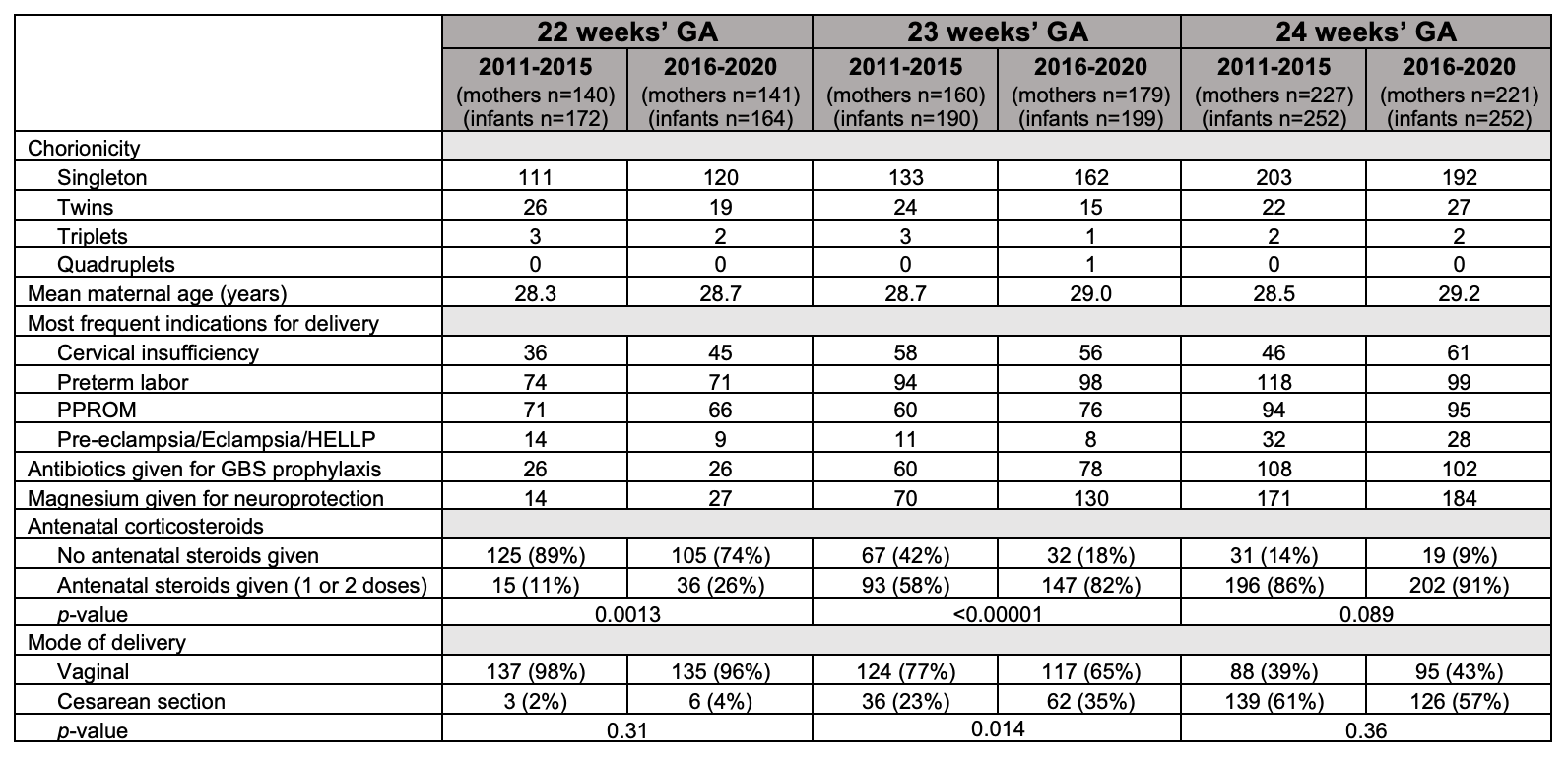
Table 2: Infant Outcomes