Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine X
394 - Video-enhanced Curriculum for Coaching Laryngoscopists: A Randomized Controlled Educational Intervention Study
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 394
Publication Number: 394.314
Publication Number: 394.314
Kelsey A. Miller, Boston Children's Hospital, Brookline, MA, United States; Marc Auerbach, Yale School of Medicine, Milford, CT, United States; Steven S. Bin, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Aaron Donoghue, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Benjamin T. Kerrey, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Matthew R. Mittiga, University of Colorado Boulder, Boulder, CO, United States; Gabrielle D'Ambrosi, Boston Children's Hospital, Allston, MA, United States; Michael C. Monuteaux, Boston Children's Hospital, Boston, MA, United States; Joshua Nagler, Boston Children's Hospital Division of Emergency Medicine, Brookline, MA, United States
- KM
Kelsey A. Miller, MD, EdM (she/her/hers)
Attending Physician in Pediatric Emergency Medicine
Harvard Medical School
Brookline, Massachusetts, United States
Presenting Author(s)
Background: Videolaryngoscopy allows for shared viewing during pediatric intubation attempts in the emergency department (ED). This creates a unique opportunity for training pediatric emergency medicine (PEM) physicians to become coaching larynogscopists who provide real-time feedback during intubations.
Objective: Develop and assess an online curriculum to train PEM attending physicians to recognize and correct suboptimal procedural techniques during intubation attempts.
Design/Methods: This prospective multicenter randomized controlled trial enrolled PEM attendings at 6 pediatric EDs. Participants were randomized to one of three cohorts. Cohort 1 received the study intervention - a 15-minute video-enhanced curriculum on optimal intubation technique developed through consensus of 6 PEM national airway experts (Figure 1). Cohort 2 received video recordings of intubation attempts without narration. Cohort 3 received an existing module on ventilator management without intubation videos as a control group. All content was delivered on the OPENPediatrics platform. Each cohort completed identical pre- and post-tests comprised of standardized questions asking participants to select ways to improve patient preparation, glottic visualization and endotracheal tube passage after watching actual intubation recordings. The post-test also asked about confidence in real-time coaching and utility of the module.
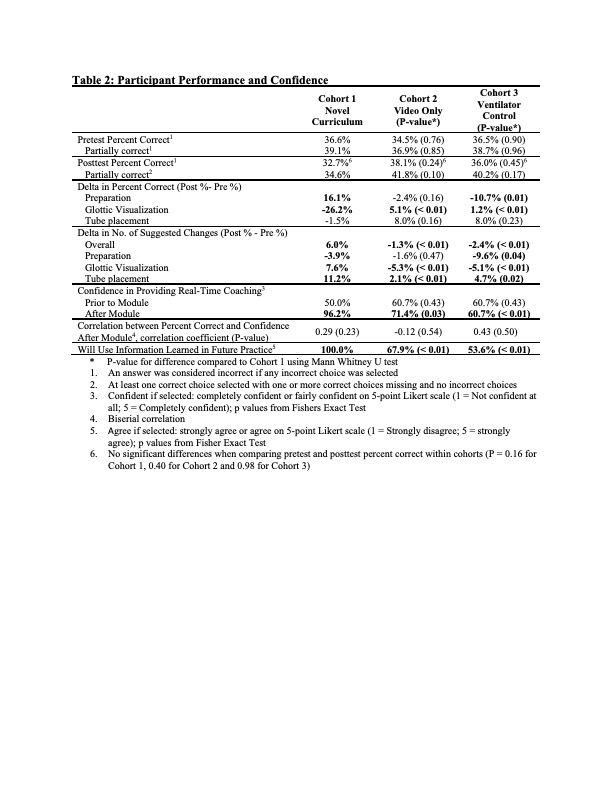
Results: Eighty-three attendings completed the curriculum (Table 1). Total percent correct did not differ between cohorts or between pre- and post-tests for any cohort (Table 2). Participants in Cohort 1 demonstrated improved performance on questions related to patient preparation but not glottic visualization or tube placement. Cohort 1 also made more suggestions for improvement, driven by increased suggestions related to glottic visualization and tube placement, and had greater increase in confidence in coaching. All participants in Cohort 1 plan to use the information learned in future practice. Confidence was not correlated with performance for any cohort.Conclusion(s): A brief novel online video-enhanced curriculum on coaching during intubation improved PEM physician identification of appropriate preparation but not glottic visualization or tube passage. Participants offered more suggestions, although not all were correct. Future efforts should evaluate how to best utilize video-enhanced approaches to maximize improvement given the perceived benefit and evidence of behavior change.
Table 1: Participant Characteristics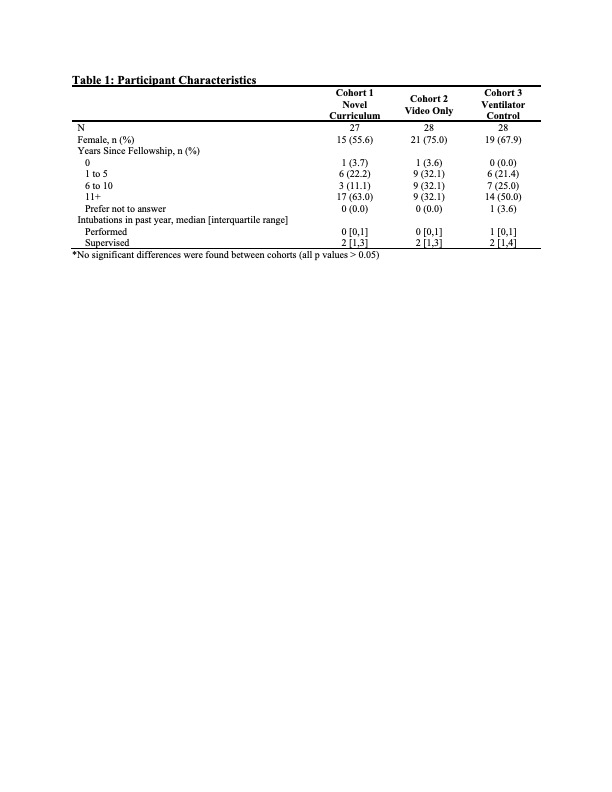
Table 2: Participant Performance and Confidence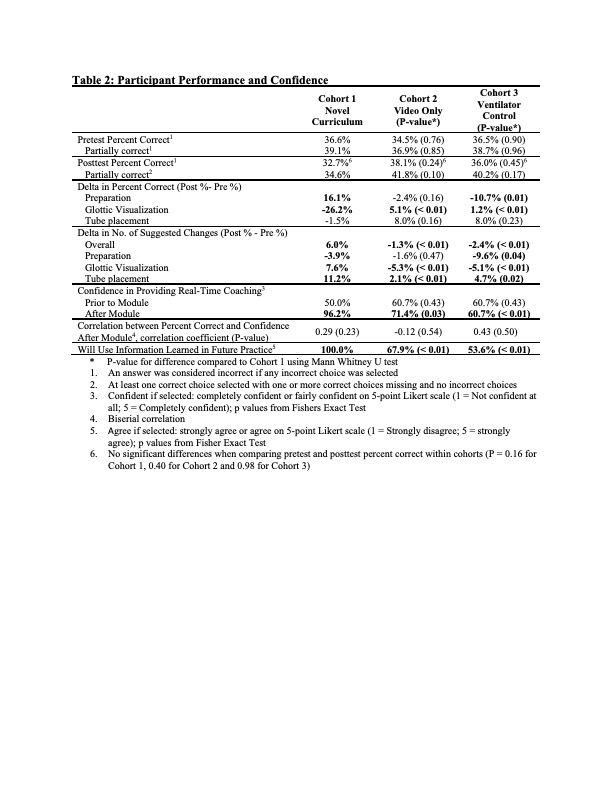
Objective: Develop and assess an online curriculum to train PEM attending physicians to recognize and correct suboptimal procedural techniques during intubation attempts.
Design/Methods: This prospective multicenter randomized controlled trial enrolled PEM attendings at 6 pediatric EDs. Participants were randomized to one of three cohorts. Cohort 1 received the study intervention - a 15-minute video-enhanced curriculum on optimal intubation technique developed through consensus of 6 PEM national airway experts (Figure 1). Cohort 2 received video recordings of intubation attempts without narration. Cohort 3 received an existing module on ventilator management without intubation videos as a control group. All content was delivered on the OPENPediatrics platform. Each cohort completed identical pre- and post-tests comprised of standardized questions asking participants to select ways to improve patient preparation, glottic visualization and endotracheal tube passage after watching actual intubation recordings. The post-test also asked about confidence in real-time coaching and utility of the module.
Results: Eighty-three attendings completed the curriculum (Table 1). Total percent correct did not differ between cohorts or between pre- and post-tests for any cohort (Table 2). Participants in Cohort 1 demonstrated improved performance on questions related to patient preparation but not glottic visualization or tube placement. Cohort 1 also made more suggestions for improvement, driven by increased suggestions related to glottic visualization and tube placement, and had greater increase in confidence in coaching. All participants in Cohort 1 plan to use the information learned in future practice. Confidence was not correlated with performance for any cohort.Conclusion(s): A brief novel online video-enhanced curriculum on coaching during intubation improved PEM physician identification of appropriate preparation but not glottic visualization or tube passage. Participants offered more suggestions, although not all were correct. Future efforts should evaluate how to best utilize video-enhanced approaches to maximize improvement given the perceived benefit and evidence of behavior change.
Table 1: Participant Characteristics
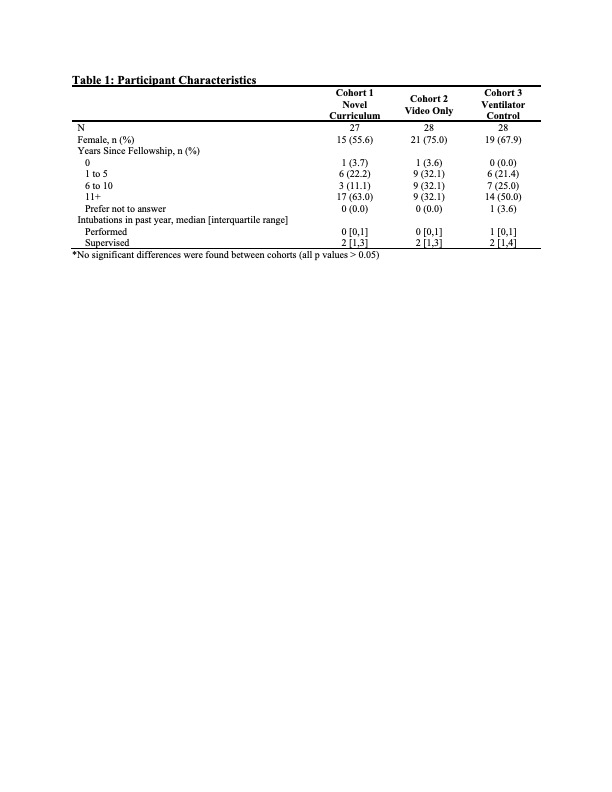
Table 2: Participant Performance and Confidence