Back
Clinical Bioethics
Category: Abstract Submission
Clinical Bioethics
617 - Using Qualitative Methods and Concrete Tools to Map Antenatal Consultations for Extreme Prematurity and Complex Anomalies
Sunday, April 24, 2022
3:30 PM – 6:00 PM US MT
Poster Number: 617
Publication Number: 617.306
Publication Number: 617.306
Mary A. Reinoehl, University of Michigan, Ann Arbor, MI, United States; Marin Arnolds, University of Michigan Medical School, Ann Arbor, MI, United States
- MR
Mary A. Reinoehl, D.O.
Neonatal-Perinatal Medicine Fellow Physician
University of Michigan
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Pediatric professional societies recommend physicians engage in the process of shared decision making with families facing extremely preterm delivery or the birth of an infant with serious fetal anomalies. In these complex clinical scenarios where outcomes are uncertain and several ethically appropriate options for treatment exist, neonatologists must share relevant clinical data as well as elicit important information from families regarding values, goals, and experiences in a bi-directional exchange of information.
Objective: To explore and characterize the content of antenatal consultations using qualitative analysis in extremely preterm infants 27 weeks and infants with severe anomalies where palliative care at delivery was being considered.
Design/Methods: Antenatal consults were audiotaped, transcribed verbatim and coded for content using a modified Roter Interaction Analysis System (RIAS). Parents completed a survey post-consultation which aimed to measure satisfaction and understanding of the consultation on a 5-point likert scale. Patients were recruited from 2 centers.
Results: 21 consultations for extreme prematurity and 2 consultations for fetal anomalies were audiotaped and analyzed with enrollment ongoing (Table 1). Nineteen (82%) of parents completed follow up surveys. In all preterm consultations 27 weeks, physicians spoke the majority of the time (87% +/- 9%) followed by mothers (10% +/- 9%), with a trend toward more parent participation in consults for fetal anomalies (Figure 1). Across all consultation groups and centers physicians spend most of their time within two RIAS categories: biomedical topics and orientation, whereas parent speech was overall more variable and balanced in content amongst groups (Figure 2). In the < 25 weeks gestation and fetal anomaly groups where decision-making was indicated, physicians spent increased time on partnership building and psychosocial topics (Figure 2). Parents expressed high levels of satisfaction with 100% of participating parents agreeing/strongly agreeing that they were satisfied with the consultation in follow up surveys, although only 66% correctly perceived whether a decision needed to be made during the consultation. Conclusion(s): Antenatal consultations were unbalanced both in subject content and share of speaking time between physicians and parents. Families expressed satisfaction with consultations but there was a heavy reliance on discussion of “biomedical topics” amongst physicians and a missed opportunity for engaging families in discussions regarding goals and values.
Table 1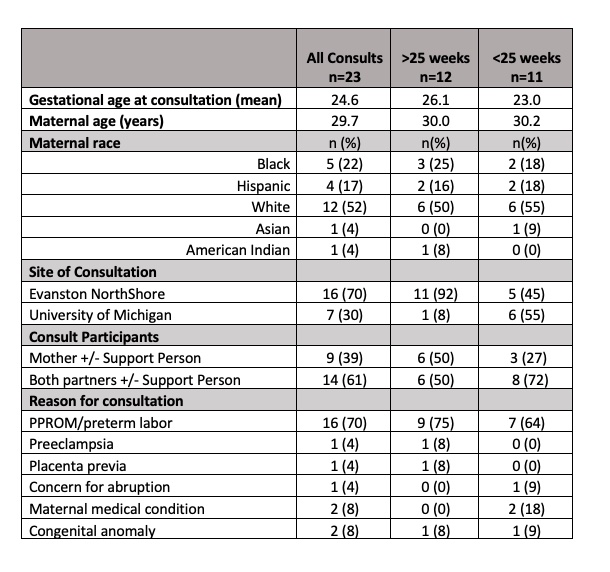 Demographics
Demographics
Figure 1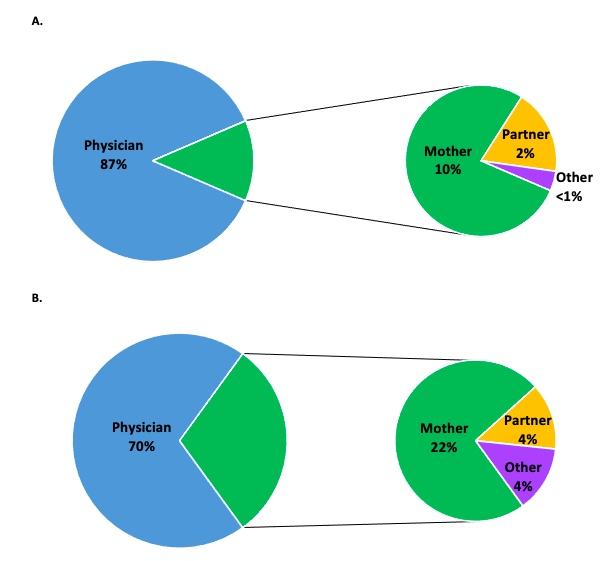 Percentage of time participants spend talking during consultations (A) preterm < 27 weeks (B) congenital anomalies
Percentage of time participants spend talking during consultations (A) preterm < 27 weeks (B) congenital anomalies
Objective: To explore and characterize the content of antenatal consultations using qualitative analysis in extremely preterm infants 27 weeks and infants with severe anomalies where palliative care at delivery was being considered.
Design/Methods: Antenatal consults were audiotaped, transcribed verbatim and coded for content using a modified Roter Interaction Analysis System (RIAS). Parents completed a survey post-consultation which aimed to measure satisfaction and understanding of the consultation on a 5-point likert scale. Patients were recruited from 2 centers.
Results: 21 consultations for extreme prematurity and 2 consultations for fetal anomalies were audiotaped and analyzed with enrollment ongoing (Table 1). Nineteen (82%) of parents completed follow up surveys. In all preterm consultations 27 weeks, physicians spoke the majority of the time (87% +/- 9%) followed by mothers (10% +/- 9%), with a trend toward more parent participation in consults for fetal anomalies (Figure 1). Across all consultation groups and centers physicians spend most of their time within two RIAS categories: biomedical topics and orientation, whereas parent speech was overall more variable and balanced in content amongst groups (Figure 2). In the < 25 weeks gestation and fetal anomaly groups where decision-making was indicated, physicians spent increased time on partnership building and psychosocial topics (Figure 2). Parents expressed high levels of satisfaction with 100% of participating parents agreeing/strongly agreeing that they were satisfied with the consultation in follow up surveys, although only 66% correctly perceived whether a decision needed to be made during the consultation. Conclusion(s): Antenatal consultations were unbalanced both in subject content and share of speaking time between physicians and parents. Families expressed satisfaction with consultations but there was a heavy reliance on discussion of “biomedical topics” amongst physicians and a missed opportunity for engaging families in discussions regarding goals and values.
Table 1
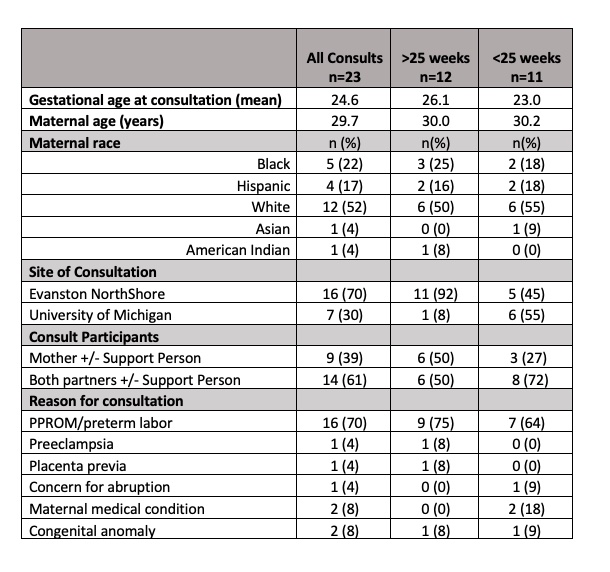 Demographics
DemographicsFigure 1
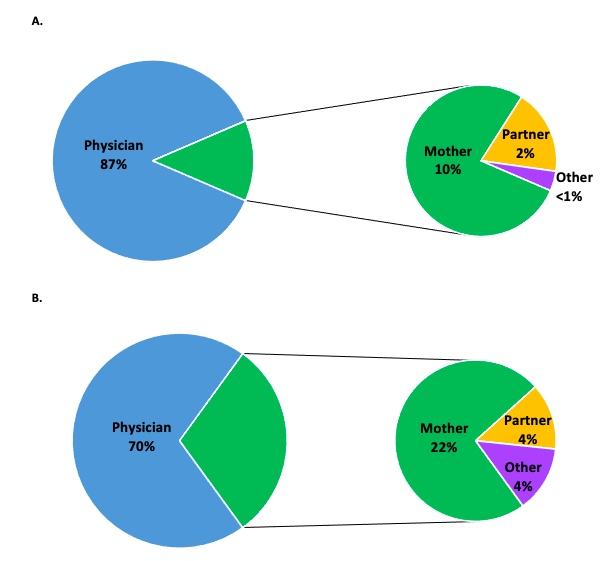 Percentage of time participants spend talking during consultations (A) preterm < 27 weeks (B) congenital anomalies
Percentage of time participants spend talking during consultations (A) preterm < 27 weeks (B) congenital anomalies