Nephrology: Clinical
Category: Abstract Submission
Nephrology III: General Nephrology and Dialysis
57 - Timing of Acute Kidney Injury (AKI) in children receiving Extracorporeal Membrane Oxygenation (ECMO)
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 57
Publication Number: 57.340
Publication Number: 57.340
Amy Strong, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Rosanna Fulchiero, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Jarcy Zee, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Diego A. Campos, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; James Connelly, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Todd J. Kilbaugh, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Benjamin L. Laskin, Childrens Hospital of Philadelphia, Bala Cynwyd, PA, United States; Michelle Denburg, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Amy Strong, MD
Fellow Physician
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The risk of AKI is high in ECMO recipients. Few studies have considered the presence of AKI at ECMO initiation and evaluated the impact of demographic and disease-related characteristics on the development and timing of AKI for children while undergoing ECMO.
Objective: To evaluate the incidence and timing of AKI in children undergoing ECMO.
Design/Methods: This retrospective cohort study included patients treated with ECMO at a single pediatric center from January 2009-December 2019. AKI was evaluated both at and post-ECMO initiation using KDIGO criteria with the creatinine drawn closest to the start of ECMO as the baseline. The baseline creatinine was compared to standard values for age and sex to define AKI at ECMO start. Multivariable cause-specific Cox proportional hazards regression models were used to assess whether age, sex, intensive care unit (ICU), and AKI at ECMO start were risk factors for both the outcomes of AKI post-ECMO start and death. Patients were censored seven days following ECMO discontinuation for both outcomes. Death was considered a competing risk for the AKI outcome, and AKI post-ECMO start was included as a time-varying covariate when mortality was examined.
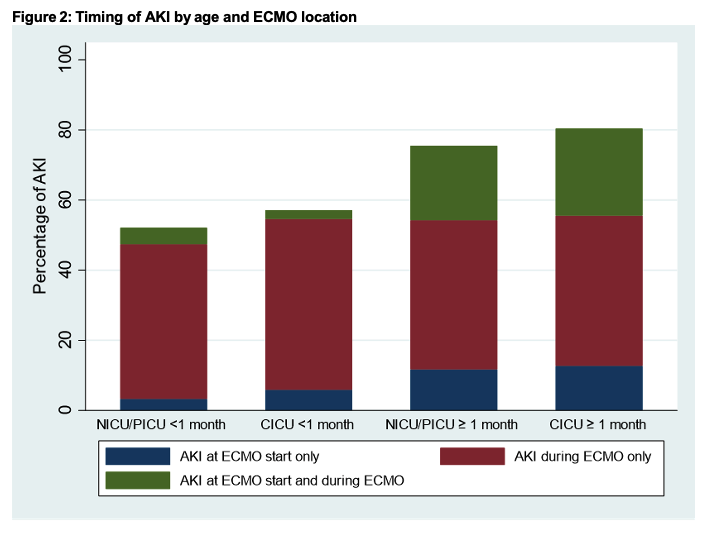
Results: 685 ECMO runs were identified, of which 615 ECMO runs from 601 unique patients had available creatinine data and were included (Table 1). AKI at ECMO initiation was present in 21%, while 57% met criteria for AKI post-ECMO start. The incidence and timing of AKI varied by age and unit (Figure 2). Patients receiving ECMO in the pediatric or cardiac ICUs had a higher risk for AKI and death when compared to neonatal ICU patients. AKI at ECMO start did not significantly increase the risk of developing AKI post-ECMO start. AKI post-ECMO start significantly increased the hazard of death (Table 3). Conclusion(s): AKI occurred more commonly post-ECMO initiation than was present at the start of ECMO. Patients who underwent ECMO in the pediatric or cardiac ICUs had a higher risk of AKI on ECMO as well as a higher risk of death when compared to the neonatal ICU. The presence of AKI after ECMO initiation significantly decreased survival.
Table 1: Baseline Demographics and ECMO characteristics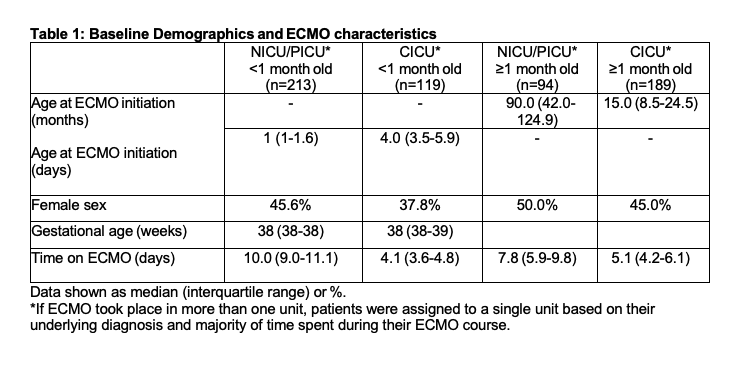
Figure 2: Timing of AKI by age and ECMO location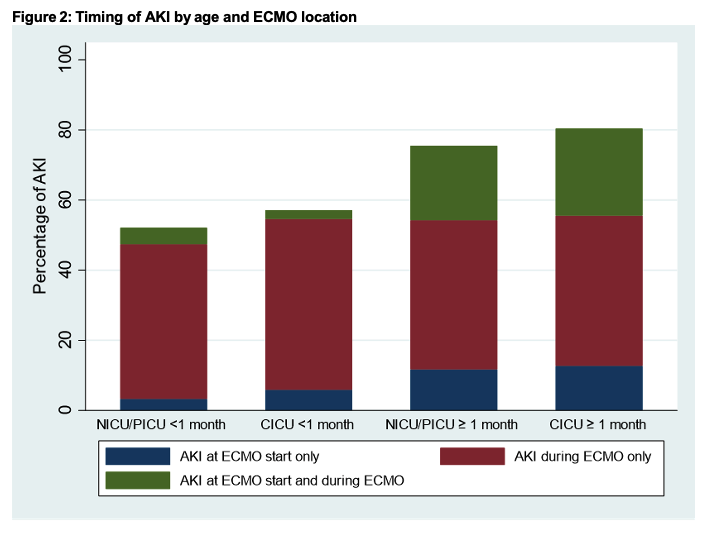
Objective: To evaluate the incidence and timing of AKI in children undergoing ECMO.
Design/Methods: This retrospective cohort study included patients treated with ECMO at a single pediatric center from January 2009-December 2019. AKI was evaluated both at and post-ECMO initiation using KDIGO criteria with the creatinine drawn closest to the start of ECMO as the baseline. The baseline creatinine was compared to standard values for age and sex to define AKI at ECMO start. Multivariable cause-specific Cox proportional hazards regression models were used to assess whether age, sex, intensive care unit (ICU), and AKI at ECMO start were risk factors for both the outcomes of AKI post-ECMO start and death. Patients were censored seven days following ECMO discontinuation for both outcomes. Death was considered a competing risk for the AKI outcome, and AKI post-ECMO start was included as a time-varying covariate when mortality was examined.
Results: 685 ECMO runs were identified, of which 615 ECMO runs from 601 unique patients had available creatinine data and were included (Table 1). AKI at ECMO initiation was present in 21%, while 57% met criteria for AKI post-ECMO start. The incidence and timing of AKI varied by age and unit (Figure 2). Patients receiving ECMO in the pediatric or cardiac ICUs had a higher risk for AKI and death when compared to neonatal ICU patients. AKI at ECMO start did not significantly increase the risk of developing AKI post-ECMO start. AKI post-ECMO start significantly increased the hazard of death (Table 3). Conclusion(s): AKI occurred more commonly post-ECMO initiation than was present at the start of ECMO. Patients who underwent ECMO in the pediatric or cardiac ICUs had a higher risk of AKI on ECMO as well as a higher risk of death when compared to the neonatal ICU. The presence of AKI after ECMO initiation significantly decreased survival.
Table 1: Baseline Demographics and ECMO characteristics
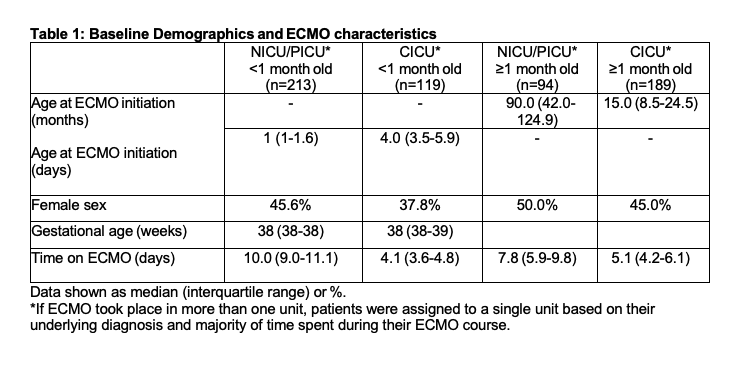
Figure 2: Timing of AKI by age and ECMO location